Esophageal candidiasis is a lesion of the digestive tract by yeast-like microorganisms.
This type of thrush is characterized by the colonization of the microflora of the esophagus by fungi from the genus Candida. Gastroenterologists noted that every year the number of diseases of the gastrointestinal tract is increasing, and the leading place among them is occupied by mycotic lesions of the esophagus, or, more simply, candidiasis. This disease manifests itself in patients with reduced protective functions of the body, HIV-positive patients or people who have undergone organ transplantation operations.
Also at risk are those who uncontrollably take antibiotics. Diet for esophageal candidiasis and the use of medications play a key role in treatment.
Reasons for development
The esophageal tube can be affected in two ways - descending and ascending. In the esophagus, the fungus begins to multiply intensively and attack the mucous membrane, thereby provoking the manifestation of characteristic symptoms. It is also worth noting that other organs of the gastrointestinal tract can be affected simultaneously with the esophageal tube. Candidiasis can begin to progress after:
- eating food products on which the fungus is located;
- close contact with a patient whose candidiasis is progressing;
- using hygiene items that may contain fungal microorganisms.
It is worth noting that esophageal candidiasis will begin to develop only if conditions are favorable for this. The main factor is a decrease in the level of the body's immune defense. If both local and general immunity decreases, then fungi begin to actively multiply and infect the mucous membrane of the organ. Other factors that can also cause the progression of the disease include the following:
- a history of diabetes mellitus;
- traumatization of the walls of the esophagus by too hard food, hot or cold dishes, chemicals;
- symptoms of esophageal candidiasis often appear after long-term treatment with antibacterial drugs for another ailment;
- malnutrition;
- parenteral nutrition;
- intoxication of the body;
- administration of inhaled corticosteroids;
- dysfunction of the parathyroid glands and adrenal glands;
- decreased acidity of gastric juice;
- organ or bone marrow transplantation;
- carrying out antacid therapy over a long period of time;
- impaired motility of the esophagus and gastrointestinal tract;
- insufficient intake of proteins from food into the human body;
- immunodeficiency state of physiological type. This group includes the gradual aging of the human body, the period of bearing a child, as well as childhood;
- formation of oncology in the body;
- allergic diseases;
- carrying out chemotherapy and radiation therapy;
- dysbiosis of mucous membranes.
It is also worth highlighting a group of local risk factors for the development of the disease. These include the formation of polyps, achalasia, and mucosal burns.
How does the fungus get into the esophagus?
Microorganisms of the genus Candida, capable of causing esophageal fungus and other diseases (oral cavity, genitourinary system, internal organs, skin and nails), are constantly present on the mucous membranes inside the body or are ingested with food, through direct contact with the carrier (for example, through a kiss) .
With candidiasis of the esophagus, the main source of fungal infection becomes the intestines, from where it “rises” upward through the digestive tract and stomach (ascending route of infection).
Structure of the gastrointestinal tract. Click on photo to enlarge
At the same time, the nearest mucous membranes are actively colonized by fungi that enter from the oral cavity (with vegetables and fruits, sweet dairy products, etc.) (descending path).
Under normal conditions, the body's immune defense restrains the pathogenicity of the microorganism (its ability to grow and reproduce, invade host tissues), in favorable conditions for the fungus, any number of cells can attach to the mucous membrane and form a colony, a focus of candidiasis.
Symptoms
In the early stages of the onset of the disease, it is difficult to diagnose, since the symptoms of the disease are very mild. The only thing that can signal candidiasis is a sharp decrease in appetite and general malaise that develops against the background of metabolic disorders. Many people may not even be aware of the disease, especially if they have an immunodeficiency.
However, these same signs are characteristic of many other diseases, so it is important to conduct additional research (microflora culture), which will be discussed below.
Possible symptoms also include:
- heartburn (in some cases with impaired swallowing function);
- increased body temperature and vomiting (mainly in the evening and at night). Vomit will contain small whitish films;
- pain in the upper abdomen;
- diarrhea, in which the stool contains light mucus mixed with blood;
- the formation of white spots on the roof of the mouth, gums and tongue if the infection begins to progress and spread from the esophagus into the oral cavity.
If treatment is not started on time, the walls of the esophagus will become covered with small ulcers or, even worse, the tissue will begin to die (necrosis, in many cases irreversible). There is also a high risk that a secondary infection will occur, and this will only worsen the course of the disease and require additional diagnostics and, accordingly, a more intensive course of treatment.
If the doctor suspects that the patient is suffering from esophageal candidiasis, he will first order an endoscopic examination and also perform a microflora culture. This will help identify the degree of the disease, of which there are three:
- catarrhal esophagitis;
- fibrinous esophagitis;
- fibrinous-erosive esophagitis.
Characteristic symptoms
The severity of symptoms is almost unrelated to the severity of the disease - obvious signs may appear at the very beginning of the process or after the fungus grows so much that it physically interferes with the esophagus from functioning normally.
In 25–30% of patients, the disease occurs without any symptoms and until a certain point (until the fungus takes over most of the organ) does not in any way affect the patient’s well-being.
When the infection spreads on a large scale, the patient has difficulty swallowing food. The process becomes painful, at the same time an aversion to food develops, nausea and uncontrollable vomiting of cheesy contents and candidal films appear.
Further development of the disease is accompanied by acute poisoning by fungal toxins, fever (sudden jumps in temperature to 39–40°C), stool disorders (diarrhea with blood and mucus), and sudden weight loss caused by aversion to food. The patient moves little due to physical exhaustion and general intoxication.
Toxins released by Candida. Click on photo to enlarge
Candidiasis of the esophagus is accompanied by more or less pronounced manifestations of diseases of the gastrointestinal tract:
- gastritis;
- duodenitis;
- enterocolitis;
- dyspepsia with indigestion, bloating, belching, heartburn, nausea, diarrhea with blood and mucus.
Against this background, there are some symptoms characteristic of fungal infection of the esophagus:
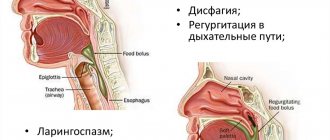
- Difficulty, painful swallowing.
- Decreased appetite to the point of complete absence.
- Weight loss, physical exhaustion, dehydration.
- Indomitable vomiting with the release of numerous whitish films or curdled contents of the esophagus.
- Pain and heaviness in the chest not associated with swallowing.
- Organ obstruction.
Fungal disease of the esophagus is complicated by:
- the addition of a secondary bacterial infection and the development of acute purulent inflammation (phlegmon);
- vascular bleeding;
- breakthroughs (perforations) of the organ wall;
- candidal sepsis (large-scale inflammation in response to a widespread fungal infection) and eventual death.
Severity
How esophageal candidiasis will proceed depends on the spread of infection throughout the mucous membrane, the area of the affected surface, and the penetration of Candida deep into the epidermis and other tissues. The combination of these factors determines the severity of the disease.
| 1st degree | The fungus invades the surface epithelial cells, forming sparse whitish cobwebs, spots and islands scattered throughout the esophageal mucosa |
| 2nd degree | Pathogenic forms of Candida (elongated cells, pseudomycelium) grow deep into the mucous membrane, one after another capturing its layers. Extensive, overgrown films and a coating of fungus appear on the inner surface |
| 3rd degree | The fungus invades vessels and tissues located outside the esophagus The process is accompanied by the appearance of necrotic ulcers (areas of dead tissue), complicated by the addition of a bacterial infection (phlegmon), bleeding from blood vessels and ruptures of the damaged mucosa In the lumen of the organ, in addition to the fused plaque and islands of fungus protruding above the surface, numerous films (pseudomembranes) are formed, blocking the lumen of the esophagus and making swallowing difficult. |
Complications
In the human body, fungi first adhere to the walls of the esophagus, penetrate epithelial tissue, and enter the bloodstream through capillaries. The infection travels through the blood through the body, capturing new structures in the human body.
At the first stage, the infection captures only the superficial layer of mucous membranes. Esophageal candidiasis of the 2nd degree is characterized by the introduction of fungal microorganisms into the internal layers of the walls of the organ. With an advanced disease, the fungal fringe can grow so that the lumen of the esophagus becomes blocked.
Advanced candidiasis of the esophagus can cause the following complications:
- bleeding from the mouth;
- intestinal obstruction;
- perforation of the esophageal walls;
- gastritis;
- stomach ulcer;
- sepsis;
- necrosis of esophageal tissue.
The above complications pose a danger to human life. Disastrous consequences can be avoided by starting therapy in a timely manner.
What is the danger?
Mycosis of the esophagus is a dangerous, difficult to diagnose disease. Fungal infection of the gastrointestinal tract in patients often causes severe complications.
What are the complications of esophageal thrush:
- Stricture. To diagnose this complication, X-rays with contrast are used. Scar changes narrow the lumen of the organ and lead to nutritional dystrophy (exhaustion). The complication occurs in 8-10% of patients.
- Bleeding. Develops due to contact bleeding of the thinned esophageal mucosa. Chronic blood loss leads to anemia.
- Perforation of the esophagus. Characterized by intense pain and subcutaneous emphysema (accumulation of air).
- Spread of candidiasis to other organs of the gastrointestinal tract.
- Sepsis. The candida form of blood infection is difficult to treat.
The condition of the esophageal mucosa with candidiasis worsens every day. It becomes thinner, and the vessels gape on its surface.
Nutrition for mycosis of the esophagus
For diseases of the gastrointestinal tract, the diet should be gentle in order to irritate the inflamed areas of the digestive tract as little as possible.
Excludes:
- rough and solid food;
- hot, cold;
- sour, spicy, salty;
- alcohol, carbonated drinks, whole milk;
- fatty, fried.
The diet should consist of vegetables, unsweetened fruits - a source of fiber, protein products, cereals, and vegetable oils. Sugar and flour contain simple carbohydrates, which serve as food for fungi, so consumption is limited to a minimum.
Important. Taking bifidobacteria in the form of drugs or as part of fermented milk products will help normalize the microflora in the esophagus.
Food is prepared by boiling, stewing or steaming, and grinding to puree. Take food in small portions. The deficiency of essential microelements is compensated with vitamin complexes.
Diagnostics
Diagnosis of candidiasis is carried out using esophagoscopy, a method using a special optical device. It allows you to assess how damaged the esophageal mucosa is.
Characteristic signs of candidiasis during esophagoscopy:
- On the mucous membrane there is a whitish or yellowish coating in the form of cobwebs, loose round or oval plaques, grayish fringed ribbons.
- The inner surface is swollen, red, easily injured and bleeds.
- Under the plaque, ulcers and erosions of various sizes are found.
To determine the location, type of esophageal fungus and its sensitivity to medications:
- A mucosal scraping (biopsy) taken from the esophagus is stained using a special cytological brush (it is inserted through the mouth or nasal opening). If the result is positive, the smear reveals round or oval Candida cells and filamentous pseudomycelium.
- Biological material (a piece of tissue, a biopsy) is stained using special dyes (CHIK reaction to mucopolysaccharides), determining how deeply the fungus has penetrated into the esophageal mucosa.
- The material (scraping from the walls) is inoculated into a nutrient medium, determining the degree of sensitivity (treatable) or resistance (not treatable) of the fungus to various medications.
The degree of damage to the esophagus due to candidiasis
It is customary to divide the degree of damage to the walls of the esophagus into three groups:
- The plaques are white, single, scattered. The superficial mucous layer is affected.
- The plaques are film-like, sometimes extensive in area in the form of rounded plaques with a diameter of 1 to 5 mm. The submucosal layer is affected.
- The overlays are represented by a fibrin mesh with the inclusion of effusion cells and necrotic mucosa. Pseudomycelium penetrated deeply into the muscle layer.
Let us recall that similar endoscopic changes can be observed with reflux esophagitis, Barrett's esophagus, herpes esophagitis, flat leukoplakia, lichen planus, burn or tumor of the esophagus. Therefore, diagnosis of esophageal candidiasis is based on endoscopic examination and laboratory examination of biopsy materials from the affected areas. It must be taken into account that with a single biopsy, the sensitivity of laboratory methods is insufficient.
How to treat esophageal candidiasis
Esophageal candidiasis is treated with antifungal (antimycotic) agents and immunostimulants. Antimycotic substances are prescribed based on the results of laboratory tests and identified resistant and non-resistant types of sensitivity to various drugs.
Immunostimulating substances are prescribed only after violations in the functioning of the immune system have been identified, since different types of these drugs have different degrees of impact on the functional components of human immunity.
When determining esophageal candidiasis in a person, it is necessary to identify and treat candidiasis in other organs of the digestive system. Without such therapy, it will be almost impossible to treat candidiasis in the esophagus, since there will be constant infection from other organs.
The arsenal of antifungal agents is quite extensive. To treat candidal lesions of the esophagus, oral therapy is initially carried out; intravenous administration of drugs is used in refractory cases of the disease.
Medicines
Before treating candidiasis, the patient must undergo a comprehensive examination. Using diagnostics, you can confirm or refute the diagnosis. Depending on the results of the examination, a treatment regimen is prescribed. As a rule, it includes the following drugs:
- Anaferon. The immunomodulator is used in the complex treatment of viral bronchitis, acute respiratory infections, pneumonia, ARVI, herpes, and various immunodeficiency conditions. The big advantages of the medicine are its homeopathic origin and strong antiviral effect. According to reviews, no disadvantages of Anaferon have been identified.
- Enterosgel. Enterosorbent has the form of a paste that has no taste or smell. The drug helps cleanse the body of allergens, pathogenic bacteria, waste and toxins. The advantage of the drug lies in the minimal list of side effects, which occur exclusively in isolated cases. The disadvantage of Enterosgel is its high cost.
- Immunal. This product has antiviral, anti-inflammatory, and immunostimulating effects. The key component of the drug is Echinacea. Immunal is used to strengthen the immune system for various diseases, including candidiasis. The advantage of the drug is its versatility in the treatment of various pathologies; in addition, it can even treat small children. The disadvantage of the medicine is that it is relatively expensive and is prohibited for use by people with AIDS and autoimmune diseases.
Antifungal drugs
Patients with moderate severity of fungal infection of the esophagus and minor disorders of the immune system are shown a short course of therapeutic drugs. As a rule, antifungal treatment is carried out in this case using an absorbable group of drugs in the form of an oral azole. Treating esophageal candidiasis usually begins with one of the following medications:
- Ketoconazole. It begins to act after the first dose and gives an excellent effect in the treatment of damage to the esophagus. The active substance is well absorbed from the gastrointestinal tract in the presence of an optimal acidic environment. The disadvantage of the drug is its ineffectiveness in acid-base imbalance. The advantage of Ketoconazole is its rapid action.
- Clotrimazole. This drug is a broad-spectrum antifungal agent and is available in the form of anal, vaginal suppositories, solution, etc. The drug disrupts the vital activity of pathogenic fungi that provoke an inflammatory process in the esophagus. The disadvantage of the drug is that it is prohibited for use in children under 12 years of age, as well as in the presence of digestive disorders. The big advantages of Clotrimazole are its effectiveness and speed of action.
- Fluconazole. It is a water-soluble form of Triazole. Like Ketoconazole, Fluconazole will be effective only if the acidity of the gastric juice is normal. The drug is most effective for the treatment of candidiasis of the esophagus than other organs of the gastrointestinal tract. The disadvantage of Fluconazole is that it has many side effects. The advantage of the medication is its speed of action and lasting effect.
Diagnosis of mycosis of the esophagus
A gastroenterologist is involved in the diagnosis and treatment of the initial stages of gastrointestinal diseases. Manifestations of fungus in the esophagus are not specific, so instrumental studies are carried out:
- X-ray with contrast. Determine uneven contours, narrowing of the esophagus, convergence or convergence of folds of the inner layer, erosion, ulcers, and impaired motility.
- Esophagoscopy. It is used as both a diagnostic and treatment method. An optical device is inserted into the cavity of the esophagus and the surface of the mucous membrane is examined. At the same time, material is collected to determine the type of pathogen.
- The resulting biomaterial is examined using cytological methods, inoculation in a culture medium and microscopy. Determine the resistance of the microorganism to drugs.
- Endoscopic ultrasonography. An ultrasound sensor is inserted into the esophageal canal and its deep layers are examined.
- Virtual endoscopy, magnetic resonance imaging. The advantages of the methods are non-invasiveness and high information content, the disadvantage is the inability to take biosamples for analysis.
To differentiate mycosis from other lesions of the esophagus - burns, reflux esophagitis, tumors, varicose veins, ulcers, lichen planus, flat leukoplakia - a biopsy is performed several times.
Mycosis of the esophagus rarely occurs as an independent disease, so the doctor prescribes a comprehensive examination of the patient:
- general blood test and glycohemoglobin test to determine sugar levels;
- HIV test;
- X-rays of light;
- colonoscopy;
- Ultrasound of organs.
Having clarified the diagnosis, the doctor prescribes the optimal treatment regimen.
Nutrition and diet
Nutrition for a fungal infection can stop the proliferation of spores or, conversely, accelerate it. He needs to pay special attention and find out what you can eat with candidiasis and what you can’t. The diet speeds up the treatment process and is also a preventative measure to prevent relapses.
Nutrition for esophageal candidiasis has two basic rules. The first is to eat only liquid, soft and pureed foods. It is necessary to exclude any solid foods that can scratch an already diseased organ. It is necessary to prepare liquid porridges from rice, semolina or oatmeal, and grind soups with a blender. Secondly, avoid prohibited foods. Any dishes that negatively affect therapy should be eliminated from the diet. The list of prohibited foods includes:
- yeast products, including bread;
- fatty, spicy, salty and sour foods;
- mushrooms of any kind;
- smoked sausages and other similar products;
- seasonings and mustard;
- sweet soda, alcoholic drinks;
- chocolate, sugar;
- citrus;
- sour berries;
- strong tea and coffee.
Do not be alarmed - these products should be excluded only during an exacerbation. When the disease begins to recede, you can eat your usual food in small quantities and monitor the body’s reaction. The duration of the therapeutic diet is from 1 month. At first, such a diet may cause apathy, weakness, and decreased concentration. This is due to a lack of carbohydrates, but this condition goes away within 7-10 days.
Treatment
When you first suspect esophageal candidiasis, you should contact a gastroenterologist to receive qualified help.
Medication
The sooner the diagnosis is made, the sooner you can begin drug therapy, which is based on taking immunostimulants and antifungal drugs. If you start therapy in the early stages of the disease, you can prevent the profuse growth of spores in the gastrointestinal tract, followed by generalized candidiasis.
To achieve a speedy recovery, drugs aimed at combating fungi (antimycotic agents) are prescribed. The peculiarity of such medications is that they are poorly absorbed through the walls of the gastrointestinal tract, exerting a local effect on pathogenic growths.
For medicinal effects, the following drugs can be prescribed:
- Fluconazole;
- Levorin;
- Nystatin;
- Pimafucin.
Photo gallery: drugs prescribed for esophageal candidiasis
Levorin
Nystatin
Fluconazole
The dosage of all the above-mentioned drugs is determined by the attending physician - it depends on the degree of prevalence of the fungus in the esophagus, the characteristics of the patient’s body and his susceptibility to specific medications.
Along with antifungal agents, eubiotics can be prescribed, which are aimed at restoring the microflora of the gastrointestinal tract after suffering from an illness. Their use begins after the end of therapy and continues for several weeks. Among the eubiotic drugs, the following should be highlighted:
- Linux;
- Baktisubtil.
Features of dietary nutrition
Diet for such a disease is a mandatory measure, which is part of the treatment process and speeds up recovery. In this case, it is necessary to strictly separate food products that have a negative effect under these conditions from those that contribute to the restoration of the body.
It is necessary to understand that Candida fungi multiply abundantly in case of violation of nutritional rules. The following should be excluded from the patient’s diet: yeast, vinegar, sugar and dishes containing these components, dairy and fermented milk products.
All foods rich in carbohydrates are prohibited:
- bread and other baked goods;
- alcoholic drinks;
- chocolate;
- raw mushrooms;
- honey;
- dried fruits;
- potato.
Prohibited products in the photo
Potato
Honey
Mushrooms
Chocolate
Alcohol
Bread
It is unacceptable to eat sweet fruits and citrus fruits - these foods contribute to the development of fungi. During treatment, all of the above should be completely excluded from the diet, and some time after recovery, foods can be introduced into the diet gradually and in small quantities.
The functioning of the digestive system should be stimulated by the development of healthy, “friendly” bacteria in the body, which are contained in products consisting of coarse fiber.
Since the process of drug treatment is carried out with the help of antifungal agents, the content of vitamin K in the patient’s body decreases, which can lead to bleeding. It is possible to obtain the necessary component from cereals with low gluten content, these include:
- millet;
- buckwheat;
- brown rice.
A lot of the essential vitamin is present in greens, strawberries, alfalfa and other plants. It is also necessary to consume various immune-stimulating substances, for example, kombucha tea, which should be included in the diet.
Often, patients with esophageal candidiasis experience significant discomfort and weakness during the period of treatment and dietary nutrition, despite the fact that there are virtually no restrictions on the consumption of meat and other protein foods. After some time, the body will begin to get used to the established restrictions, and the condition will improve.
Traditional methods
It should be understood that traditional medicine cannot be the only therapeutic tool for esophageal candidiasis. Such drugs are often used for symptomatic treatment, stimulation of the body and strengthening the immune system. As part of auxiliary treatment, it is possible to use various decoctions and infusions that will have a beneficial effect on the course of recovery.
Among the most popular and effective folk recipes, the following should be noted:
- in the presence of severe painful sensations, decoctions of chamomile, oak bark or calendula will be indispensable. It is very simple to prepare them: a tablespoon of dry raw materials is poured into a glass of clean water and boiled in a water bath for about a quarter of an hour. After cooling, the composition is filtered. Such remedies also help cope with inflammatory processes;
- Kombucha tincture. The product is prepared as follows: the mushroom is placed in a jar and filled with sweet tea (10 g of tea leaves and up to 100 g of granulated sugar are needed per liter of water), after which it is left in a dark place for a week. The finished infusion is taken in a glass daily, dividing this volume into 4 doses.
Folk remedies in the photo
Oak bark
Calendula decoction
Chamomile decoction
Kombucha tincture
Folk remedies
Traditional treatment of esophageal candidiasis with folk remedies complements antifungal therapy:
- For combined damage to the esophagus and oral cavity, traditional healers recommend a solution of baking soda. 1 spoon of soda is diluted with a glass of water. Irrigate your mouth 2-3 times a day after meals.
- Propolis tincture gives a good result for esophageal candidiasis. Take 3 teaspoons 3-4 times a day.
- Pharmaceutical chamomile gives a good anti-inflammatory effect. Water infusions are used. 2 tablespoons of plant material are poured into 1 liter of boiling water and left for 2-3 hours. Drink 1/3 glass 3 times a day throughout the entire treatment.
- An alcohol solution of chlorophyllipt is also taken internally. A teaspoon of tincture is diluted in 1/3 glass of water. Drink half an hour before meals 3 times a day.
- Affected tonsils are lubricated with lavender oil. The plant's esters have an enveloping and wound-healing effect.
Symptoms of candidiasis
Among gastroenterological diseases, esophageal candidiasis is the most difficult to diagnose. After all, the degree of damage to the walls of the esophagus and what the patient feels do not correspond to each other.
A third of the sick are not bothered by any symptoms; when the pathology develops, people are not aware of their illness. There are signs by which the disease can be identified. The following symptoms indicate esophageal candidiasis:
- Heartburn.
- Lack of appetite.
- Dysphagia is an abnormal process of swallowing food.
- Odynophagia is pain when swallowing.
- Frequent manifestations of nausea and vomiting.
- Pain in the stomach and chest.
- Loose stools.
- Unreasonable increase in temperature.
I would like to draw attention to the symptoms of vomiting and pain when swallowing, which may appear slightly, or may be so pronounced that it will become impossible to eat and drink water. And with nausea and vomiting, specific whitish films are present in the vomit.
There are bloody spots in loose stools. With loss of appetite, body weight decreases. With esophageal candidiasis, a characteristic concomitant disease is oral thrush.
This disease begins with penetration into the mucous cavity, then goes deep into the tissue. The resulting films can close the lumen of the esophagus, and ulcers and necrotic areas appear in the esophagus itself and on its walls. This means adding a bacterial infection. Esophageal candidiasis has complications, but they manifest themselves to a lesser extent compared to intestinal candidiasis, such as the development of ulcers, bleeding and tissue necrosis.
The disease manifests itself as yellow or white foci on the affected walls of the esophagus. These zones are raised and after some time are able to merge. Fungal colonies get inside the joints, penetrating into blood vessels and muscle tissue.
Composition of plaque ⏤ epithelial cells mixed with fungi, bacteria and inflamed cells. When analyzing microscopy, characteristic threads with fungal mycelia are found. The yeast-like structure and uniform color of the research object are characteristic. According to the severity of esophageal candidiasis, they are divided into three groups:
First. There are whitish plaques with pseudomycelium of the fungus between the epithelial cells.
Second. The plaques form a film and vast fields, merging together. In this case, the pseudomycelium of the fungus penetrates deeper into the layer of submucosal tissue.
Third. Pseudomembrane type of deposits, and the fungus penetrates into the muscle tissue.
Prevention
In order to reduce the risk of disease, it is necessary:
- Maintain personal hygiene and brush your teeth regularly;
- Limit consumption of sweets;
- Get regular dental check-ups;
- When using antibiotics, take antifungal drugs and eubiotics (dietary supplements).
- General strengthening measures to improve immunity.
Treatment of esophageal candidiasis requires patient responsibility, since consequences and complications threaten worsening of the condition and relapses. Instrumental studies and accurate diagnostics help confirm the success of therapy.
Causes of candidiasis
Research conducted in the medical field shows statistics: in a quarter of people, the candida fungus is in the mouth, and in eight out of ten it is in the intestines.
There are a number of factors and conditions that trigger the fungus to develop and multiply, creating colonies that attack organs.
The infection enters the body from the environment. For example, this happens when:
- eating contaminated foods;
- using household items that have been contaminated;
- direct contact with the patient.
Antifungal Diet
One of the most important parts of therapy is nutrition. Unfortunately, without following certain rules, it is impossible to completely get rid of the disease and recover. The daily diet should be nutritious and balanced. It should be free of heavy carbohydrates, which complicate digestion and take a long time to digest. The patient needs to stop smoking and drinking alcohol, as they will only worsen their health. When following a diet, you must include foods such as:
- oatmeal;
- pickled vegetables;
- kefir with low fat content;
- natural yoghurts.
If it is impossible to swallow on your own, all food is finely ground to a puree consistency before consumption. All dishes are steamed or simply boiled. There should be no fatty, spicy foods in the diet, and any spices should be excluded. The temperature of the food consumed should not be very hot or cold. This will help reduce irritation of the mucous membrane. Regular jelly or oatmeal broth can also help improve digestion. The patient must ensure that the daily diet contains all the vitamins and microelements necessary for normal functioning. Try to eat foods that do not irritate the intestines and esophagus, be sure to include fruits and vegetables. They contain vitamins and minerals of various groups.
For nutrition, you need to select vomits that do not irritate the esophagus
Fungal infections of the gastrointestinal tract
Today, humanity is experiencing an epidemic of opportunistic infections, among which mycoses occupy one of the leading places. According to WHO, in the last decade, about 20% of the world's population suffers from mycoses [1]. Mycoses are infectious diseases whose etiological pathogen is fungi. Most often, people with primary or secondary immunodeficiency conditions suffer from mycosis [2]. Mycosis is an opportunistic infection [3, 4]. Mushrooms are lower plants (more than 100 thousand species), lacking chlorophyll, so their existence requires ready-made organic substances. The vast majority of fungi are saprophytes, a minority of them are parasites of humans and animals. About 500 species of fungi can cause infectious diseases in humans. The yeast-like C. albicans is most often found in humans [5]. Candidiasis is an anthroponotic mycosis characterized by damage to the mucous membranes and skin. Lesions in humans are caused by C. albicans (more than 90% of lesions), C. tropicalis, C. krusei, C. lusitaniae, C. parapsilosis, C. kefyr, C. guilliermondii, etc. [6–8]. At the beginning of the 20th century. candidiasis was observed relatively rarely. Since the beginning of the use of antibiotics and to the present day, the incidence of candidiasis has increased significantly and continues to grow. An unfavorable environmental situation, which has a negative effect on the immune system of the human body, is of no small importance in the development of candidiasis [9]. Candidiasis usually occurs endogenously as a result of dysfunction of the immune system and dysmetabolic disorders in the body. In recent years, candida are the most common causative agents of opportunistic mycoses [4]. When the body is affected by candida, severe visceral forms may develop, often involving the lungs and digestive organs and other body systems. Candidiasis can be systemic in nature and become disseminated (massive growth of the pathogen in the body) and take on the picture of fungal sepsis with damage to all organs (kidneys, heart, spleen, brain), and sometimes with the development of septic shock [10]. More often, this form of candidiasis affects patients with the last stage of cancer and AIDS [11, 12]. Etiology and pathogenesis
The most common causative agent of mycoses, C. albicans, is a normal commensal of the oral cavity, gastrointestinal tract, vagina, and sometimes skin. C. albicans are opportunistic microorganisms with a high level of carriage and a pronounced tendency to increase it: if in the 1920s. carriage on the oral mucosa was 10%, then in the 1960–1970s. increased to 46–52% [13]. Many studies have shown that any violations of the body’s resistance or changes in the normal intestinal microbial cenosis can lead to the development of the disease – candidiasis [14]. The skin and mucous membranes are “open systems” of the macroorganism, constantly in contact with the environment. In turn, Candida spp. widely distributed in nature, they often contaminate soil, water, food, and household surfaces. Frequent human contact with Candida spp. explains the significant prevalence of transient candidiasis in the human population. According to statistics, among the population of European countries, candida is detected in the feces of 65–80%. As an opportunistic representative of the human microflora, fungi do not pose a serious threat to the health of an immunocompetent person [15]. At the same time, against the background of an increase in the number of patients with disorders in antimicrobial resistance systems, a significant increase in the incidence of candidiasis is observed [16]. Many researchers associate the increase in candidiasis with risk factors, which include childhood and old age, therapy with glucocorticosteroids and antibacterial drugs, intensive cytostatic polychemotherapy, diabetes mellitus and other diseases of the endocrine system, AIDS, severe debilitating diseases, impaired trophological status, genetically determined immunodeficiencies [17 -19]. Primary infection of the human body by Candida occurs when passing through the mother's birth canal, as evidenced by the high frequency of Candida isolation in newborns (up to 58%) and the almost complete coincidence of the species composition of Candida in the child and mother. Infection is facilitated by the increased frequency of carriage and vaginal candidiasis in the last third of pregnancy. There is information about the transmission of Candida fungi during breastfeeding [20]. Fungi that parasitize human skin feed on particles of the epidermis, the horny masses of the nail plates, and the products of their life - proteins - cause an allergic reaction. The pathogenicity factor of fungi of the genus Candida is their ability for adhesion and invasion, followed by tissue cytolysis, and then lymphohematogenous dissemination [21]. Candida spp. capable of an invasive process in the mucous membranes, primarily represented by stratified squamous epithelium, less often - single-layer cylindrical. Most often, the invasive mycotic process is observed in the oral cavity, esophagus, stomach and intestines. It has been proven that even without penetration deep into the epithelium, Candida spp. [22] can cause pathology – a non-invasive form of candidiasis. Contact of surface and corpuscular antigens of the fungus with immunocompetent cells of the macroorganism can lead to the production of increased amounts of specific IgE and sensitized lymphocytes, which serves as the pathogenetic basis for mycogenic sensitization. Allergens in Candida albicans are also the primary metabolites - alcohol dehydrogenase and acidic P2 protein. This is potentially dangerous in terms of the development of mycogenic allergic diseases: specific bronchial asthma, atopic dermatitis, urticaria. Resorption in the intestine of metabolic products of fungi of the genus Candida - its plasmacoagulase, proteases, lipophosphorylases, hemolysin and endotoxins can cause specific intoxication and secondary immunodeficiency [23]. Due to interaction with representatives of obligate normobiota and opportunistic microorganisms Candida spp. can induce dysbiosis and mixed infection of mucous membranes. The key factor in the onset of the infectious candidiasis process is the violation of nonspecific and specific resistance of the body both at the local and general levels [23]. Factors of nonspecific resistance traditionally include an adequate balance of desquamation and regeneration of epithelial cells, mucopolysaccharides of mucus, normal microbiota of the mucous membranes (Bifidobacterium spp., Lactobacillus spp., Escherichia coli, Peptostreptococcus spp.), peristaltic activity and the acid-enzyme barrier of the digestive tract. It has been shown, for example, that treatment of patients with drugs containing bifidobacteria significantly reduces the content of Candida fungi in the feces of patients [24]. Nonspecific factors also include secretory IgA, lysozyme, transferrin, and complement components. However, the number and function of polymorphonuclear mononuclear phagocytes are most important, in particular their ability to chemotaxis, attract, kill, and present fungal antigen. It is under conditions of neutropenia that life-threatening forms of candidiasis develop, including visceral lesions (liver, gallbladder, pancreas) [11]. The specific immune response to candidiasis is represented by the production of specific anti-candidiasis antibodies of the classes IgA, IgG, IgM, which inactivate invasion enzymes and endotoxins of the fungus, as well as together with complement components involved in opsonization [25, 26]. The conflict between the pathogenicity factors of the fungus and the factors of antifungal resistance leads to the development of one or another form of candidiasis. The mechanisms of pathogenesis of 2 fundamentally different forms of candidiasis (invasive and non-invasive) formed the basis for the classification of intestinal candidiasis.
Clinical forms
For practical purposes, it is necessary to distinguish 3 forms of damage: – invasive diffuse;
– focal (secondary to duodenal ulcer, nonspecific ulcerative colitis); – non-invasive (so-called candidiasis dysbiosis) [27]. Quite often, candidiasis of the digestive system occurs in the form of a mixed infection: Candida-bacterial, Candida-herpetic, Candida-protozoal, which makes the clinical picture of the disease quite variable. The frequency of mixed infection in intestinal dysbiosis with increased proliferation of fungi of the genus Candida, according to some data, is 63%. Moreover, an association with a significant number of bacteria with the so-called proteolytic main metabolic pathway (opportunistic pathogens) is more often found: Escherichia coli, Ristella, Clostridium perfringens, Klebsiella, Morganella, Bacteroides, Staphylococcus aureus, Pseudomonas aeruginosa [28]. Among all localizations of candidiasis of the digestive tract, oropharyngeal localization
ranks first [29].
Candidal stomatitis in newborns is a common disease. In the first days after birth, the baby’s mucous membranes are resistant to fungi. Subsequently, insufficient secretion of IgA and a gradual decrease in antimicrobial immunity transmitted from the mother lead to high morbidity [30, 31]. Oral (oropharyngeal) candidiasis is a widespread mycosis in people suffering from various forms of immunodeficiency, primarily AIDS and hematological malignancies, and the gastrointestinal localization of candidiasis in patients with AIDS can be a source of candidemia, which in such patients with other localizations of candidiasis occurs in only 1% of cases [ 32, 33]. A common mycosis of the digestive tract is esophageal candidiasis,
which is recorded both in immunocompetent and (much more often) in immunocompromised individuals [34].
Candidal esophagitis in general hospitals occurs in 1.3-2.8% of patients, in transplant departments - in 4%, with disseminated carcinomatosis - in 2.8-6.7%. This disease often occurs without subjective complaints and is detected by chance during “continuous” studies of the population in 1–7% of cases. Sometimes patients note pain and discomfort when passing solid and liquid food, dysphagia, and hypersalivation. According to the depth of the lesion, 4 types are endoscopically distinguished - from mild edema, hyperemia, single white plaques < 1 mm in diameter to massive inflammation, deformation and bleeding of the mucosa, ulceration, even perforation. A comparative assessment of various methods for diagnosing esophageal candidiasis showed that in 95% of cases, candidiasis was detected by analyzing scrapings and only in 39% by analyzing biopsy material [35]. Gastric mycoses,
including candidiasis, are rarely noted in the absence of any other pathology of somatic or bacterial etiology [36–38].
Their share among all cases of candidiasis of the upper digestive tract is only 5.2%. Much more often (up to 17–30%) Candida spp. found in biopsy samples of gastroduodenal ulcers, as well as in chronic gastritis [39]. However, only the findings of pseudomycelial structures of the fungus, and not individual non-budding cells, during a morphological study of cytological and/or histological preparations stained according to the Romanovsky-Giemsa method or the PAS method, reliably confirm the diagnosis of gastric candidiasis. In recent years, Candida spp. often isolated in association with Helicobacter pylori, and standard anti-Helicobacter therapy increases the incidence of gastric candidiasis [40]. The vast majority of Candida spp. isolated from patients (65.6%) had high or moderate virulence. When isolated from the gastric juice of patients with gastroduodenal diseases, the association of Candida spp. and Helicobacter pylori, a more severe course of the disease can be assumed, and the planned antibacterial therapy must be carried out in conjunction with antifungal therapy [39]. Intestinal candidiasis
as an isolated form of the disease is rare.
Usually it is a continuation of candidiasis of the stomach and upper digestive tract. Intestinal candidiasis is often accompanied by diarrhea. There are diarrhea of various etiologies [40] with concomitant release of Candida and candidal diarrhea (CD), in which Candida is the only excreted pathogen. The main predisposing risk factor for KD, especially in hospitalized patients, is antibiotic therapy. Other risk factors: endocrine disorders, immune dysfunctions, neoplasms, steroid therapy; The elderly age of patients also plays a role [41]. In patients with CD, C. albicans is most often isolated, followed by C. krusei, C. tropicalis, C. kefyr, C. stellatoidea, C. guilliermondii, C. parapsilosis, C. lusitaniae [41]. In cases where Candida is a component of the normal intestinal biota, its growth and reproduction are suppressed by intestinal microorganisms, where the fungus is present in stable quantities and does not multiply [35]. When the bacteriobiota is suppressed by antibiotics, yeast multiply with the formation of growth tubes and the appearance of mycelial structures. According to T.V. Tolkacheva et al. [13], the frequency of isolation of yeast fungi from the intestines of immunocompromised patients remains high, reaching 63–65% in the last 2 years. The ratio of detection rates of C. albicans and non-albicans strains is 52.5%. Among the latter, C. krusei (40%), C. glabrata (28%) and C. kefyr (15.6%) dominate [42]. An increase in the frequency of occurrence of an association of 2 species of Candida non-albicans and an expansion of the species spectrum of yeast fungi colonizing the intestines of patients with hemoblastosis were noted. Candidiasis of the large intestine is a rare disease; it is more often recorded in association with other intestinal pathogens of a bacterial nature [43]. In recent years, it has been hypothesized that chronic intestinal candidiasis may be an etiological factor in the formation of chronic fatigue syndrome [44]. Signs of mycogenic sensitization are detected in 10.4% of patients with intestinal dysbiosis with excessive growth of Candida fungi. The diagnosis is established in the presence of the following criteria, such as: flatulence, abdominal discomfort, changes in stool consistency and frequency, signs of moderate intoxication and a tendency to exacerbation of allergic diseases. Fungal infection of the biliary system
is facilitated by previous biliary dyskinesia, dyspancreatism, giardiasis, cholestasis, hypotension of the gallbladder and other lesions.
Under these conditions, favorable conditions are created for the proliferation of fungi and other microorganisms. The cause of candidiasis cholecystitis can be stones in the bile ducts, which are often a “reservoir” for fungi; some authors even call them “fungal bodies” or “candidiasis stones”. Mycoses of the biliary tract are more common than is commonly believed. Diagnosis
Diagnosis of candidiasis using purely clinical methods is impossible due to the fact that its clinical manifestations do not have absolute specificity. In the vast majority of cases, modern clinical and laboratory instruments allow for high-quality examination and help the clinician make a diagnosis, as well as prescribe effective treatment for infections caused by fungi. In recent years, endoscopic technologies have expanded the possibilities for diagnosing fungal esophagitis and gastritis. During esophagogastroduodenoscopy, attention is paid to hyperemia and ulceration of the mucous membrane, the presence of white deposits and films, narrowing of the lumen of the esophagus, and accumulation of mucus [45]. During this procedure, it is imperative to take material for microbiological examination, since the etiology of these manifestations is not always fungal. Moreover, the information content of plaque research is higher than that of biopsy specimens (95% compared to 39%). Video information endoscopic studies with digital recording and image analysis are especially promising. A clear distinction between unchanged and pathological tissues and analysis of histochemical processes in the mucous membrane of the digestive tract are possible using endoscopic spectroscopy and fluorescence endoscopy [46]. Video and colonoscopy, chromoendoscopy against the background of “medicinal” sleep using Diantek technology are distinguished by high quality research, painless manipulations and the absence of stress and fear in patients [8]. It should, however, be emphasized that invasive manipulations with inflamed gastrointestinal mucosa are unsafe, can promote fungal and bacterial dissemination, and sometimes lead to injury and perforation of the wall of the esophagus or stomach. Endoscopic ultrasonography with Doppler mapping and contrast enhancement of tissue and vascular structures is promising; it allows detailed differentiation of all layers of the wall of the digestive tract. Non-invasive methods - virtual endoscopy, which allows obtaining a 3-dimensional image, magnetic resonance imaging - have a great future [47]. Studying gastroduodenal motility using scintigraphy and electrogastrography is also important for diagnosis and prescribing additional medications, since impaired motor function of the stomach and “stagnation” in the gastrointestinal tract create conditions for the proliferation of fungi and bacteria. Colonoscopy makes it possible to assess the condition of the intestinal mucosa, the presence of white plaque, ulcerative defects, etc. In the future, methods based on new scientific and practical research will be introduced in gastroenterology: enzyme immunoassay of fecal antigens, PCR and even genetic testing [5, 47]. Laboratory confirmation of a fungal disease of the gastrointestinal tract is possible through microscopy and/or cultural examination of swabs from the mucous membranes of the oral cavity and esophagus, the contents of the stomach and intestines, pathological films, plaque, etc. Quantitative assessment of fungi in biosubstrates should be carried out in comparison with clinical symptoms, taking into account the presence background diseases, mixed infections, etc. [48]. For example, the detection of single Candida colonies on the mucous membranes is not a basis for diagnosing candidiasis in immunocompetent patients. In stool, the number of colonies (more than 105–106) acquires diagnostic significance. Culture results are interpreted differently, with a lower diagnostic threshold, in immunosuppressed individuals, neutropenic patients with AIDS, and in intensive care units [49, 50]. You should also pay attention to the ability of mushrooms to vegetate and form mycelium, since this is one of the laboratory signs that confirm the diagnosis of candidiasis. Histological (Gomori-Grokkot staining, PAS reaction) and cytological (Romanovsky-Giemsa staining) studies of biopsy specimens can detect tissue forms of fungi. Many authors consider these methods to be the most reliable. In addition, mycelium and pseudomycelium in tissues confirm the presence of an invasive form of fungal infection of the gastrointestinal tract [51]. Microbiological examination of portions of bile obtained through multifractional duodenal intubation makes it possible to differentiate fungal from bacterial or functional pathology of the duodenum, gallbladder, biliary tract and liver.
Conclusion
Thus, today candidiasis is the most common type of fungal infection. People with weakened immune systems should take any manifestations of candidiasis seriously and consult a doctor at the first sign of the disease for treatment.
Causes of the disease
The main factor in its occurrence is weakened immunity. In this case, an excellent environment for the development of harmful bacteria arises, and the body is unable to independently fight the resulting infection. In addition, the fungus occurs when there is injury to the digestive system. This could be a surgical operation or the entry of chemical elements into the esophagus. Heavy, fatty and spicy foods can also cause stagnation, which leads to the proliferation of fungal infections.
In addition, there are other factors that provoke the development of esophageal pathology - these are:
- recovery period after surgery;
- tuberculosis disease;
- HIV;
- oncology;
- pathology of the kidneys, liver, endocrine system;
- chronic depression;
- emotional experiences;
- work in hazardous production;
- poor nutrition;
- bad habits;
- some medications.
Fungal spores are often found in the environment, but with a strong immune system the disease will not develop