Read more about what acute gastritis is
Gastritis is the most common pathology of the stomach. Every second adult suffers from various types of this disease. In the acute form of gastritis, inflammation usually affects the glandular layer of the stomach and the surface epithelium. Much less often, inflammation penetrates the entire mucosal layer and even the muscle layer.
The danger and insidiousness of this disease is that there is a risk of gastrointestinal bleeding, erosion of the mucous membrane, cicatricial transformations in the stomach, complications of a purulent-septic nature, and the transition of acute gastritis to a chronic form. Various forms of acute gastritis are also present in children of primary school age.
Acute gastritis recommendations for every day
Gastritis is considered a fairly common disease and therefore methods of its treatment are well known. If patients adhere to certain recommendations from doctors, then the course of the inflammatory process in the gastric mucosa will be “eased.” What patients with diagnosed gastritis need to remember:
- Try not to violate your diet - there should be at least 5 meals per day.
- If you are forced to consume “forbidden” foods (it was a holiday, you ate barbecue, etc.), then the next day reduce the aggressive effect on the mucous membranes - the menu should include pureed soups and broths.
- Drink mint and lemon balm teas regularly - they will not only correct your psycho-emotional state (nervousness and irritation can cause exacerbation of chronic gastritis), but also reduce the intensity of pain.
- If exacerbations of the chronic form of the inflammatory process in question occur in spring and autumn, then when the first signs of the pathological process appear, you can take a course of Ranitidine (10 days, 2 tablets per day).
- Go for preventive examinations with your doctor at least 2 times a year - this will reduce the risk of developing gastric ulcers significantly.
- During periods of exacerbation of inflammation, it is better not to exercise.
It is very important to realize that this disease, which occurs in a chronic form, is incurable and therefore some restrictions and prohibitions will have to be observed throughout your life. But this does not mean that the lifestyle will be radically changed - people diagnosed with gastritis are not prohibited from playing sports, having children, or engaging in extreme labor.
Sources
https://healthperfect.ru/ostryy-gastrit-simptomy-i-lechenie.html
https://hudey.net/pravila-pitaniya-pri-erozivnom-gastrite.html
https://gastryt.ru/gastrit/gastrit-rekomendacii.html
https://gigastroi.ru/ostryj-gastrit-klinicheskie-rekomendacii/#i-9
Pathogenesis and etiology of the disease
According to the etiological mechanism of formation, acute gastritis is divided into endogenous and exogenous.
The occurrence of acute endogenous gastritis depends on the presence of infections in the body. The main reason is the presence of the bacterium Helicobacter pylori, which is detected in 80% of patients diagnosed with acute gastritis. Helicobacter bacteria secrete various toxins, under the influence of which inflammatory reactions begin to develop in the gastric mucosa. This bacterium also contributes to the appearance of gastric ulcers.
Less commonly, the causative agents of gastritis of the endogenous mechanism (infectious, for example) are staphylococci, streptococci, Escherichia coli, Proteus, causative agents of fungal infections, cytomegalovirus, and others. Functional and morphological prerequisites for the appearance of this type of gastritis occur with scarlet fever, influenza, viral hepatitis, measles, pneumonia, diphtheria. In some cases, acute gastritis of secondary etiology can occur with secondary syphilis or disseminated tuberculosis.
The etiological causes of acute exogenous gastritis are food agents - mechanical, thermal, chemical. Irritation of the mucous membrane by hot, rough, spicy food can cause the development of acute gastritis. They also have an adverse effect on the stomach and can act as irritants:
- dry food;
- poorly chewed food;
- overeating or an overly strict diet;
- eating a large amount of spicy, fried, salty, smoked foods and food seasoned with vinegar, pepper, mustard.
Frequent consumption of alcohol, strong coffee, and smoking have a damaging effect on the mucous membrane of the digestive organ.
Exogenous causes often include food poisoning, which is caused by eating foods contaminated with Shigella, Salmonella, Yersinia, and Klebsiella. Also, damage to the mucous membrane and its irritation can be provoked by prolonged use of certain medications - sulfonamides, glucocorticoids, salicylates, iron preparations, bromides, antibiotics.
Acute gastritis can manifest itself against the background of radiation therapy in the treatment of gastric oncology (radiation gastritis), accidental (or intentional) penetration into the stomach of chemicals (compounds of iodine, acetone, arsenic, nitric, phosphoric, sulfuric, acetic, hydrochloric acids, ammonia, caustic soda and others). With large concentrations or volumes of toxic substances entering the body, a burn may occur or perforation of the wall of the esophagus and stomach may develop.
Acute allergic gastritis can develop due to personal intolerance to certain types of foods and may be accompanied by other allergic reactions - angioedema, urticaria, an attack of bronchial asthma.
Damage or inflammation of the mucous membranes is also caused by frequent endoscopic examinations, the study of gastric secretion with the support of probes and pH meters. Mechanical damage to the walls of the stomach is also undesirable - injuries from blows, bruises, intense physical activity or foreign objects entering the stomach (poultry bones, fish, chips, needles).
Stress, neuroses, and depressive disorders are also considered risk factors.
Etiology and pathogenesis of the disease
The causes of the development of chronic gastroduodenitis can be divided into endogenous (internal) and exogenous (external).
Endogenous include:
- pathologies of the gastrointestinal tract (increased acidity of the digestive organ, decreased amount of mucus produced, disruption of hormonal regulation of digestion and reparative processes);
- damage to the pancreas, liver;
- endocrine disorders.
External reasons include:
- eating excessively spicy, hot or cold foods, large amounts of food that contain dyes, pesticides and preservatives, drinking alcohol, strong coffee and tea.
- presence of the bacteria Helicobacter pylori in the body.
When the cause of pathology is diseases of internal organs, this indicates a secondary form of pathology. When the formation of the disease is influenced by external factors or an unhealthy diet, a diagnosis of “primary gastroduodenitis” is made.
With the development of secondary chronic gastroduodenitis, the presence of gastric ulcer, chronic gastritis, pancreatitis, hepatitis, allergic and parasitic diseases, chronic renal failure, and pathology of the cardiovascular system can be identified.
The secondary form can be provoked by the following factors:
- constant stress;
- malfunction of the nervous system;
- poor immunity;
- use of antibiotics;
- presence of intestinal infections.
Infectious diseases can also contribute to inflammation of the mucous membrane. Sometimes the chronic form occurs with reflux syndrome, when bile is thrown into the stomach.
The primary form can be caused by:
- exposure to poisons and chemicals;
- unhealthy diet and irregular diet;
- bad habits - excessive drinking and smoking;
- eating too hot or cold food.
Heredity also plays a significant role in the development of the disease.
To establish the causes contributing to the appearance of chronic gastroduodenitis, the classification of chronic gastritis is used:
- Type A. It appears as a result of autoimmune disorders in the body, proceeds with a tendency to atrophy, usually of the mucous membranes of the stomach, then the duodenum. A characteristic symptom is a decrease in hemoglobin.
- Type B. An inflammatory process in the stomach appears as a result of an infectious lesion. In most cases, the causative agent is considered to be the bacterium Helicobacter pylori, and much less frequently (more often in children) - the Epstein-Barr virus and enterovirus. As a result of gastric metaplasia of the epithelium, inflammation of the duodenum occurs.
- Type C. It is called chemical or reactive. The causes of gastritis and duodenitis in this form are: consumption of alcohol, certain medications (antibiotics, NSAIDs, corticosteroids), smoking, poor diet, stress. These factors contribute to ulceration of the intestinal and gastric walls.
Classification of acute gastritis
With acute gastritis, various transformations can occur in the gastric mucosa, depending on which the disease can occur in various forms:
- catarrhal (simple, allergic, superficial, banal, alimentary gastritis);
- fibrinous;
- corrosive (necrotic);
- phlegmonous (purulent).
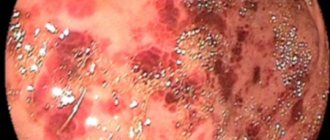
The catarrhal form of the pathology is characterized by thickening, plethora, swelling of the gastric mucosa, the presence of a large volume of mucus, and in some cases, superficial pinpoint hemorrhages may be present. In the presence of numerous erosions merging together, we can talk about acute erosive gastritis (at a later stage it turns into ulcerative). The microscopic picture of the pathology is characterized by dystrophy and desquamation of the epithelium of the surface layer, the presence of diffuse infiltration, and serous exudation.
The causes of catarrhal gastritis are:
- consumption of alcoholic beverages;
- acute infections;
- gross violations of proper nutrition;
- psycho-emotional or physical stress;
- irritating effects of drugs;
- food allergy - the presence in the diet of food with a high amount of allergen - mushrooms, strawberries, oranges, fish and other products.
The allergic form can be accompanied by various manifestations of dermatosis - rash, redness, Quincke's edema, etc. The first symptoms of this type of gastritis can occur immediately after an allergen enters the stomach.
In acute fibrinous gastritis, necrotic changes in the mucosa, the formation of fibrinous-purulent exudate and the appearance of a fibrous film on the surface of the stomach occur. Considering the depth of the inflammatory process, it is possible to distinguish between croupous (superficial) and diphtheritic (deep) gastritis.
The cause of fibrinous diphtheritic acute gastritis is considered to be a severe infectious disease:
- measles;
- scarlet fever;
- typhoid fever;
- sepsis.
Acute necrotizing gastritis occurs due to the entry of aggressive substances into the digestive organ. Acid intoxication causes coagulation necrosis, while salt poisoning provokes liquefaction necrosis. Not only the mucous layer of the digestive organ is damaged, but also the entire thickness of the gastric wall with the occurrence of erosions and perforated ulcers.
In acute phlegmonous gastritis, all layers of the wall of the digestive organ are involved in the inflammatory process - mucous, submucosal, serous, muscular. The purulent type of gastritis often appears with stomach injuries, ulcers, and disintegrating tumors. Against the background of this type of gastritis, perigastritis and peritonitis can occur.
Considering the area that is involved in the inflammatory process, one can distinguish:
- local (focal);
- widespread (diffuse) type.
The focal form of acute gastritis, taking into account the affected part of the stomach, is divided into:
- antral;
- fundamental;
- pyloroantral;
- pyloroduodenal form.
Acute gastritis nutritional recommendations
Compliance with the principles of dietary nutrition during the development of gastritis is the basis for the patient’s further recovery. It is important to prepare all dishes using the steam method, boil, stew, bake in the oven, for example, in a sleeve. Nutritionists do not recommend eating on an empty stomach; be sure to drink a glass of water or warm tea. If you have physical activity, add more protein in the first half of the day, try to avoid empty carbohydrates, and use vegetable fats instead of animal fats.
Nutritionists do not recommend eating on an empty stomach; be sure to drink a glass of water or warm tea. If you have physical activity, add more protein in the first half of the day, try to avoid empty carbohydrates, and use vegetable fats instead of animal fats.
With increased acidity
For gastritis with high acidity, it is important to reduce the activity of gastric juice production, and to do this, remove fiber, streaky meat, fish with cartilage, radishes, black bread with bran, and dried fruits from the diet. It is also necessary to avoid foods that stimulate juice production.
These are alcoholic drinks, caffeine, mushrooms, cabbage. Food should be consumed warm, excluding too cold or hot dishes. Allowed products for high acidity:
- dietary meat - rabbit, turkey, nutria, skinless chicken;
- river fish – pike perch, pike, carp, perch, catfish
- fatty milk - goat, sheep, cow;
- egg white; seafood;
- cereals - oatmeal, buckwheat;
- pureed boiled vegetables and fruits without skin; herbal teas, tinctures of medicinal plants.
To reduce the acidity of gastric juice, you need to categorically avoid any fermented milk products, it is important to minimize the consumption of baked goods, sweets, and give up onions and garlic. It is strictly forbidden to chew chewing gum, eat near the TV, or read a newspaper or book, in order to avoid overeating. You cannot follow strict dietary programs that contribute to the development of digestive tract disorders.
With low acidity
Basic postulates when following a diet with low acidity:
- exclude semi-finished products, spicy, salty, sweet, peppery, fried, fatty, sour foods;
- introduce boiled dietary meat and fish into the daily menu;
- fruits and vegetables must be heat-treated (stewing, steam method); the use of fermented milk products is allowed; use puddings, jelly, jelly as dessert;
- Drinks include lightly brewed tea, mineral water, diluted juices, herbal infusions.
After eating food, you need to rest for at least 15 minutes, if possible, take a lying or reclining position.
Symptoms of pathology
Signs of acute gastritis usually appear 6-12 hours after the onset of exposure to the etiological factor. The most common dyspeptic disorders are:
- heaviness and discomfort in the epigastric area;
- loss of appetite;
- constipation;
- moderate pain;
- presence of an unpleasant taste in the mouth;
- nausea;
- belching;
- vomiting of food; the vomit contains impurities of mucus and bile.
With food infections, flatulence, loose stools, and an increase in temperature are observed. Attacks of repeated vomiting and diarrhea can provoke dehydration of the body, which will manifest itself as headache, weakness, and dizziness.
Erosive gastritis is characterized by vomiting blood or the presence of streaks of blood in the stool, which indicate gastric bleeding.
With the phlegmonous type of gastritis, fever, vomiting mixed with pus, chills, and severe cramping pain in the upper abdomen are observed.
In acute corrosive gastritis, which is caused by the entry of chemicals into the body in high concentrations, repeated vomiting may occur, which does not bring relief; mucus and blood may be present in the vomit. Traces of a chemical burn may be present in the patient’s mouth and lips; when poisons penetrate the larynx, laryngospasm and asphyxia occur. The general condition is aggravated by the symptoms of shock: shallow breathing, tachycardia, hypotension, pale skin.
Acute gastritis during pregnancy and its prevention
Changes in hormonal levels, symptoms of toxicosis - nausea, vomiting - greatly worsen the condition of the mucous membrane of the digestive organ of the expectant mother. This pathology does not have a direct impact on the health of the unborn child, but to prevent complications, the pathology should be treated.
In pregnant women, factors that may be prerequisites for the appearance of acute gastritis are:
- Toxicosis.
- Violation of healthy eating rules.
- Stress.
- Excessive intake of vitamin complexes.
General prevention of the occurrence of acute gastritis and its complications consists of the prevention of toxicosis:
- complete cessation of bad habits;
- regular physical activity;
- following a diet;
- walks in the open air;
- controlling the psycho-emotional state;
- good sleep;
- At the first alarming symptoms, consult a doctor.
Medicines to relieve nausea are selected only by the supervising doctor.
Acute gastritis in children and its prevention
Attacks of gastritis can occur in children 5-6 and 9-12 years old. In a child, simple catarrhal acute gastritis can occur not only in the form of a malfunction of the stomach, but also in the form of poisoning of the entire body, disturbances in the functioning of the cardiovascular system. With frequent vomiting and diarrhea, the child’s body begins to suffer from dehydration, posing a threat of acute renal failure.
In a quarter of cases, the cause of pathology in schoolchildren is a violation of the diet. The following factors can provoke an attack of this form of gastritis:
- the beginning of puberty;
- an infection that entered the body through the mouth - failure to comply with hygiene rules, the habit of biting pens, pencils, nails;
- heavy emotional and physical stress.
The causes of the disease in children are the child’s feeding on “adult” foods – not according to age.
The treatment method is selected individually. Treatment includes gastric and intestinal lavage. Also, treatment of acute gastritis at home in children consists of:
- diets;
- compliance with bed rest;
- frequent warm drinks in small portions.
Prevention of acute gastritis in children consists of several features:
- complementary foods that are administered to babies must be freshly prepared;
- the transition to “adult” food should be gradual;
- It is recommended to teach your child to wash his hands before eating, after visiting the toilet, and after a walk;
- eat only washed vegetables and fruits;
- it is recommended to closely monitor psycho-emotional stress at school and at home;
- carry out timely sanitation of the child’s mouth.
Acute gastritis clinical guidelines
Diet for gastritis is the basis of therapy during exacerbation and maintenance of remission. Product composition and restrictions vary depending on the patient's condition. During an exacerbation, a strict diet for gastritis - switching exclusively to easily digestible foods in liquid form, dairy products, and low-fat broths. For severe exacerbations, 1-2 days of fasting is recommended. As the symptoms of the disease subside, the child is allowed a more varied diet - soups, cereals, tea.
The transition from strict restrictions during exacerbation to softer ones during remission occurs gradually.
Prevention measures:
Diet for gastritis is the basis of therapy during exacerbation and maintenance of remission.
Improper nutrition for acute gastritis is the root cause of its appearance. Make sure to comply with the shelf life of food, limit the consumption of seasonings, fatty, fried, smoked foods, and fast food.- Timely treatment of infectious diseases.
- Maintain personal hygiene (wash your hands often, brush and treat your teeth regularly).
- Eat only washed fruits and vegetables; meat and fish must undergo long-term heat treatment.
- When taking medications, do not give up prebiotics.
- Stop smoking and alcohol.
- If you have already been diagnosed with gastritis, regularly visit a gastroenterologist and follow his recommendations.
- Control your psycho-emotional state.
- Walk more often and lead a healthy lifestyle.
- At the first symptoms, consult a specialist; do not self-medicate.
Diagnosis of acute gastritis
To make a diagnosis, the doctor examines the patient, ascertains the medical history, clarifies concomitant pathologies, and palpates the epigastric region, where painful manifestations are felt during palpation. When examining the oral cavity, a grayish coating is noticeable on the tongue, and there is an unpleasant odor from the mouth.
Diagnostic methods that are used to make a diagnosis are as follows:
- analysis of urine, blood, feces;
- coprogram;
- breath test for the presence of the bacterium Helicobacter pylori;
- gastroscopy;
- endoscopic biopsy;
- X-ray of the stomach;
- plain radiography and MSCT of the abdominal organs (for phlegmonous gastritis);
- Ultrasound.
Differential diagnosis is needed to exclude diseases that have similar symptoms: gastralgic form of myocardial infarction, pancreatitis, appendicitis, cholecystitis.
Treatment of pathology
In case of acute gastritis, fasting is recommended in the first day or two, after which a diet is prescribed. In case of chemical or food poisoning, gastric lavage is done as first aid. Also stop taking medications that irritate the stomach, stop smoking and drinking alcohol.
Drug treatment involves the use of H2-histamine receptor blockers that have an antisecretory effect (Cimetidine, Ranitidine, Famotidine), antacids (aluminum hydroxide, magnesium oxide, aluminum phosphate, magnesium carbonate), proton pump inhibitors (Omeprazole "and its analogs), gastroprotectors (bismuth preparations).
For gastritis of a specific etiology, clinical recommendations include the appointment of appropriate treatment - antifungal, anti-Helicobacter, anti-tuberculosis therapy.
To relieve pain, the following painkillers are used: Papaverine, Atropine, Platifillin; for vomiting, prokinetics are used - Metoclopramide, Domperidone. In case of severe dehydration, infusion therapy with saline solutions is performed.
Treatment of phlegmonous acute gastritis is carried out surgically: gastrotomy is performed, drainage of the purulent focus, in some cases gastrectomy or gastrectomy is performed.
Nutrition
Following a diet for pathology is an obligatory stage not only in the treatment process, but also in subsequent life. During the treatment period, food is limited, after which the usual regimen is gradually introduced, but the dishes should be pureed.
After treatment, the patient must carefully follow the rules of a healthy diet, and not eat unhealthy, spicy or fatty foods.
During the first 2-4 days of therapy, the patient should refrain from eating. After this, it is necessary to ensure that food does not burden the weakened gastrointestinal tract. Meals should mainly consist of boiled or steamed dishes. Spices are strictly excluded, salt consumption is limited.
Dishes allowed for acute gastritis:
- Lean meat (veal, turkey, rabbit, chicken).
- Porridge on the water.
- Boiled potatoes (no more than 1-2 servings per week).
- Soup with cereals in vegetable broth.
- Tea with chamomile, rosehip, jelly.
With high acidity, it is allowed to eat: milk, boiled eggs, natural yoghurts, kefir.
With low acidity, low-fat cottage cheese and kefir are allowed.
Chronic gastroduodenitis
Diet therapy
Treatment of chronic gastroduodenitis is usually long-term and includes several stages, sequentially following each other.
Treatment begins with the appointment of a special diet. Meals include pureed porridge in meat, vegetable or mushroom broth; lean meats and fish; vegetables and fruits, dairy products; bakery products (excluding baked goods). Food preparation can be varied (steamed, boiled, stewed, baked); Freshly squeezed juices are allowed. Even milk is allowed if it does not have a laxative effect. The diet must include foods rich in vitamins B1, B2, PP, C. There should be at least five meals per day. Food should be eaten warm, chewed thoroughly, and in small portions.
In the acute period, bed rest is required for at least seven to eight days. If you adhere to a diet, this allows you to reduce the intensity of the inflammatory process and pain.
Pharmacotherapy
Considering the high frequency of detection of Helicobacter pylori infection in chronic gastroduodenitis, eradication of the pathogen is carried out according to a certain scheme, which is selected based on the severity of the disease:
- bismuth preparation, metronidazole and tetracycline antibiotic for one to two weeks
- Metronidazole, clarithromycin, omeprazole for a week
- Ranitidine, amoxicillin, metronidazole for 10-14 days
To prescribe or correct the most effective treatment regimen, a second consultation with a gastroenterologist may be required. For increased acidity, H2-histamine receptor blockers (cimetidine, ranitidine, famotidine), proton pump inhibitors (omeprazole, lansoprazole, pantoprazole, rabeprazole, esomeprazole), antacids (aluminum hydroxide, magnesium hydroxide, aluminum phosphate, magnesium carbonate), gastroprotectors (bismuth) are used , sucralfate). Complex treatment necessarily includes prokinetics and enzymes.
Non-drug therapy
Of great importance in the treatment of chronic gastroduodenitis is sanatorium-resort and balneological treatment, physiotherapeutic measures, moderate physical activity and physical therapy. Herbal medicine is also widely used (decoctions of chamomile, string, plantain, mint, yarrow, St. John's wort, valerian).
Pathology prognosis
With proper and timely treatment, acute catarrhal gastritis ends in a few days with recovery. The prognosis for acute corrosive gastritis is unfavorable: the patient may die from peritonitis, shock, or gastric perforation.
An unfavorable prognosis is possible in acute phlegmonous gastritis, when the appearance of mediastinitis, pleural empyema, purulent peritonitis, sepsis, gastric perforation, and liver abscess cannot be ruled out.
Video on the topic:
Prevention
Preventive measures for all forms of acute gastritis are associated with following food hygiene and sanitary hygiene:
- compliance with the terms and conditions of food storage;
- oral hygiene - treatment of dental diseases, teeth cleaning;
- limiting the use of seasonings, fried, fatty foods, heavy foods;
- timely treatment of various infectious diseases;
- eating washed vegetables and fruits.
It is also necessary to monitor the stomach’s reaction to drug therapy, be attentive to the psycho-emotional state - avoid stress, and maintain the body’s immunity.
List of references: https://ru.wikipedia.org/wiki/Gastritis https://www.nrmed.ru/rus/dlya-vzroslykh/gastroenterologiya/gastrit/ https://www.gmsclinic.ru/diseases/gastritis https ://www.smed.ru/guides/43945/doctor/ https://medportal.ru/enc/gastroenterology/gastritis/3/ https://www.kp.ru/guide/kak-lechit-gastrit.html https://www.kp.ru/guide/simptomy-i-priznaki-gastrita.html https://www.obozrevatel.com/health/bolezni/ostryij-gastrit.htm https://aif.ru/health/ leksprav/gastrit_prichiny_simptomy_i_lechenie https://policlinica.ru/ostryy-gastrit.html https://atvmedia.ru/materials/ostryj-gastrit-prichiny-simptomy-i-lechenie med.vesti.ru/articles/zabolevaniya/gastrit-ostraya -i-hronicheskaya-formy/ med.vesti.ru/articles/zabolevaniya/gastrit-simptomy-i-lechenie-u-vzroslyh/ crb-bel.ru/gastritis/ Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/31/2020
Acute gastritis in children clinical recommendations
The child is prescribed a diet with limited spicy foods and foods that increase acidity.
Diet for gastritis is the basis of therapy during exacerbation and maintenance of remission. Product composition and restrictions vary depending on the patient's condition. During an exacerbation, a strict diet for gastritis - switching exclusively to easily digestible foods in liquid form, dairy products, and low-fat broths. For severe exacerbations, 1-2 days of fasting is recommended. As the symptoms of the disease subside, the child is allowed a more varied diet - soups, cereals, tea.
The transition from strict restrictions during exacerbation to softer ones during remission occurs gradually.
During remission, the main task of the diet is to prevent another exacerbation. The child is prescribed a diet with limited spicy foods and foods that increase acidity. Cereals, dairy products, potatoes, bread and pastries in moderate quantities, and sweet fruits are allowed. You need to limit or exclude all sour vegetables and fruits - sour apples, lemons. It is advisable not to overuse spices.
The diet is important - the entire daily diet is divided into small meals, as with other gastrointestinal diseases - enteritis, gastrointestinal tract diseases, gallbladder diseases. More or less equal intervals should be observed between meals. Complete prevention of exacerbations involves eliminating stress. Parents need to reconsider their child's schedule and reduce the workload.
Drug therapy has several goals - protecting the gastric mucosa, reducing the acidity of gastric juice, suppressing the activity of Helicobacter and alleviating the patient's condition. Therefore, complex therapy is prescribed.
Drug treatment follows several regimens, which include antibiotics against Helicobacter, drugs that reduce the production of acid in the stomach and drugs that protect the gastric mucosa. Treatment regimens prescribed for children differ from those for adults.
List of active ingredients allowed for children and adolescents:
- anti-Helicobacter drugs: Metronidazole, Clarithromycin;
- acidity reducing agents: Ranitidine;
- gastroprotectors: De-nol, Almagel;
- products that improve gastrointestinal motility: No-spa, Cerucal.
Only a specialist can select a treatment regimen; parents should not do this on their own.
NSAIDs are excluded from treatment regimens, including drugs that are used to relieve fever during ARVI . These medications have two harmful effects on the stomach - they increase acid production, and most of them are chemically acidic. NSAIDs are not prescribed during the acute stage. During remission, the dosage of such drugs is strictly limited. The same applies to steroidal anti-inflammatory drugs and other drugs with an ulcerogenic effect.
The child needs to be taught food hygiene, as well as following a number of rules that will help him maintain health in the future:
- eating small portions;
- moderation in seasonings and salt;
- moderate fat and sweet content;
- sufficient fluid intake.
These recommendations will help prevent gastritis, biliary tract diseases, hepatitis A, and intestinal diseases.