Perforated duodenal ulcer ranks last among surgical diseases. Complications from this illness can be disastrous. In 10–12% of patients with ulcers, perforation develops. The pathology is most often diagnosed in men than in women. According to statistics, perforation in the duodenum is more common in young people, and in the stomach it forms in old age.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Complications
- Forecast
- Prevention
Etiology
The chance of developing the disease is possible if a person is diagnosed with the chronic stage of an ulcer or has had acute attacks. A perforated duodenal ulcer can also form for the following reasons:
- inflammation near the source of damage;
- overeating;
- increased level of hydrochloric acid;
- consumption of prohibited foods and alcohol;
- strenuous physical activity.
As a result of modern research, doctors have determined that the cause of the disease is the bacterium Helicobacter pylori. The formation of a perforated ulcer is directly influenced by those factors that cause the development of a common peptic ulcer:
- deterioration of immunity;
- stress;
- sleep disturbance;
- taking illegal or heavy drugs;
- smoking and alcohol;
- unbalanced diet;
- heredity;
- the presence of other gastrointestinal ailments.
Causes of pathology
There are so many factors that provoke the development of this disease that sometimes, after the perforation has begun and it has been successfully stopped, it is not possible to find out what exactly caused the pathology. Such cases are most often observed in young patients.
The main reason why a perforated duodenal ulcer occurs is Helicobacter pylori. It is also generally accepted that it can be caused by the following factors:
- A foreign object enters the mucous membrane of the duodenum or stomach and causes mechanical damage.
- Dietary disorders - eating smoked, spicy, fatty or fried foods in the acute phase of development of duodenal and gastric ulcers.
- The development of concomitant pathologies of the gastrointestinal tract, which have an indirect effect on the state of peptic ulcer.
- Poisoning with chemicals or burns of the mucous membrane of the digestive organs.
- Abdominal injury.
- Infectious infection of the gastrointestinal tract.
- Alcohol abuse with a history of chronic ulcerative pathology.
- Excessive use of certain medications, usually non-steroidal anti-inflammatory drugs.
- Inadequate treatment or its absence in acute or chronic forms of peptic ulcer.
- Having diseases such as diabetes, cancer, AIDS or autoimmune diseases.
In the rarest cases, physical overstrain of the abdominal cavity can provoke the development of a duodenal ulcer. It usually occurs when lifting excessive weights.
Classification
Clinicians have determined that perforation of a duodenal ulcer can manifest itself in different forms depending on the criteria for assessing the disease. According to the etiology, there is perforation:
- chronic pathology;
- acute illness;
- with tumor damage to the walls of a hollow organ;
- with a parasitic disease;
- due to a disruption in blood circulation.
Ulcers can form in:
- stomach;
- duodenum;
According to clinical indicators, the following forms of the disease are divided:
- perforation into the peritoneum;
- atypical perforation;
- perforation with bleeding.
Classification of perforated duodenal ulcer
Clinicians also determined that the pathology has several phases of progression:
- primary shock;
- contamination with microorganisms and the development of bacterial peritonitis;
- systemic inflammatory response;
- severe abdominal sepsis with purulent peritonitis.
Treatment of perforated ulcers
A patient with a perforated ulcer requires emergency medical attention. If the patient consults doctors at the first stage, they will most likely be able to preserve the duodenum. It is possible to suture the ulcer or remove a section of the intestine with an ulcerative defect.
To prevent perforation, a person with a duodenal ulcer needs to adhere to certain lifestyle recommendations: follow a diet, eliminate bad habits, try to avoid stress, etc. The patient also needs to periodically check his gastrointestinal tract using gastro- and colonoscopy to monitor the disease.
To treat ulcers, you can use a gastroprotector based on rebamipide (Rebagit). This drug has shown itself well in restoring the mucous membrane of the gastrointestinal tract. To reduce pressure in the stomach and intestines, I recommend a prokinetic agent (itomed), which restores normal motility of the digestive organs.
Take care of yourself and be healthy!
Author: Sergey Vyalov – gastroenterologist at GMS Clinic, Ph.D. Member of the American Gastroenterological Association (AGA) and the Russian Gastroenterological Association (RGA), member of the European Society for the Study of the Liver (EASL), member of the Russian Society for the Study of the Liver (ROSIP). He trained and worked at the Charite clinic (Germany).
, for today 1
Symptoms
During the typical course of the disease, the patient can be detected with the contents of the duodenum entering the peritoneum. The symptoms of the pathology vary depending on the period of development of the disease. At the time of chemical peritonitis, which lasts up to 6 hours, the pathology in the duodenum has the following symptoms:
- acute pain in the navel area and under the right rib; there may be pain on the left side of the abdomen and forearm due to perforation of the anterior wall of the organ;
- rare vomiting;
- decreased pressure in the arteries;
- rapid breathing;
- pale skin;
- increased sweating;
- Gases accumulate in the peritoneum.
The next stage of development is bacterial peritonitis. It begins 6 hours after the formation of perforations. At this stage, the disease is characterized by the following symptoms:
- the abdominal muscles relax;
- breathing deeper;
- pain subsides;
- temperature rises;
- pulse quickens;
- formation of a large amount of gases;
- dry oral cavity with a gray coating.
A patient in this state may experience euphoria and relief, become a little irritable, and want to be alone. If treatment is not started at this stage, then the body develops the third stage, which is particularly complex.
The stage of acute intoxication during perforation of a duodenal ulcer is characterized by severe symptoms. At this point, the patient complains of severe vomiting and dehydration. The following symptoms are also added:
- dry skin;
- temperature changes;
- rapid pulse;
- high pressure in the arteries;
- lethargy;
- slow reaction;
- the abdomen enlarges due to the accumulation of gases and liquids;
- failure of urinary excretion.
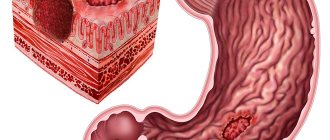
Stages of development of a perforated ulcer
A perforated ulcer goes through three stages of development within 24 hours. Of course, it is best if the patient seeks medical help during the first phase - this period is considered the most favorable for surgery. Yes, perforation can only be eliminated through surgery.
Perforation stages:
- Acute stomach. The patient develops severe abdominal pain. They last for 6-8 hours. At first the pulse is rare, but gradually it becomes faster. Blood pressure is reduced in the first hours, but then returns to normal. The patient breathes frequently and not deeply, so as not to provoke increased pain.
- Imaginary well-being. This is the longest and most dangerous period. Doctors also call this stage treacherous. Symptoms disappear (except for bloating) for 12 hours. Because the pain disappears, patients calm down and put off calling an ambulance. Approximately 6 hours after the start of remission, the body temperature begins to rise.
- Peritonitis. Food entering the abdominal cavity causes severe inflammation. The temperature rises, severe pain appears again. If the patient is not helped quickly, he may die.
Diagnostics
To establish the correct diagnosis, the doctor must thoroughly examine the intestines, stomach and analyze the functioning of the entire gastrointestinal tract. To establish the disease, it is necessary to conduct laboratory and instrumental studies.
First of all, the doctor must examine the patient. The pathology is characterized by a sharp onset of pain. When diagnosing a disease, it is important to know whether the patient had early gastrointestinal diseases, for example, a history of peptic ulcers or gastritis. During palpation, the doctor can presumably assess the patient's condition. To make an accurate diagnosis, the following diagnostic methods are used:
- X-ray;
- Ultrasound;
- endoscopic examination;
- ECG;
- laparoscopy.
Duodenal endoscopy
Also, the patient must undergo a series of laboratory tests. As part of this examination, the patient must donate blood for general and biochemical analysis.
The doctor needs to carefully analyze all the results, since the symptoms of the disease may be similar to: perforation of a gastroduodenal ulcer, pleurisy, pneumonia, renal colic or other ailments.
Treatment
To treat the perforated part of the duodenum, doctors most often resort to radical measures - surgery. Surgical intervention for this type of pathology can be of different types, it all depends on the degree of the disease. The doctor may prescribe one of the following operations to the patient:
- suturing the perforated hole;
- plastic;
- vagotomy;
- gastric resection.
Most often in practice, doctors prescribe suturing of a perforated ulcer to a patient. The main goal of such an intervention is to save the patient’s life.
Surgeons can perform therapy using truncal vagotomy and pyloroplasty if an ulcer has developed in the pyloric part of the stomach, bleeding and stenosis have begun. If prompt care is not provided, the patient may die.
A perforated duodenal ulcer requires quality treatment and a diet after surgery. To increase the chances of recovery and reduce the possibility of re-inflammation of the disease, the patient must follow all the doctor’s recommendations. In the first period after surgery, the patient is prescribed a strict diet, which can last up to six months. The complication of the diet occurs gradually.
During the postoperative period, the patient should adhere to the following dietary principles:
- eat at least 6 times a day;
- all dishes should be liquid and light;
- the ingredients must be steamed or well boiled;
- limit salt intake;
- reduce sweetness and liquid in your diet.
On the second day after surgery, the patient is allowed to drink mineral water, fruit jelly, weak and slightly sweet tea. After a few more days, you can diversify your diet with pureed soups, cereal porridges, vegetarian first courses of carrots, pumpkin, zucchini, potatoes or beets. You can also eat eggs and cottage cheese souffle cooked in a steam bath.
Diet in the early postoperative period
After a 10-day strict diet after surgery, the patient is allowed to gradually introduce into the menu:
- cutlets, meatballs and zrazy from low-fat meat and fish, which are steamed;
- cheesecakes, pudding, cottage cheese casserole;
- fresh crushed cottage cheese;
- milk and non-sour dairy products.
After a month, you can diversify the menu with dried bakery products. And after two - add sour cream to dishes and drink kefir.
At the same time, the diet after a perforated duodenal ulcer implies some food restrictions:
- fatty foods, broths;
- yeast baked goods;
- dishes with spicy, smoked or salty ingredients;
- smoked products;
- canned food;
- mushrooms;
- legumes;
- marinades;
- sauces;
- jam and honey;
- chocolate, cocoa and ice cream;
- alcohol.
In the process of improving the patient’s condition, he is allowed to diversify his diet with new dishes from meat, vegetables, cereals and dairy products. You need to completely eliminate all canned, spicy and smoked foods.
In medical practice, there is a traditional method that is used in emergency cases when surgery cannot be performed for objective reasons. In this situation, doctors use the following method of therapy:
- a transnasal gastric tube is inserted to empty the stomach of contents;
- carry out infusion therapy;
- antibiotic treatment is prescribed.
Forecast
In recent years, the number of deaths during surgery has decreased and accounts for a maximum of 7% of all patients. This figure depends not only on the patient’s condition, but also his age, and the correctness of the chosen method of operation.
In the postoperative period, the number of deaths is also possible. During the first 6 hours, a maximum of 4% of patients may die. The majority of deaths occur within the next 24 hours after surgery. During this time, up to 40% of patients may die.