How is pathological hyperechogenicity of the pancreas treated?
Treatment of all conditions associated with hyperechogenicity is prescribed only by a doctor.
Therapy depends on the cause of hyperechogenicity:
- In acute pancreatitis, drugs are prescribed that reduce the production of hydrochloric acid in the gastric mucosa. Agents that can reduce pancreatic enzyme activity are also needed. It must be remembered that therapy for an acute disease is carried out in the surgical department.
- For lipomatosis, a diet low in fat, especially of animal origin, is indicated.
- In the presence of calcifications and areas with fibrosis, along with the prescription of a diet, the issue of surgical intervention is decided.
- If proper nutrition and therapy for the underlying disease is necessary.
- Exacerbations of chronic pancreatitis are treated in a hospital setting. Intravenous injections and infusions are indicated.
- Treatment of carcinoma is carried out surgically; often the patient may require chemotherapy.
Proper nutrition plays a vital role in reducing pancreatic hyperechogenicity. The patient should give up fried, smoked, and salty foods.
Alcohol and smoking are strictly prohibited
It is also important to limit your consumption of sweets.
It should be remembered that increased hyperechogenicity is not a disease, but a characteristic of the organ. Based on the results of the ultrasound, appropriate treatment is prescribed. It is possible that the patient may require additional instrumental examinations and tests.
Treatment of pathological hyperechogenicity
Treatment of conditions where the echogenicity of the pancreas is increased is prescribed only by a gastroenterologist, who must find the cause of this ultrasound symptom:
- if the cause is acute pancreatitis, therapy is carried out with drugs that reduce the production of hydrochloric acid in the stomach and inhibit the enzymatic activity of the pancreas;
- if hyperechogenicity is caused by lipomatosis, a diet with a reduced amount of animal fats in the diet is prescribed;
- if the etiological factor is calcifications, fibrosis or stones in the ducts, a diet is prescribed, and the need for surgical treatment is decided;
- reactive pancreatitis requires treatment of the underlying disease and diet.
Advice! Not a single specialist proceeds from the assumption that it is necessary to treat the tests, and not the person. Increased echogenicity of the pancreas is an ultrasound symptom, not a diagnosis. It requires further examination, and therapy is prescribed only on the basis of subsequent data.
In some cases, ultrasound diagnoses increased echogenicity of the pancreas. What does the diagnosis mean, and should you panic when you see it?
What is increased echogenicity of the pancreas?
In general, the term “echogenicity” is usually understood as the ability of the tissues of certain organs to reflect an ultrasonic wave from itself, which is largely determined by their density. Echodensity is distinguished between homogeneous and heterogeneous, and the denser the organ itself, the lighter its tone on the monitor of the ultrasound machine. In the presence of liquid formations, echo negativity appears, this is due to the fact that they cannot reflect high-frequency sound, and therefore transmit it through themselves. In medical practice, pathological formations in the form of cysts with fluid inside or hemorrhages are called anechoic, but this concept also applies to some other healthy organs and their parts, for example, the intestines, gall and bladder, ventricles of the brain, heart cavities and blood vessels.
As for the pancreas (PG), it can reflect the ultrasound beam, since its structure, like the liver, has a relative density. In this regard, the images obtained during ultrasound of the two organs are almost the same: they are characterized by a light gray tone; also, when assessing the pancreas, a tone slightly lighter than that of the liver is allowed. One way or another, it is by color in a comparative aspect with the liver that experts determine the condition of the pancreas.
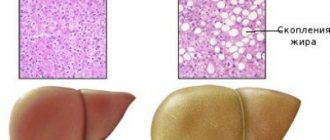
With a decrease in the volume of the glandular structures of the pancreas, which contain a large amount of fluid, echogenicity increases: healthy cells are replaced by pathologically altered cells or cells of other tissues. This phenomenon can be both local and diffuse in nature. Focal echogenicity indicates the presence of pathological formations in the organ: stones, cysts, tumors and metastases, calcifications, therefore, in order to find out the nature of the deviation in detail, further more accurate examination is necessary, for example, CT or MRI. Diffuse echogenicity is often a temporary phenomenon that occurs due to heat or fasting, elevated body temperature, or the presence of infection in the body.
Pancreatic tumors on ultrasound
In most (50-80%) cases, the tumor affects the head of the pancreas. Tumors of the head compress the common bile duct. In cancer of the pancreas, the contour of the pancreas is unclear; local enlargement or bulging of the gland is characteristic, sometimes penetrating into the surrounding tissue in the form of tongues or pseudopodia.
In most cases, a pancreatic tumor is a hypoechoic formation, almost devoid of internal echo structures. However, there are tumors with diffusely scattered echo signals and with high-intensity echo signals in the center and their absence in the periphery. Despite the fact that the boundary between the tumor and the rest of the parenchyma of the gland is unclear, it can always be approximately drawn due to the difference in the echogenicity of normal tissue and the tumor focus.
Although the hypoechoic structure of the tumor, especially in the absence of small areas of increased density in it, resembles that of cysts, the absence of the effect of distal enhancement allows us to exclude the liquid nature of the formation. In addition, cysts are characterized by a much smoother and clearer border.
| Photo. Carcinoma of the head of the pancreas (arrow): the common bile duct (A) and pancreatic duct (B) are dilated, and a hypoechoic tumor surrounds the superior mesenteric vein (C). | ||
With tumors of the head of the pancreas, the common bile and pancreatic duct is often dilated, unlike chronic pancreatitis, its walls are smooth and not compacted.
Important. Visualization of the main pancreatic duct within the hypoechoic zone is in favor of local edema and against tumor.
Sometimes, with pancreatic cancer, typical signs of chronic pancreatitis are revealed, as well as pseudocysts distal to the site of tumor obstruction. This is a consequence of obstruction. Intrahepatic metastases, enlarged celiac, periportal and retroperitoneal lymph nodes indicate cancer.
| Photo. Carcinoma of the head of the pancreas: the contour of the head is uneven due to a volumetric hypoechoic formation, the parenchyma of the body is very thin (atrophy), the pancreatic (A) and common bile (B) ducts are dilated, and there is a large round lymph node (C) at the porta hepatis. | ||
| Photo. A large lymph node (arrow) next to the pancreas may be mistaken for a tumor of the head. Enlarged mesenteric lymph nodes are round in shape, hypoechoic and without a central scar, which indicates their malignancy. | ||
| Photo. Large neuroendocrine tumor(arrows) of the pancreas with calcification and liver metastases (B). | ||
Take care of yourself, Your Diagnosticer !
All iLive content is reviewed by medical experts to ensure it is as accurate and factual as possible.
We have strict sourcing guidelines and only link to reputable sites, academic research institutions and, where possible, proven medical studies. Please note that the numbers in parentheses ([1], [2], etc.) are clickable links to such studies.
If you believe that any of our content is inaccurate, out of date, or otherwise questionable, please select it and press Ctrl + Enter.
Instrumental diagnostics using ultrasound scanning (ultrasound), also called ultrasonography, can detect areas with different acoustic densities in internal organs and cavities - hyperechoic or hypoechoic formation.
Causes
Pancreatic cells normally contain a lot of fluid; in a liquid environment, ultrasound waves propagate with minimal changes, so an increase in echogenicity means that the number of normal cells in the glandular tissues (parenchyma) of the organ has decreased.
The pancreas is characterized by age-related changes; they are manifested not only by a diffuse increase in density, but also by small linear foci of increased echogenicity, which indicate local scar (fibrous) tissue transformations.
Point hyperechoic formations are displayed on the screen in case of deposition of calcium salts (calcifications).
A pronounced diffuse increase in the density of the pancreas most often means degenerative-dystrophic processes in the organ, which can be caused by circulatory disorders in the gland, endocrine and metabolic diseases, alcoholism, dysfunction of the liver and biliary tract.
An acute inflammatory process is visualized by an increase in the size of the pancreas, while the echogenicity of its glandular tissue is reduced due to edema, and the edges of the organ have a characteristic compaction. Inflammation can develop into pancreatic necrosis, which is displayed on the ultrasound machine screen in the form of heterogeneity in the structure of the pancreas and unevenness of its contours.
What size should the pancreas be normally? You can find out about this here.
Another factor that increases gland density is diabetes. In patients suffering from this disease, the volume of pancreatic glandular tissue gradually decreases, and the freed space is filled with fat cells. Such changes do not require special treatment, but are reflected in the results of ultrasound.
Another factor that increases gland density is diabetes.
The reasons for a local increase in echogenicity may be:
- concretions (stones) in the gland ducts;
- ;
- focal fibrofatty tissue degeneration;
- metastases.
The predominant part of such changes are the consequences of pancreatitis.
The concept of echogenicity
Echogenicity is a term that is used only to describe the ultrasound picture. It refers to the ability of the tissue to which ultrasound is directed (that is, high-frequency sound) to reflect it. The reflected ultrasound is recorded by the same sensor that emits the waves. Based on the difference between these two values, a picture of different shades of gray is constructed, observed on the device’s monitor screen.
Each organ has its own echogenicity index, and it may be homogeneous or not. The following dependence is observed: the denser the organ, the more echogenic it is (displayed as a lighter shade of gray). Liquids do not reflect ultrasound, but transmit it. This is called “echonegativity,” and fluid structures (cysts, hemorrhages) are called anechoic. For the urinary and gall bladder, the cavities of the heart, intestines and stomach, blood vessels, and ventricles of the brain, this “behavior” is the norm.
Thus, we have analyzed what the echogenicity of the pancreas is - this is the ability of this glandular tissue to reflect high-frequency sound emitted by an ultrasound transducer. It is compared with the properties of the liver (they should either be equal, or the pancreas should be a little lighter), and based on the resulting picture, they talk about a change in the echogenicity of the gland. The homogeneity of the organ is also assessed by this indicator.
An increase in the echogenicity of the pancreas is described when there are fewer normal glandular cells in the tissue of the organ (as we remember, fluid reduces echogenicity, and glandular cells are rich in it). Such a change can be observed both locally and diffusely. In addition, some factors may temporarily affect this indicator.
Warning! The description of echogenicity alone is not a diagnosis.
Treatment
Hyperechogenicity is not a diagnosis, but only a symptom, meaning that certain areas of tissue have high echogenicity.
Comparing the results of an ultrasound examination and the patient’s general history is the task of a gastroenterologist. He should also prescribe treatment.
In most cases, the echogenicity coefficient increases due to pancreatitis, which often manifests itself as a consequence of another disease. In this case, therapy should begin with the cause, and then improve the functioning of the pancreas.
Whether it is a diet or drug treatment is largely determined by the quality of the ultrasound examination and the qualifications of the ultrasound specialist. His competence should allow him to determine the alternation of areas in which the echo density is low, medium or high. Also note whether the contour is smooth, clear, fuzzy edges, notice the slightest important nuances.
We recommend that you familiarize yourself with other methods for diagnosing pancreatic diseases:
- Application of FGDS;
- Comprehensive diagnosis of pancreatitis.
The concept of echogenicity
What does the concept of “echogenicity of the pancreas” mean, which doctors talk about after conducting research? The concept of increased or decreased echogenic factor is widely used when describing the condition of the pancreas after an ultrasound examination of the organ. The echogenicity of the pancreas indicates the physical ability of the digestive organ to reflect ultrasound signals sent by the ultrasound machine.
There are a number of standard notations and tables, according to which each organ in the human body, in the absence of pathologies, reflects the signal only in its individual form. Therefore, a change in the data of the received reflection signals indicates a serious problem with the gland, which serves as a kind of warning. So, what is an increased or decreased echogenic factor and how is it determined by ultrasound equipment?
When diagnosing the body using ultrasound, the signal is reflected from the internal organs according to the principle of returning the frequency and strength of the impulse from the device to the organ and back. Receiving an echo-like return of the impulse, a pattern is displayed on the monitor, from which the doctor determines the increased or decreased signal and the condition of the pancreas, as well as possible neoplasms. And also, using the data obtained, the compactions that have arisen are determined, which makes it possible to identify foci of pathology in certain areas and the cause of their occurrence. What is visible on the monitor of an ultrasound machine when diagnosing a patient?
The signal displayed on the screen of the ultrasound machine is a gray scale, which has its own shades. The shade obtained from the diagnosis indicates whether the ultrasound pulse return signal is increased or decreased. Based on this fact, a possible pathology of the pancreas or its condition is determined. There are also extraneous factors that affect the accuracy of receiving the return signal:
- mobile phone;
- implant in the human heart;
- electrical equipment and items, and much more.
Types of change
When examining the pancreas, its echogenicity is compared with that of a healthy liver; in the normal state, the density of the pancreas is the same as that of the liver, or slightly higher. Changes can have varying degrees and distribution in the body of the gland. A diffuse (encompassing the entire volume of the organ) increase in the echogenicity of the pancreas does not always mean a disease; the presence of local compactions most often indicates pathology.
Echogenicity is displayed on the device screen in the form of a scale of shades of gray; the higher the density of the tissues being examined, the closer the shade is to white.
Slightly
With a slight increase in echogenicity, the ultrasound specialist indicates the presence of changes, but does not make diagnostic conclusions. A slight increase in pancreatic tissue density may be observed in healthy people.
With age, the density of the pancreas increases; the criterion for normality in such cases is the uniformity (homogeneity) of the tissues; if it is preserved, pathology is excluded. Also, in older people, the detection of small hyperechoic inclusions is not considered a pathology.
In older people, the density of the pancreas increases; the criterion for normality in such cases is the uniformity (homogeneity) of tissues; if it is preserved, pathology is excluded.
Moderately
If the homogeneity of the gland is preserved, a diffuse increase in density may not mean disease. To interpret the result, the following are important: the patient’s age, his diet, and the condition of nearby organs. Sometimes such a change is temporary; when nutrition is normalized, a repeated examination may not detect deviations from the norm.
A segmental increase in the density of glandular tissue indicates pathology even with moderate severity of the change.
Much
A significant diffuse increase in the echogenicity of the pancreas indicates degenerative damage to the organ. With a local focal increase in the echo signal, a dangerous disease can also be suspected. Both conditions are most often accompanied by severe clinical manifestations and require therapeutic measures.
?enablejsapi=1″>
?enablejsapi=1″>
About the most important thing PANCREAS Diffuse changes in the pancreas: what they are, signs, treatment
Methods of treating neoplasms
Pancreatic tumors cannot be treated either by diet or by folk recommendations. Patients should not waste time searching for fabulous advertised remedies. A combination of modern methods includes:
- surgical stage - resection of part of the pancreas or together with surrounding organs (gastropancreatoduodenal, subtotal, pancreatectomy),
- consolidation of the operation with multi-course chemotherapy.
The role of diet
The importance of therapeutic nutrition is to maximally support the functions of the pancreas. Pancreatitis necessarily develops against the background of a tumor. Therefore, it is necessary to comply with food requirements:
- give up spicy, fatty foods, fried foods,
- reduce easily digestible carbohydrates in the diet (sweets, honey, jam),
- eat at least 8 times a day, but reduce portions by half,
- all dishes should be steamed or boiled,
- Fresh vegetables, fruits, salads are prohibited,
- salt is limited, seasonings, ketchups, and mayonnaise are excluded.
To improve absorption, food should be in a semi-liquid state, pureed, meat in the form of minced meat.
Surgical intervention
The extent of the operation is determined during the examination. The location of the tumor, size, and growth into nearby vessels and lymph nodes are important. The result should minimize the risk of relapse and digestive disorders. Surgeons resect the surrounding vascular branches very carefully. Excessive removal of blood vessels causes disruption of the intestinal innervation. The development of diarrhea does not make it possible to carry out subsequent full-fledged chemotherapy.
When removing ductal adenocarcinoma, it is usually necessary to simultaneously remove adjacent organs (spleen, colon, part of the stomach, left adrenal gland, half of the diaphragm).
Other tumors are removed if there is compression of neighboring organs or bleeding. The method of choice is partial resection of the gland and angioplasty. The doctor will tell you whether it is necessary to be treated with chemotherapy after a complete cytological analysis.
Chemotherapy
Chemotherapy is used to prepare the patient for radiation. Its goal is to bring the tumor to an operable state. The drugs used are administered intravenously (Gemcitabine, Erlotinib, Capecitabine, 5-fluorouracil), they increase the sensitivity of tumor cells to radiation therapy.
There is ongoing debate among scientists about whether it is worth treating a patient with chemotherapy drugs only. It is believed that the patient can be prepared for surgery without subsequent radiation. Typically, a course of chemotherapy is carried out for 2–3 months before surgery and the same amount after. It has been proven that the survival prognosis is the same.
The drugs are often difficult to tolerate and have negative effects (joint pain, nausea, yellowing of the skin).
Irradiation
If the disease does not progress during chemotherapy, then external radiotherapy is added. The radiation dose is calculated individually for each patient.
In addition to remote irradiation, the following forms of irradiation are used:
- fast electrons,
- Bremsstrahlung radiation.
Radiation therapy is prescribed before and after surgery, and less often - instead of surgery.
Targeted therapy
Targeted therapy is a targeted therapy aimed at a specific target of malignant cells. The created drugs primarily affect tumor cells and suppress their growth. Do not affect surrounding tissues.
Targeted therapy drugs “teach” the body to produce antibodies; they must block the mutating gene that causes the cells to transform into malignant ones. So far, few of them have been synthesized, and the price is too high for general use.
Avastin is suitable for treating pancreatic tumors. One course of treatment will cost $50,000.
When the echogenicity of the entire gland increases
A diffuse change in the permeability of pancreatic tissue to ultrasound can be a symptom of pathology, but can also be observed normally. This cannot be said about foci with increased echogenicity - this is almost always a pathology.
The gland has normal dimensions, but its echogenicity is increased (this can be seen in the two-dimensional graph that displays the density of the liver)
The echogenicity of the pancreatic parenchyma is increased in the following pathologies:
- Glandular lipomatosis, when glandular tissue is replaced by fat cells containing almost no intracellular fluid; however, the size of the pancreas is not increased. This condition is most often asymptomatic. Read more about this disease in the article: How to recognize and treat pancreatic lipomatosis in time?
- Swelling of the gland that develops with acute pancreatitis. Accompanied by abdominal pain, diarrhea, vomiting.
- Organ tumor. If the ultrasound describes the pancreas with increased echogenicity, then there are necessarily symptoms of the disease: weight loss, pallor, weakness, lack of appetite, frequent bowel movements.
- Pancreatic necrosis, accompanied by the death of organ cells, will also appear on ultrasound as a lighter area. This disease has such signs as severe abdominal pain (up to the development of painful shock), disturbance of the general condition, uncontrollable vomiting, and diarrhea.
- As a result of diabetes mellitus, which is manifested by thirst in the absence of hot conditions, elevated temperature, active work, as well as frequent and abundant (including night) urination.
- Development of connective tissue in the gland () - usually as a result of previous inflammation or metabolic disorders. In this case, a person may remember cases of unstable stool and abdominal pain. Ultrasound shows not only an increase in echogenicity, but also a decrease in the size of the gland and the tuberosity of its contours.
The hyperechoic pancreas can also be a temporary phenomenon, manifested by:
- as a result of reactive inflammation in many infectious diseases: influenza, pneumonia, meningococcal infection. This requires treatment of the underlying disease;
- when changing the type of food consumed;
- after a lifestyle change;
- at certain times of the year (usually spring and autumn);
- after a recent heavy meal.
In such temporary conditions, the echogenicity of the pancreas is moderately increased, in contrast to pathologies, when significant hyperechogenicity is noted.
Local increase in echogenicity
Fatty inclusions in the pancreatic tissue will appear hyperechoic.
What are hyperechoic inclusions in the pancreas? It can be:
- pseudocysts - liquid formations that develop as a result of acute pancreatitis; with this disease, the contour of the pancreas becomes uneven, jagged, hyperechoic;
- calcification of tissue areas - calcifications; they are also formed as a result of inflammation (usually chronic);
- areas of adipose tissue; they replace normal gland cells in case of obesity and excessive consumption of fatty foods;
- fibrous areas - where areas of normal cells have been replaced by scar tissue; usually this occurs as a result of pancreatic necrosis;
- stones in the gland ducts;
- fibrocystic degeneration of the gland is either an independent disease or an outcome of chronic pancreatitis;
- metastatic tumors.
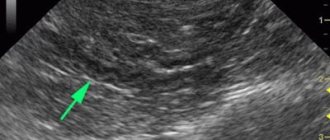
Calcifications in the pancreas on ultrasound
Important. If there is dilatation of the pancreatic duct, you should look for stones in the pancreatic duct and in the common bile duct.
Calcifications inside the pancreas can give an acoustic shadow, but if they are small, they appear as a separate bright echostructure without an acoustic shadow. In chronic pancreatitis, calcifications are distributed diffusely throughout the pancreas. Stones in the duct are located along the duct. Gallstones in the distal common bile duct may be mistaken for calcifications in the pancreas. Calcifications are clearly visible on CT, and for non-calcified stones, MRI or ultrasound is preferable.
| Photo. A - There is a small stone in the dilated duct. B - In the dilated pancreatic duct there is a row of several stones with shadowing behind. B — A patient with chronic pancreatitis has huge stones in the dilated duct. Note the intense shading behind. | ||
| Photo. A, B — Calcifications in the pancreatic parenchyma in patients with chronic pancreatitis. Some calcifications have a shadow. B — A 5-year-old boy with chronic hereditary pancreatitis: calcifications (small arrows) and dilatation of the pancreatic duct (large arrow). C - confluence of the superior mesenteric and splenic veins. | ||
What changes occur in the pancreas
As already noted, various types of abnormalities on ultrasound indicate that pathological processes are occurring in the gland. With diffuse changes, the organ may increase or decrease.
Tissues can become denser, their structure becomes heterogeneous. Often the contours of the pancreas become unclear. Decoding the diagnostic results describes in detail all such phenomena.
This is what happens in the gland in the presence of certain pathologies:
- In acute pancreatitis, the pressure in the duct increases. The organ tissues are destroyed and the body is poisoned. Such processes signal themselves with terrible pain.
- In the first stages of chronic pancreatitis, the gland is swollen. Then it decreases and becomes sclerotized.
- With fibrosis, some areas of the organ are replaced by connective tissue.
- Replacement of organ areas with adipose tissue is an irreversible process. With a massive process, the pancreatic parenchyma is compressed.
- In pancreatitis or diabetes, ultrasound shows various signs of changes in the parenchyma, hyperechoic areas are noted in it.
- Structural changes affect the parenchyma, since it consists of many glands.
- Possibly tumors.
- Reactive changes indicate that the patient has problems with the liver and gall bladder.
- Finally, due to cell death, ultrasound shows fatty degeneration.
It is possible that mild changes may occur that do not affect the functionality of the gland.
Changes in echogenicity during pregnancy
Acoustic changes can occur in fetal and maternal tissues. The doctor may notice some pathologies in the intestines of the unborn child. Often they talk about ischemia of this organ, cystic fibrosis, developmental delay. When an organ is perforated, an increase in its echogenicity is also noticeable.
The doctor also determines the ultrasonic density of the placenta. An increase in it indicates the onset of an organ infarction, detachment, as well as the presence of calcifications in it. Normally, calcifications can only appear after the 30th week of pregnancy.
An increase in ultrasound density of amniotic fluid is normal, but only after the 30th week. If such a change is determined before this period, then additional examination is required for the mother and fetus.
Increased echogenicity of the pancreas in a child
Sometimes this phenomenon occurs in young children. The heterogeneity of the structure of the pancreas manifests itself as dysfunction of the gastrointestinal tract, which most often occurs due to spasm of the pancreatic ducts and increased activity of its enzymes. Their obstructed outflow provokes swelling of the organ in the child.
This disease can develop even in children of one year of age, and the most common reason for its development is the incorrect introduction of complementary foods: previously adding fish and meat products to the diet or too quickly, not gradually accustoming the baby to adult food.
Causes
Increased echogenicity is accompanied by changes in the contours of the organ, the appearance of tuberosity, an increase in the size of the gland and occurs against the background of many liver diseases. When the entire liver parenchyma is affected, diffusely increased echogenicity occurs. Changes in the structure in certain areas of the organ lead to focal increases. Most often the cause is one of the following.
In cirrhosis, liver cells are completely replaced by connective tissue. There is a heterogeneous structure with tuberous contours and significantly increased echogenicity.
Chronic hepatitis
Depending on the stage of development of hepatitis, healthy cells are replaced by fat cells, which leads to fatty degeneration of the gland. Ultrasound reveals light areas of heterogeneous structure and moderately increased reflectivity of waves.
Liver neoplasms
A benign hemangioma or adenoma has a homogeneous structure, with a smooth or uneven contour border and increased density.
Too high echogenicity indicates the presence of a malignant tumor.
An abscess of a bacterial or parasitic nature is also the cause of a high echogenicity index.
Cystic formations usually contain an accumulation of pus, which is observed on the monitor as a slightly increased echogenicity.
Other diseases that contribute to increased tissue density include:
- Heart diseases.
- Diabetes.
- Focal or diffuse form of fatty hepatosis.
- Obesity.
- Drug poisoning.
- Inflammation of the pancreas and other organs located near the liver.
What is echogenicity?
Echogenicity is usually called a special system that determines the correspondence of the anatomical structure of the digestive tract organs with the reflection and absorption of ultrasonic waves.
Fluid tissue of the pancreas should correspond to the average level on this scale.
The study is carried out using ultrasound. This technique, in addition to the perception of high-frequency waves by the internal organs of the gastrointestinal tract, allows you to determine other indicators:
- Contours.
- Dimensions.
- Structures.
- Form.
Volume
To determine the volume of an organ, calculate the length of the entire organ, including the head, tail, and body. These indicators should not exceed 30, 24, 25 mm.
When the latter value is elevated, an inflammatory process occurs in the organ. If the size is increased, pancreatitis can be judged.
This also includes abdominal injuries, hepatitis, biliary dyskinesia, and organ infection. With local changes, cysts and malignant tumors occur.
According to external data, the organ has an oblong shape in the form of a comma. Thickenings are observed in the area of the head. Any irregularities in form are considered to be a deviation.
The contours of the organ must have clear boundaries. If any blurry outlines are visible on the image, this is a clear sign of an inflammatory process.
If the boundaries are blurred or swelling is observed, this may indicate diseases of the neighboring digestive organs.
Focal processes
Multiple small areas of reduced echogenicity may indicate previous acute pancreatitis. They form at the sites of former hemorrhages, where further tissue destruction (necrosis) occurred. The overall reflection of ultrasound by the gland may also be slightly reduced.
A single local attenuation of the echo signal is characteristic of:
- acute limited pancreatitis - inflammation in any part of the pancreas (head, body, tail) with an increase in only this segment and a change in echo parameters in it;
- chronic focal pancreatitis – heterogeneous echo structure of any part of the gland (“marbling” of the tissue);
- neoplasm.
With regard to tumors and tumor-like changes, it is necessary to take into account that sonography is not a completely reliable method of detecting, much less identifying, such processes. But, first, an ultrasound diagnostic specialist can distinguish a benign formation from cancer.
The cyst has clear boundaries, represented by a capsule, and is visualized as a rim with an increased echo signal surrounding the area of complete absence of ultrasound reflection. One of its main characteristics is that it is a formation that has a regular round or oval shape.
A pseudocyst does not have a capsule. The darkened area at the borders, visible on the device monitor and sonograms, gradually transforms into the echo structures of the unchanged gland.
A malignant tumor is characterized as a homogeneous hypoechoic formation, having wavy borders with thin outgrowths along the periphery. There is a change in the contours of the gland itself - protrusions are visible at the tumor site.
Tumor of the head of the pancreas
High-class ultrasound scanning equipment and appropriate qualifications of a specialist make it possible to reduce diagnostic errors in the early detection of tumors. This is facilitated by the presence of a Doppler mode, which evaluates the presence of blood flow in the formation and its intensity.
There are a number of reasons why the echogenicity of the pancreas may be reduced, but this is not related to the above. Visualization deteriorates when the patient is insufficiently or incorrectly prepared for the study or is overweight. In addition, in the case of isolated liver disease, the normal echo signal from the pancreas will be determined to be attenuated in comparison.
Click on pictures to enlarge.