Dysphagia is a violation of the complex reflex swallowing act. This is not a separate nosology, but a syndrome that manifests itself in many diseases. Patients complain of difficulty swallowing food, pain in the retrosternal area, salivation, belching, and heartburn. If the act of swallowing is impaired, symptoms associated with food entering the respiratory tract are common, which is manifested by coughing and hoarseness. The doctor’s tactics are aimed primarily at identifying the causes.
To do this, use pharyngoscopy, radiography of the esophagus with contrast, FGS (if necessary with a biopsy), measurement of pH indicators and manometry of the esophagus. After differential diagnosis and identification of a disease occurring with dysphagia syndrome, etiotropic conservative or surgical treatment is prescribed.
Esophageal dysphagia: symptoms
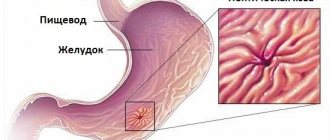
Esophageal dysphagia is most often caused by esophageal diseases, diseases of the gastrointestinal tract, and pathology of the mediastinal organs.
Acute esophageal dysphagia occurs as a result of:
- allergic edema (Quincke's edema);
- obstruction by a foreign body.
Causes of esophageal dysphagia:
- Narrowing of the lumen of the esophagus causes esophageal cancer (stomach cancer localized in the cardia) and GERD also occur. Cicatricial narrowings occur after chemical burns and radiation therapy for thoracic oncology.
- When the esophagus is compressed by tumors of the chest organs (lung cancer, bronchi), enlarged lymph nodes of the mediastinum, paraesophageal hiatal hernia, cardiac pathology with severe myocardial hypertrophy.
- Violation of coordinated contraction of the esophageal muscles can be a sign of achalasia, total spasm of the esophagus, diabetes mellitus, and scleroderma.
- Infectious diseases (tuberculosis) and uncontrolled use of certain drugs (calcium antagonists, nitrates) can lead to disruption of esophageal peristalsis.
Symptoms of esophageal dysphagia:
- in the initial stage of the disease, patients complain of difficulty swallowing dry, solid food;
- retrosternal pain, drooling, often heartburn, dry cough, hoarseness appear;
- As the symptoms progress, the symptoms increase, and difficulties appear when swallowing soft foods and then liquids.
Folk remedies for the treatment of dysphagia
Traditional healers recommend that those suffering from dysphagia take a healing decoction before eating. Its composition: 25 g hop cones, 20 g rosemary leaves, 25 g peppermint leaves, 20 g St. John's wort herb, 25 g lemon balm leaves, 30 g valerian root. Grind all the ingredients well and mix, pour a tablespoon of boiling water, let it brew for 2 hours, strain. Drink a quarter glass half an hour before meals 3 times a day.
10 minutes before meals you can take 15 drops of belladonna tincture. As an antispasmodic agent, you can use a decoction of 15 g of godson root, 20 g of ephedra herb and 20 g of motherwort herb. Pour the crushed and mixed herbs with cold water for 3-4 hours, then bring to a boil, strain and take a couple of tablespoons 10 minutes before meals.
After eating, you can drink syrup an hour or two later. 5 tbsp. l. Boil plantain for half an hour, cool, add a teaspoon of celery seed, 200-300 g of honey, boil again and strain.
Flaxseed and anise fruits, taken in equal parts, honey and water, ease the symptoms of dysphagia. Boil everything, strain and drink instead of water.
You can do an enema before going to bed. For a liter of strong black tea, take a decoction of 3 tbsp. l. chamomile per liter of water.
Types of dysphagia
All diseases occurring with dysphagia syndrome, depending on the anatomical level of swallowing disorders, are divided into:
- Oropharyngeal (oropharyngeal) dysphagia is a violation of the formation of a food coma and its movement into the pharynx, in this case the initial swallowing movements are disrupted.
The causes may be neurological pathology, thyromegaly, lymphadenopathy, oncological diseases of the head and neck, and degenerative processes of the spine. Main symptoms:
- cough;
- nasal regurgitation;
- attacks of suffocation.
Treatment depends on the causes of this syndrome.
- Esophageal (esophageal) dysphagia is a violation of the movement of food from the pharynx to the stomach. The causes of the disease are narrowing or compression of the esophageal tube, as well as impaired motility.
In addition, all dysphagia is divided into:
- spicy;
- chronic
According to the nature of the flow:
- intermittent;
- permanent;
- progressive, with increasing clinical symptoms.
Treatment of dysphagia
Of course, the treatment of dysphagia depends on the cause of its occurrence. If the disease was caused by disorders of the nervous system, then the patient requires attention and care while eating. It is necessary to control the consistency of food, the position of the patient’s body, you need to monitor the frequency of swallowing and portions of food. For such patients, tea, spicy or sour foods are not recommended, coffee and alcohol are contraindicated. It is advisable that after a meal the patient does not take a horizontal position for 3 hours. If the disease is a consequence of a systemic disease, then it needs to be treated.
In case of acute symptoms of dysphagia, it is necessary to urgently empty the airways of food and liquid and carefully monitor that the patient does not experience asphyxia. Further, the disease must be treated inpatiently; in especially severe cases, food and drink are administered through a tube.
If dysphagia appears as a result of the development of inflammatory processes, then treatment is carried out with aluminum-containing drugs that reduce acidity. Treatment of dysphagia, which is accompanied by hypermotility of the digestive tract, is based on taking antispasmodics. If drug treatment does not help, then the patient is prescribed surgery. Organic dysphagia is treated with either muscle stimulating or muscle-inhibiting drugs. For esophageal hernias, surgical intervention is prescribed as therapy, and if the disease is bacterial in nature, then treatment begins with identifying and treating the infection.
In addition to medications, diets and food intake rules are used to treat dysphagia. It is better to eat fractionally, portions should be small, it is better to exclude hard and dry foods, chew food for a long time and thoroughly. It is prohibited to eat dry food or quickly. It is not recommended to bend forward for two hours after eating. The final meal should be no later than 2 hours before bedtime. Nutritionists recommend light food. Steamed vegetables, lean fish, poultry, and white meat are suitable. It is better to exclude fatty, smoked and fried foods from the diet; you should also avoid spicy and spicy foods. Fizzy drinks, fast food, coffee and strong tea are also prohibited for those suffering from esophageal dysphagia. You should not eat coarse fiber. Porridges, slimy soups, vegetable and dairy products are best suited for such patients.
Dysphagia - what is it?
Dysphagia (Greek dys - denial, phagein - is) is the general name for a swallowing disorder.
Dysphagia is a syndrome (complex of symptoms) manifested by a violation of the act of swallowing.
Oropharyngeal dysphagia
Oropharyngeal dysphagia is also called “upper”; with this form of dysfunction, the oral and oropharyngeal phases of swallowing are disrupted.
Oropharyngeal dysphagia syndrome includes the following symptoms:
- difficulty at the very beginning of swallowing;
- return of food through the nasal passages;
- cough;
- attack of suffocation;
- neurological diseases leading to oropharyngeal dysphagia often occur with dysarthria (impaired articulation and pronunciation) and diplopia (impaired function of the visual muscles);
Causes of oropharyngeal dysphagia:
- Obstruction of the esophageal tract.
- various infectious processes (sore throats, pharyngitis, abscesses);
- enlargement of the thyroid gland (thyromegaly);
- various lymphadenitis;
- Zenker's diverticulum;
- various types of myositis and fibrosis;
- cervical osteochondrosis;
- oropharyngeal malignancy;
- Disturbance in the conduction of nerve impulses to muscle fibers:
- diseases of the central nervous system (brain tumors, stroke, Parkinson's disease);
- disorder of nerve impulse transmission to smooth muscles (ACD dysfunction).
- Psychosomatic disorders (neuroses, various functional disorders).
Treatment of oropharyngeal dysphagia depends on the etiology of the disease.
Dysphagia in stroke
Swallowing is a complex reflex reaction.
Peripheral innervation of the muscles involved in the act of swallowing is carried out by pairs of cranial nerves, their afferent and efferent fibers (trigeminal nerve, facial nerve, glossopharyngeal nerve, recurrent, hypoglossal nerve).
The central nuclei of regulation of the act of swallowing are located in the reticular formation of the brain stem. The cortical swallowing centers are located in the posterior parts of the frontal lobes.
With cortical strokes, a clinical picture of pseudobulbar syndrome appears:
- as a result of central paresis of the masticatory muscles, chewing food becomes impossible, the lower jaw droops;
- due to central paresis of the muscles of the tongue and cheeks, the movement of food to the root of the tongue is disrupted.
With brainstem strokes, a clinical picture of bulbar syndrome develops, caused by central paralysis of the cranial nerve:
- choking when swallowing liquid food as a result of it entering the respiratory tract;
- difficulty and inability to swallow solid food as a result of paresis of the pharyngeal muscles;
- nasal tone of voice;
- aphonia due to paresis of the vocal cords;
- dysarthria due to paralysis of articulatory muscles;
- cardiac pathology (arrhythmias).
In the treatment of dysphagia after a stroke, in addition to the neurologist, a speech therapist plays an active role. He primarily assesses the severity of dysphagia, dysarthria and dysphonia, since the same muscle groups are affected. For this purpose, the L.I. scale is used. Wasserman, a dysphagia rating scale, a three-sip test, a protocol that records in detail the condition of the facial muscles, articulatory apparatus, and the condition of the soft palate.
The speech therapist gives the patient’s relatives a reminder:
- how to properly care for a neurological patient, how to feed the patient;
- what products can be used and in what form, how to properly use a food thickener;
- how to do facial gymnastics yourself.
During the rehabilitation period, a patient suffering from dysphagia after a stroke learns to swallow again.
If the swallowing function is completely disabled and the patient is unable to swallow anything, a nasogastric tube is placed.
Paradoxical dysphagia
Paradoxical dysphagia is a special type of change in the act of swallowing, when the patient is able to swallow solid food, but liquid food is retained.
Paradoxical dysphagia (Lichtenstein syndrome), characteristic of:
- achalasia cardia;
- esophageal diverticulum;
- burns of the esophagus;
- HH;
- esophagitis;
- esophageal tumors.
In the mechanism of occurrence of the syndrome, the main role is played by hypermotor dyskinesia of the esophagus.
Sideropenic dysphagia
Sideropenic dysphagia (Plummer-Vinson syndrome) occurs with a lack of iron in the body and hypovitaminosis B₂ and B₉. The disease occurs more often in women.
This systemic disease is characterized by the following symptoms:
- dysphagia, which can be constant and accompanied by unpleasant sensations along the esophagus;
- hypochromic anemia;
- atrophy of the mucous membranes (atrophic glossitis, pharyngitis, esophagitis, gastritis);
- trophic changes in nails, hair, skin;
- disturbance of taste, smell, vision.
Neurogenic dysphagia
Various neurological diseases are often complicated by dysphagia. The act of swallowing is a complex reflex reaction that requires the coordinated work of many muscles, which is ensured by the work of all levels of the central nervous system and peripheral nerves.
The condition can occur with organic diseases of the brain, subcortical formations, brain stem, and cerebellum. Often there is psychogenic dysphagia, which is purely functional in nature, developing against the background of various neuroses.
The cause of peripheral neurogenic dysphagia is damage to the glossopharyngeal (IX pair of cranial nerves), sublingual (XII pair of cranial nerves) and recurrent (X pair) nerves.
The most common cause of neurogenic dysphagia is stroke.
Together with organic pathology of the nervous system, dysfunction of the swallowing muscles is a common manifestation of psychogenic, functional disorders. Against the background of prolonged mental stress, overwork, and emotional exhaustion, various types of neuroses appear, accompanied by a feeling of fear, unconscious aggression, and a tendency to hysteria.
Symptoms:
- complaints of difficulty swallowing;
- itching;
- sore throat;
- hoarseness of voice.
Treatment of neurogenic dysphagia is carried out by a neurologist, and if necessary, the patient is consulted by a psychiatrist.
Dysphagia in the elderly
Dysphagia is a common human pathology, but older people are more likely to suffer. This is due to the fact that with age, muscles lose elasticity and firmness, age-related muscle weakening occurs, and, as a result, dysphagia occurs.
In addition, they contribute to the development of dysphagia in older people:
- degenerative diseases of the central nervous system;
- past illnesses (stroke, head injury, gastrointestinal diseases);
- oncological diseases;
- the presence of severe chronic diseases (diabetes mellitus, ischemic heart disease, hypertension).
Dysphagia in children
Dysphagia in children has some features. First of all, this is due to the diseases that cause this syndrome.
The causes are the following pathologies:
- Cerebral palsy is the general name for a large group of diseases, common to which is damage to the brain structures responsible for voluntary movements.
- Athetosis (hyperkinesis) – involuntary movements in individual muscle groups, occurs when subcortical structures are damaged. It appears immediately after birth, is the result of birth injuries, kernicterus.
- Various congenital pathologies of the oral cavity and nasopharynx.
- Infectious lesions of the pharynx, larynx, esophagus.
- Consequences of surgery.
- Oncological pathology.
The efforts of doctors are aimed at treating the disease that caused dysphagia and eliminating or reducing the severity of this syndrome.
Particular attention is paid to neurological pathology, since these diseases have not only medical, but also social significance. An entire rehabilitation program for patients with cerebral palsy has been developed. Rehabilitation measures begin almost from the first days of life (drug therapy, massage, exercise therapy, physiotherapeutic procedures are carried out). From the age of three, a speech therapist is involved in treatment.
Dysphagia after fundoplication
In severe forms of GERD, a fundoplication operation is performed - this is an anti-reflux operation, which consists in forming a special cuff from the bottom of the stomach around the esophagus, preventing the reflux of reflux into the esophagus (Nissen fundoplication). The operation has proven itself and gives good results. However, after fundoplication in the early stages after surgery, dysphagia and moderate epigastric pain are often observed. This is due to the fact that a “new” esophageal valve is being formed and the body is adapting to it. These unpleasant sensations go away without any treatment.
Functional dysphagia
Functional dysphagia is a manifestation of various neuroses. This form of pathology can manifest at any age. People suffering from cadiospasm have a special psychological characteristic - they:
- suspicious;
- anxious;
- are susceptible to various types of phobias.
In children, functional dysphagia of the esophagus and pharynx may be present from a very early age. It is often accompanied by the following symptoms:
- poor appetite;
- frequent regurgitation, vomiting
- bad night's sleep.
Without treatment, by the age of 7, children experience dystrophy, increased fatigue, and poor tolerance of physical and mental stress.
Prevention of dysphagia
You can prevent the development of esophageal obstruction if:
- visit a doctor in a timely manner and responsibly treat gastrointestinal diseases;
- eat rationally, including vitamins, proteins, minerals in the menu;
- do not drink alcohol, give up cigarettes;
- sleep 8 hours a day, play sports, follow a work and rest schedule;
- strengthen the immune system by hardening;
- avoid stressful situations.
Dysphagia is manifested by difficulty swallowing and is a symptom of diseases of various etiologies. The initial stage of the disease can be treated with medication. Elimination of the extreme stage of esophageal obstruction is possible only by surgical intervention. Therapy with folk remedies will relieve inflammation, strengthen the immune system, and calm the nerves. Prevention of dysphagia involves a healthy lifestyle.
We recommend: How to cure a sore throat when swallowing without fever and not harm the body?
Diagnosis of dysphagia
Dysphagia syndrome itself usually does not cause diagnostic difficulties. All efforts of doctors are aimed at identifying the disease that causes dysphagia. In terms of diagnosis, the following examinations are carried out:
- Pharyngoscopy is a method that allows you to identify the causes of oropharyngeal dysphagia: glossitis, tonsillitis, neoplasms, foreign bodies. Pharyngoscopy is complemented by indirect laryngoscopy; the method allows identifying pathology of the epiglottis.
- Fluoroscopy with contrast of the esophagus can detect esophageal motility disorders and diverticula.
- EFGS reveals foci of inflammation and areas suspicious for cancer pathology. If necessary, a tissue biopsy is performed for morphological examination.
- Long-term measurement of the pH of the environment inside the esophagus is the most reliable method for identifying GERD; esophageal manometry is performed (to determine disturbances in the functioning of the esophageal esophagus).
- Laboratory research methods are nonspecific:
- in peripheral blood, slight leukocytosis, anemia, and increased ESR may be detected;
- in venous blood, a decrease in total protein, dysproteinemia, is most often observed;
- testing stool for occult blood.
In order to identify neurological pathology, an in-depth neurological examination is performed. If clinical diagnosis is in doubt, instrumental diagnostics are performed:
- CT scan of the brain;
- MRI;
- EEG.
If cardiac or pulmonary pathology is suspected, the following is carried out:
- chest x-ray;
- ECG;
- echocardiography.
Treatment of dysphagia is carried out after the final diagnosis.
Treatment
The doctor’s tactics in the treatment of dysphagia are determined by the cause of the disease and the severity of the syndrome. The efforts of doctors are aimed at quickly restoring the act of swallowing and preventing aspiration complications.
Acute cases of dysphagia require urgent care:
- the foreign body is urgently removed.
- desensitizing therapy is urgently carried out.
With a long course of the disease, complicated by dysphagia, a full course of etiopathogenetic treatment is carried out. The following medications are used:
- Means for improving the neuroregulation of the act of swallowing. For degenerative diseases, dopamine agonists and precursors, central H-anticholinergic blockers are prescribed. For strokes, membrane stabilizers, neuroreparants, and neuroprotectors are widely used.
- Calcium antagonists. The medicine reduces the concentration of intracellular calcium, thereby eliminating spasm of muscle fibers (diffuse esophageal spasm, achalasia), thereby improving the passage of food.
- Antisecretory drugs. These drugs are used for GERD and eosinophilic esophagitis with dysphagia. Antacids, PPIs, and IGRs are used.
- For infectious etiology of the disease (sore throat, abscesses, pharyngitis), antibacterial therapy is indicated.
- Traditional medicine is widely used in the treatment of functional swallowing disorders.
In some cases, elimination of dysphagia is only possible through surgery. For neoplasias that cover the lumen of the esophagus or compress it, resection or removal of the pathologically altered organ (removal of the stomach, lung) is performed, followed by radiation and chemotherapy.
Also, patients with Zenker's diverticulum can only be treated in surgery; timely cricopharyngeal myotomy practically cures dysphagia.
For cicatricial narrowings of the esophagus that prevent the progression of the food coma, the following is used:
- bougienage;
- endoscopic dissection of strictures;
- stenting.
If dysphagia cannot be eliminated, the patient is given a nasogastric tube or a gastrostomy tube.
The main clinical recommendations concern the correction of the diet, the replacement of solid foods with soft foods.
Hypersecretory disorders require diet and a special lifestyle.
For neurological pathologies, a number of techniques have been developed to improve oral swallowing. The speech therapist selects individual methods for each individual patient during the rehabilitation period.
Massage and hydrotherapy
Patients with dysphagia are advised to undergo general massage. It is especially useful to work on the areas of the neck, chest and back. It is better to massage in the middle of the sternum, along the spinal segments and along the intercostal space. Water procedures also provide positive dynamics in the treatment of dysphagia. Warm baths with pine needles, wet wraps, chest compresses - all this will be a good help in treating the disease.
Prevention of the disease consists of the following measures: timely diagnosis and treatment; a balanced diet, which involves avoiding fatty, fried, canned and too hot foods, fast food, fizzy drinks, smoking, alcohol, introducing vegetables, fruits, and herbs into the diet.
Speech therapy massage
Therapeutic massage is widely used in medicine, both in adults and children. In neurology, it is used for pathologies of the central and peripheral nervous system.
Speech therapy massage is one of the types of therapeutic massage. It is carried out using a special probe with various attachments. Special techniques have been developed for this type of massage. The efforts of the logopath are aimed at:
- to normalize muscle tone, relieve spasms of facial and chewing muscles;
- improvement of blood circulation, metabolic processes, nerve conduction.