- Causes and risk factors
- Species and types
- Symptoms
- Stages of the disease
- Diagnostic methods
- Early diagnosis in Belgium
- Treatment
- Forecast criteria
A malignant tumor of the cecum is a special case of colorectal cancer with all its inherent features of the course, diagnosis and treatment.
However, the localization of cancer in the area of the cecum also has its own characteristics. This type of colorectal cancer is usually detected at a later stage and behaves more aggressively compared to malignancies in other parts of the large intestine.
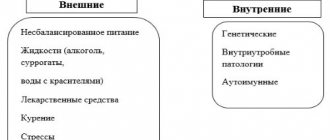
Reasons for tumor formation
Many lifestyle factors influence the risk of developing cecal cancer.
Overweight or obesity
Being overweight (especially with a large waist circumference) increases the risk of colon cancer in both men and women, but the association appears to be stronger in men.
Physical inactivity
Physical inactivity is associated with a greater likelihood of developing colon cancer, and therefore the cecum.
Certain types of diets
A diet high in red meat (eg, beef, lamb, or liver) and processed meat (eg, smoked meat, sausage) increases the risk of developing colorectal cancer.
Cooking meat at very high temperatures (frying or grilling) creates chemicals that can increase the risk of cancer.
Smoking
People who smoke tobacco for a long time are more likely than non-smokers to develop and die from colorectal cancer. Smoking is a well-known cause of lung cancer, but it is also associated with many other types of cancer.
Alcohol abuse
Right-sided colon cancer is significantly associated with alcohol consumption. Limiting alcohol consumption can have many health benefits, including reducing the risk of many types of malignant neoplasia.
Colon polyps
This is especially true if the polyps are large, if there are many of them, or if any of them have dysplasia.
Inflammatory bowel diseases
Diseases such as ulcerative colitis or Crohn's disease greatly increase the risk of developing cecal cancer.
How does a benign tumor develop?
The glandular epithelium of the colon in the epithelial form degenerates in a multi-stage process as a result of genetic changes. Initially, a benign tumor appears - an adenoma, which is noticeable as a colon polyp during colonoscopy. However, adenoma cells are sensitive to further gene mutations, so cancer cells eventually arise that quickly divide and grow into the surrounding tissue. More than 90% of colorectal carcinomas are caused by adenomas, so removing them is a doctor's first priority. Neuroendocrine tumors are a rare group of neoplasms that originate from cells of the diffuse neuroendocrine system. The most common localization of neoplasia is the cecum and lower ampullary rectum.
Types of cecal cancer
Adenocarcinomas account for about 96% of cecal cancers. These tumors begin in the cells of the mucous glands of the large intestine. When doctors talk about colorectal cancer, they almost always talk about this type of tumor. Some subtypes of adenocarcinoma, such as signet ring cell and mucinous, may have a worse prognosis.
Other types of cecal tumors are much less common.
- Carcinoid tumors. They begin in the endocrine hormone-producing cells of the large intestine. These are slow-growing tumors with little malignant potential.
- Gastrointestinal stromal tumors (GISTs) develop from special cells in the wall of the colon called interstitial cells of Cajal.
- Lymphomas are cancers of immune system cells. They mostly start in the lymph nodes, but can also develop in the large intestine.
- Sarcoma can start in the blood vessels, muscle layers or other tissues in the wall of the large intestine. Sarcomas of the colon and, especially, the blind are extremely rare.
Types and stages of disease development
There are several types of cancer:
- The most common type is adenocarcinoma. In this case, the tumor is formed from damaged cells of the mucous membrane, and consists of benign and malignant cells.
- Glandular cancer. The tumor develops from glandular epithelial cells and is exclusively malignant.
- Signet ring cell carcinoma. A malignant tumor has the form of small vesicles that give extensive metastases to other organs.
- Sometimes so-called squamous cell carcinoma occurs. In this case, the malignant neoplasm affects the cells of the squamous epithelium, but over time the tumor also invades other areas of the cecum.
- Undifferentiated cancer is rare. It is a malignant neoplasm that arose from several tumors of different types (for example, from adenocarcinoma and signet ring cell tumor).
- In very rare cases, unclassified cancer occurs. This diagnosis is made if the tumor develops atypically, and the neoplasm does not resemble any of the known tumors.
The disease usually develops in four stages:
| Stage | Description |
| 1 | The tumor is small in size (up to 20 mm) with clear edges. There is no metastasis. |
| 2 | Cancer has increased dimensions (up to 30 mm), the boundaries of the tumor can be clear or blurred. There may be small metastases in the lymphatic system or liver. |
| 3 | The neoplasm is large in size (40 or more millimeters), the boundaries of the tumor are blurred in most cases. A large number of metastases can be observed in the liver, lymphatic system and stomach. |
| 4 | The tumor is large; the boundaries are blurred. There are many metastases in many organs (liver, stomach, kidneys, spinal bones, lymphatic system and some other organs). |
Signs of the disease
Physical examination findings may be very nonspecific (eg, fatigue, weight loss) or normal in the early stages of cecal cancer.
The main symptoms develop already in the advanced stages of the disease, when the cancer has already spread beyond the intestines.
Cecal cancer - symptoms and signs in late stages:
- abdominal pain;
- macroscopic rectal bleeding;
- palpable abdominal mass;
- hepatomegaly;
- ascites.
Complications
The first complication that the patient encounters is anemia. This condition develops against the background of frequent bleeding and spotting from the affected area of the intestine. Anemia leads to weakness and increased fatigue.
When the tumor reaches a large size, intestinal obstruction occurs. This process requires immediate surgical intervention. However, the most dangerous consequence of intestinal blastoma is metastasis.
The disease rapidly progresses, due to which the neoplasm spreads to neighboring organs that are essential for the body. Sometimes the affected cells travel through the blood or lymph to distant systems, causing new blastomas there.
Stages
| Stage | Determination by TNM | Description |
| 0 | Tis N0 M0 | Cancer is at its earliest stage. This stage is also known as carcinoma in situ or intramucosal carcinoma (Tis). The tumor has not grown beyond the inner layer (mucosa) of the colon. |
| I | T1 or T2 N0 M0 | The cancer has grown through the mucosa into the submucosa (T1), and it can also grow into the muscularis propria (T2). It has not spread to nearby lymph nodes (N0) or distant lymph nodes (M0). |
| IIA | T3 N0 M0 | The tumor has invaded the outermost layers of the colon but has not invaded the peritoneal cavity (T3). It has not spread to nearby lymph nodes (N0) or distant sites (M0). |
| IIB | T4a N0 M0 | The tumor has grown through the wall of the colon into the abdominal cavity but has not invaded adjacent tissues or organs (T4a). It has not yet spread to nearby lymph nodes (N0) or distant organs (M0). |
| IIC | T4b N0 M0 | The tumor has grown through the wall of the intestine and has attached to or invaded other nearby tissues or organs (T4b). It has not yet spread to local lymph nodes (N0) or distant sites (M0). |
| IIIA | T1 or T2 N1/N1c M0 | The cancer has grown through the mucosa into the submucosa (T1), and it can also grow into the muscularis propria (T2). It has spread to 1-3 nearby lymph nodes (N1). Or there is damage to the fatty tissue near the lymph nodes, but not on the nodes themselves (N1c). No spread to distant organs (M0). |
| T1 n2a M0 | The tumor has grown through the mucosa into the submucosa (T1). It has spread to 4-6 nearby lymph nodes (N2a). It has not spread to distant sites (M0). | |
| IIIB | T3 or T4a, N1/N1c M0 | The cancer has grown into the outermost layers of the bowel (T3) or through the visceral peritoneum (T4a), but has not reached nearby organs. It has spread to 1-3 regional lymph nodes (N1a or N1b). It has not spread to distant sites (M0). |
| T2 or T3 n2a M0 | Growth of the tumor into the muscle layer itself (T2) or into the outer layers of the colon (T3). The tumor has spread to 4-6 regional lymph nodes (N2a). It has not spread to distant sites (M0). | |
| T1 or T2 N2b M0 | The tumor has grown through the mucosa into the submucosa (T1), and it can also grow into the muscularis propria (T2). It has spread to 7 or more local lymph nodes (N2b). It has not spread to distant sites (M0). | |
| IIIС | T4a n2a M0 | The cancer has grown through the wall of the colon or rectum (including the visceral peritoneum) but has not reached nearby organs (T4a). It has spread to 4-6 local lymph nodes (N2a). It has not spread to distant sites (M0). |
| T3 or T4a N2B M0 | The cancer has grown into the outermost layers of the colon or rectum (T3) or through the visceral peritoneum (T4a), but has not reached nearby organs. It has spread to 7 or more nearby lymph nodes (N2b). It has not spread to distant sites (M0). | |
| T4b N1 or N2 M0 | The tumor has grown through the wall of the colon or rectum and has attached to or grown into other nearby tissues or organs (T4b). It has spread to at least one regional lymph node. | |
| IVA | Any T Any N M1a | Cancer may or may not grow through the wall of the colon or rectum (either T). This may or may not have spread to nearby lymph nodes. (Any N). It has spread to 1 distant organ such as the liver or lung (M1a). |
| IVB | Any T Any N M1b | The cancer has spread to more than 1 distant organ, such as the liver or lung (M1b). |
| IVC | Any T Any N M1c | The cancer has spread to distant parts of the peritoneum (the lining of the abdomen) and may or may not have spread to distant organs or lymph nodes (M1c). |
Innovative diagnostic methods used in clinics in Belgium
Virtual colonoscopy (CT colonography) is a method of non-invasive visualization of the mucous membrane of the large intestine by constructing a three-dimensional computer model. Its diagnostic value approaches that of conventional colonoscopy, without causing any discomfort to the patient.
PET-MRI is a hybrid of magnetic resonance imaging and positron emission tomography. The method allows you to obtain a detailed image of the intestine with visualization of areas of abnormally increased metabolism (cancer tumor).
Treatment methods
Surgery is the only curative treatment for localized cecal cancer (stage I-III).
Surgical resection is also potentially considered as the primary treatment option for patients with limited metastatic disease to the liver and/or lung (stage IV disease). But the appropriate use of elective colon resections in uneventful patients with stage IV disease remains a source of ongoing debate.
Adjuvant chemotherapy is the standard treatment for patients with stage III disease. Its use in stage II remains controversial, and ongoing research is seeking to confirm which markers can identify patients who may benefit from it.
Currently, the role of radiotherapy is limited to palliative therapy for selected metastatic sites, such as bone or brain metastases.
Biological agents have assumed a major role in the treatment of metastatic cases, with selection increasingly determined by genetic analysis of the tumor.
Chemotherapy
Drugs commonly used to treat colorectal cancer include:
- 5-fluorouracil (5-FU);
- Capecitabine (Xeloda);
- Irinotecan (Camptosar);
- Oxaliplatin (Eloxatin);
- Trifluridine and tipiracil (Lonsurf).
In most cases, 2 or more of these drugs are combined, making the treatment more effective. When diagnosed with cecal cancer, stage IV treatment is often carried out with complex therapy, which includes, in addition to 2-3 chemotherapy drugs, also a drug for targeted therapy.
Targeted therapy
Vascular endothelial growth factor (VEGF) is a protein that helps tumors form new blood vessels (a process known as angiogenesis) to obtain the nutrients they need to grow. Drugs that stop VEGF from working can be used to treat some types of cecal cancer.
These are the drugs:
- Bevacizumab (Avastin®);
- Ramuchirumab (Kiramza®);
- Ziv-aflibercept (Zaltrap®);
Pembrolizumab (Keytruda ®) and Nivolumab (Opdivo ®) are drugs that target PD-1, a protein in immune system cells that normally keeps those cells from attacking other cells in the body. By blocking PD-1, these drugs enhance the immune response against cancer cells.
Side effects of these drugs may include fatigue, cough, nausea, itching, skin rash, decreased appetite, constipation, joint pain, and diarrhea.
Ipilimumab (Yervoy ®) is another drug that enhances the immune response, but it has a different purpose. It blocks CTLA-4, another protein in T cells that normally blocks their activity.
This drug is used with Nivolumab (Opdivo®) to treat cancer of the cecum
Other types of polyps
The shape or rough texture is also clinically significant. Polyps with a stalk are called “footed”, and without it - “sessile”. Some precancerous growths are now recognized as flat rather than raised. Such nonpolypoid neoplasia is more common in the setting of chronic colitis and may be more easily detected using non-conventional endoscopic imaging techniques. Polyposis syndromes are inherited conditions that include:
- familial adenomatous, hyperplastic polyposis;
- hereditary nonpolyposis colorectal cancer;
- Gardner's syndrome;
- Turkota;
- Poitz-Yeghers;
- MutYH-associated polyposis;
- Cowden's disease.
Progress has been made in understanding some of the genetic factors that contribute to the development of the above conditions. Some of them have extraintestinal features. Familial adenomatous polyposis is best understood in terms of its genetic basis. Gamaromatous polyps, consisting of a mixture of normal tissue and inflammatory polyps, are more common in the context of colitis.
Forecast
The prognosis for cancer of the cecum is always more serious than for other special cases of colon cancer. In general, right-sided colorectal cancer, which includes tumors of the cecum, is associated with a higher mortality rate than left-sided colorectal cancer. But even among right-sided tumors, cecal neoplasms are the most serious in terms of overall survival.
So, with a diagnosis of stage 3 cecal cancer, the prognosis will be extremely unfavorable with a five-year survival rate below 30%.
The overall five-year survival rate, depending on the extent of the disease, looks like this:
- localized disease: 79.9%;
- regional disease: 51.3%;
- metastatic disease: 10.2%.
Find out more about early diagnosis and modern treatment options for cecal cancer in Belgium. Write to us or request a call back.
Diagnostics
The preliminary diagnosis of “cecal cancer” is established by specialists at the oncology clinic during the collection of complaints and anamnesis, and clinical examination. A large tumor can be detected during palpation of the abdomen. For the purpose of differential diagnosis, to clarify the location, shape and size of the tumor, and to identify metastases, additional research methods are carried out:
- Colonoscopy;
- Irrigoscopy;
- Computed tomography;
- Ultrasound screening;
- Diagnostic laparoscopy.
During an endoscopic or laparoscopic examination, doctors necessarily select material for histological analysis, which allows them to come to unambiguous diagnostic conclusions. The most informative method for diagnosing sigmoid colon cancer is rectoscopy. With sigmoidoscopy, up to 25 cm of the distal colon is examined.
The use of a flexible sigmoidoscope and colonoscope allows for more accurate preoperative diagnosis of cecal cancer. The X-ray method using a double contrast enema has great sensitivity. It allows you to detect small tumors. A malignant neoplasm manifests itself in the form of a characteristic narrowing or compaction, which is located in the contrast zone. In doubtful cases, doctors at the Yusupov Hospital repeat the examination or perform a colonoscopy.
Scanning computed tomography with air contrast is becoming increasingly widespread. This method is used when making a final decision about the need for surgical intervention. At the Yusupov Hospital, spiral computed tomography with a small slice thickness, the so-called “virtual colonoscopy,” is widely used to detect cancer of the cecum.
Colon carcinoma cells produce carcinoembryonic antigen (CEA), a tumor marker for cancer. However, it is not specific enough to serve as a reliable indicator of the existence of a tumor. Carcinoembryonic antigen is also found in pancreatitis, inflammatory bowel processes, in smokers and in people who abuse alcohol. The CEA test is used in patients with initially high levels of this tumor marker after surgery. Its level decreases after successful surgery, and an increase in CEA concentration in the postoperative period may be the first sign of tumor relapse.
Doctors at the Yusupov Hospital carry out differential diagnosis of cecal cancer with the following diseases:
- Diverticulosis of the colon;
- Ulcerative and ischemic colitis;
- Irritable bowel syndrome.
Other diseases manifested by rectal bleeding (hemorrhoids, polyposis) make diagnosis difficult. Pain in the right half of the abdomen may indicate the development of acute appendicitis. If the patient has positive symptoms of an “acute abdomen,” he undergoes urgent surgery, during which the true cause of the pain syndrome is determined.
Tubular adenoma of the cecum is a benign neoplasm. It may present with symptoms that resemble those of a cancerous tumor.
Make an appointment