FGS stands for fibrogastroscopy (or simply gastroscopy), perhaps the most effective method for studying the digestive organs. Let us consider in detail in this article what FGS of the stomach is, how it is done and how long the procedure lasts, what indications and contraindications it has, as well as how an adult can prepare for its safe, most comfortable implementation.
In medicine, FGS is the “gold standard” for examining people with pathologies of the digestive system. But this is unlikely to inspire “feat” in the name of their health in patients leaving the gastroenterologist’s office for the first time with a referral for FGS or FGDS. Many are lost, not knowing what to expect from this “execution” and how best to prepare for it, even if the doctor has given instructions.
After reviewing the information presented below, you will be able to expand your understanding of this procedure, get rid of prejudices that give rise to fear of the study, and prepare properly for it.
Table of contents
- FGS of the stomach - what is it, how does it differ from FGDS
- What does gastric FGS show?
- Indications and contraindications
- FGS of the stomach - how the procedure works
- How long does FGS last?
- How soon can you eat after the examination?
- How to prepare in the morning What you need to take with you for the procedure
- How to behave correctly during FGDS and FGS
- Is it possible to drink water during gastroscopy?
- Taking pills before the procedure
- Is it possible to smoke before and after FGS?
- What can you eat before FGS of the stomach?
FGS of the stomach - what is it, how does it differ from FGDS
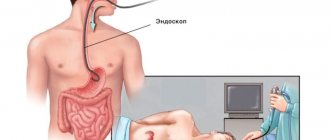
Visual examination of the mucous membrane of the stomach and esophagus using an endoscope (a flexible tube with a video camera and a light source at its end), which is inserted through the oral cavity (less often through the nose), is called gastroscopy - FGS (fibrogastroscopy).
FGS is a modern, accessible, fairly informative and popular diagnostic method for assessing the condition of the mucous membrane of the esophagus and stomach in order to make the correct diagnosis.
In many cases, to obtain the most accurate information about the state of the organs of the digestive system, the flexible endoscope probe moves further than the stomach - into the lumen of the duodenum. Then another letter appears in the abbreviation of the name of the study, replacing it with FGDS (fibrogastroduodenoscopy).
FGDS is a method that allows you to closely examine not only the condition of the esophagus and stomach (as with FGS), but also the initial part of the small intestine - the duodenum. This is the only difference between these two procedures. Preparation for the procedures is the same.
FGS or FGDS is prescribed by a gastroenterologist, and the procedure itself is performed by an endoscopist.
Important!
Today, bulky gastroduodenoscopes with thick hoses have been replaced by innovative devices that have high technical and optical characteristics, and, most importantly, a minimum thickness of the flexible tube.
These factors provide a number of benefits:
- no pain;
- easy tolerability of the procedure;
- high security;
- high information content.
If necessary, during the procedure, medical and surgical manipulations are performed, a portion of gastric juice, bile is taken, or a fragment of mucosal tissue is taken (biopsy) for laboratory testing.
Examination of the stomach if you feel unwell
Carrying out gastroscopy requires the patient to have a positive psychological attitude and satisfactory well-being. The only exceptions are critical cases when the patient requires emergency medical care.
For example, if there are signs of internal bleeding associated with exacerbation of an ulcer, erosion of the gastric mucosa and the walls of the duodenum. If the patient experiences general malaise, is bothered by severe nausea, bouts of vomiting, or dizziness due to fear and panic, the endoscopist may reschedule the examination for another day.
Unsatisfactory health caused by acute pain in the stomach is not a reason to cancel the diagnosis. In this case, the patient is indicated for an early examination of the gastrointestinal tract, since inaction is fraught with the development of serious complications.
Preparing for an FGDS of the stomach means following the approved rules in the medical leaflet. This type of examination is carried out in the morning and must be done on an empty stomach. 48 hours before the scheduled diagnosis date, a person should stop eating salty, too sour, or spicy foods.
Dishes containing an excessive amount of coarse fibers, fats of animal and vegetable origin are strictly prohibited. On the day of fibrogastroduodenoscopy, you should not brush your teeth, smoke or chew gum. Concomitant medications should be agreed upon with the endoscopist.
What does gastric FGS show?
During FGS (FGDS), even the slightest changes in the mucous membrane of the stomach, esophagus and duodenum are visible and diagnosed. A more detailed picture can only be provided by a biopsy of neoplasms (for oncology), but this is already a study at the cellular level.
FGS of the stomach in adults can show:
- condition of the mucous membrane and walls of the stomach and esophagus;
- diameter of the lumen of the esophagus (possible narrowing);
- degree of reflux (reflux of stomach contents into the esophagus);
- detect neoplasms, erosions, ulcers and bleeding.
Important!
Very often, in the early stages, dangerous diseases of the gastrointestinal tract are “silent”. Not only polyps and tumors, but also erosions and ulcers sometimes occur without symptoms. Their timely detection, as is known, is the basis for successful recovery.
Now endoscopic equipment has been so improved that anyone can be examined painlessly and comfortably for prophylaxis (without any complaints, at their own request).
Why and when is FGDS done?
An examination is prescribed for pain in the epigastric region that occurs 5-10 minutes after eating. The procedure is done to detect changes in organs, to monitor existing ulcers and cancerous tumors. The study is also carried out when:
- the occurrence of causeless nausea, vomiting;
- suspected gastrointestinal tract diseases;
- disruption of the passage of food through the esophagus;
- suspected malignant tumors;
- bloating;
- a feeling of constant heaviness in the stomach;
- some types of hernia;
- suspected polyps;
- constant or periodic but stable heartburn.
In addition to the listed cases, an examination is prescribed if, despite complaints, other studies have not yielded any results. The examination is prescribed for anemia and vomiting with blood. Gastroscopy with biopsy allows you to take samples of the juice of the digestive organs and mucous membranes for analysis. This collection helps to identify abnormalities that were not noticed with x-rays and ultrasound.
FGS of the stomach - how it is done
The FGS procedure is performed in a specialized gastroscopy room and consists of several stages.
Let's look at how gastric FGS works:
- The patient is given local anesthesia: the throat or root of the tongue is treated with a solution of Lidocaine or Dicaine (used as a spray or given to drink).
- After a feeling of numbness appears (about 5 minutes), the patient is placed on his left side.
- A mouthpiece (a plastic ring-mouthpiece) is inserted into the subject's mouth, which must be clamped with the teeth and lips.
- The doctor will carefully insert the flexible endoscope hose through the mouthpiece to the root of the tongue. Then he will ask you to swallow or inhale, and the endoscope will move into the esophagus.
- The doctor will slowly advance the device from the esophagus to the stomach and examine its walls. From this moment, the image of the mucous membrane can be seen on the monitor (if necessary, video or photo recording is carried out on a digital medium). Air is supplied through the endoscope to straighten the lumen of the esophagus and the stomach cavity. While advancing the gastroscope probe, the doctor can perform therapeutic and diagnostic manipulations.
- After the probe enters the stomach, the doctor examines the condition of its walls for several minutes.
- After completing the examination of the stomach (and other manipulations), the doctor carefully removes the device - the procedure is completed (with FGDS, the endoscope is first advanced into the duodenum). The results are recorded.
How to do gastroscopy of the stomach
The examination is carried out by a qualified specialist. Diagnosis can be performed using local anesthesia or under general anesthesia (during sleep). In any case, medication support is necessary. A gastroscopy of the stomach is performed using a fiberscope.
The device is equipped with an optical system and a light bulb, which serves to illuminate the internal surface of the organ, tools for manipulation and taking a biopsy. The device is inserted through the mouth, gradually advancing the tube to the stomach, and, if necessary, to the upper intestines.
How the research works
Patient preparation is required to perform the procedure. It differs depending on the type of anesthesia. If local anesthesia and subsequent examination of the stomach are planned, gastroscopy is performed in such a way that the patient remains conscious for the entire period. This study is done quickly - 7-10 minutes. If there are circumstances where an examination is needed over a long period of time, a drug for general anesthesia is administered intravenously to the person. For this it is important to prepare in advance.
Attention!
Gastroscopy in medicated sleep is prescribed in the morning on an empty stomach.
The general methodology includes the following steps:
- The patient is placed on his left side with his knees brought to the stomach. In this case, your back should be perpendicular to the couch.
- The pharynx is pre-irrigated with an anesthetic to reduce the occurrence of the gag reflex and involuntary cough.
- Install a mouthpiece.
- The tube is inserted into the oral cavity, gradually moving along the digestive tract.
- The specialist pumps air into the stomach for better visualization.
- The walls of the organ are examined.
- During the examination, a histological examination is performed, if necessary.
- The fiberscope is removed slowly to avoid traumatic damage to the soft tissues of the stomach, esophagus and duodenum.
During gastroscopy, a scaled image is displayed on the monitor.
Biopsy
Adult patients can undergo advanced diagnostics - perform a gastric biopsy using gastroscopy. During the procedure, tissue samples are taken with special forceps at the border of the changed and healthy areas of the mucosa. The number of samples required for histological examination is from 3 to 5.
If a tumor is suspected, chromoscopy is additionally used. The method consists of staining mucosal tissues with safe dyes in the area of suspicious areas. This allows for differential diagnosis between benign and malignant processes, as well as determining the extent of organ damage.
Helicobacter pylori
In addition to identifying pathological formations, a biopsy helps to identify Helicobacter pylori. Various studies of the obtained tissue sections are carried out.
Testing for Helicobacter pylori includes:
- microscopy;
- immunohistochemistry;
- PCR to clarify the presence of pathogen DNA;
- cultural method;
- pH-metry;
- urease test.
Additionally, swabs are taken from the surface of the stomach and the degree of contamination of the mucous membrane is determined.
How long does gastroscopy of the stomach take?
When performing FEGDS, the fiberscope is advanced to the duodenum. This allows the specialist to examine the upper digestive tract, the initial parts of the small intestine, including the nipple of Vater. Depending on the manipulations that are planned during the procedure, gastroscopy of the stomach lasts from 3 minutes to half an hour. A visual examination of internal organs without a biopsy takes 3-10 minutes. If additional studies, biopsy, and therapeutic manipulations are performed, the procedure is carried out from 15 to 30 minutes.
How to behave during the procedure
During the examination, it is important to be in the optimal position, despite physical and emotional discomfort. To do this, before the study, the patient is told how to behave and breathe correctly. It is necessary to take evenly slow inhalations and exhalations through the nose. This allows you to relax and ensures that enough oxygen reaches your lungs.
How to prepare for FGS of the stomach in the morning
In the morning before the FGS, in the first half of the day you are allowed to brush your teeth, but not eat. Only preparation for FGS of the stomach and duodenum, carried out in the afternoon, allows a light breakfast.
What should you bring with you to the procedure?
Before the gastroscopy procedure, you need to take from home:
- drinking water and medicine, which should be taken immediately after the examination;
- food, preferably kefir, yogurt (if necessary);
- towel.
In addition, you need to prepare and take with you to the FGDS:
- referral for research;
- outpatient card;
- protocols of previous studies.
How to behave during FGDS (FGS)
You should definitely notify your doctor if you are allergic to drugs for local anesthesia (for example, lidocaine).
People wearing glasses or dentures are asked to remove them.
The best advice for well-bearing and surviving FGS of the stomach is to relax as much as possible and take slow and deep breaths through your nose and mouth. Also listen to your doctor and follow his breathing recommendations.
Is it possible to drink water before FGS of the stomach?
It is not advisable to take a lot of liquid on the day of the procedure. You can drink before FGS no later than 3 hours before the test and no more than half a glass. This can be mineral water (still), weak tea. It is not recommended to drink coffee.
Taking pills before the procedure
It is allowed to take medications that do not require swallowing (dissolve in the mouth). The remaining tablets are not taken before the FGS or FGDS procedure.
Is it possible to smoke before and after FGS?
Many years of practice have proven that smoking contributes to the appearance of nausea and other unpleasant sensations during endoscopy. It can also increase the duration of the procedure due to irritation of the mucous membrane.
3 hours before the test, smoking must be stopped before FGS (nicotine and tar activate the production of gastric juice and mucus).
For the same reasons, it is also necessary to maintain an hour-long period without smoking after the examination.
Peculiarities
The individual characteristics of the preparation should be explained by the doctor. We will just look at the main points.
- How to prepare for gastroscopy in the morning. Typically, the endoscopist begins the appointment around 9 am. Therefore, if you were prescribed the procedure in the morning, your last meal should be at 19-20 pm the previous day. Although it is recommended not to eat 8-10 hours before, the resulting gap is explained by the fact that after dinner you will go to sleep at night around 22 pm and have a good rest. If you have dinner at 12 am, healthy sleep will occur no earlier than 2 am.
- How to prepare for a gastroscopy in the afternoon. If the procedure is scheduled around 1-3 p.m. or in the evening, then a very light breakfast is allowed at 6-7 a.m. You should not eat food that coats the walls of the stomach, such as oatmeal. Limit yourself to a baked apple with a glass of weak tea.
- If a biopsy is planned. This procedure does not require a special approach. However, you should not take blood thinning drugs : aspirin (acetylsalicylic acid), warfarin, pentoxifylline, cardiomagnyl, rheopolyglucin, etc. You should avoid taking Citramon, as it contains not only caffeine, but also acetylsalicylic acid.
- If FGDS simultaneously with colonoscopy. This combination is called combined diagnostics. It is performed only under anesthesia. Preparation begins 4 days before the study: diet described earlier; fasting for 12 – 14 hours before the procedure; Avoid drinking an hour before diagnosis; on the eve of the study, Fortrans or an enema is prescribed.
For patients with diabetes and bronchial asthma
If you suffer from bronchial asthma, use your inhaler on a schedule. You should also inhale one dose of the drug 5-10 minutes before the procedure. Do not use nebulizers before the procedure, as they may stimulate the formation of bronchial secretions. Take your inhaler with you.
Patients with diabetes must agree in advance on the exact time of the procedure , since insulin intake depends on this. If the procedure is in the morning, the patient does not eat, but takes food with him. You should also take insulin with you. After the procedure you should eat. When performing fibrogastroduodenoscopy during the day, the patient has breakfast and receives a dose of insulin according to his usual schedule. Then the procedure is carried out after 4-5 hours.
Diet before FGS of the stomach
Diet recommendations should not be neglected, since even a minor error can lead to difficulties during the study. The diet before FGD of the stomach, first of all, takes into account the intake of warm food with a soft consistency and small portions.
What can you eat before FGS of the stomach?
The final meal before gastroscopy should be 19 hours (in the most extreme case - 12 hours before the start of the procedure).
If the diagnosis is carried out in the afternoon, then 8 hours before it you can allow yourself a light breakfast. The liquid can be drunk 3 hours before FGS, but its amount should not exceed 100 ml.
However, nutrition before FGS of the stomach is a purely individual topic. And what you can and cannot eat, how much not to eat before gastroscopy, the attending gastroenterologist should say exactly at the stage when the patient is preparing for the study.
Example of a light dinner
In the evening you can eat, for example: steamed vegetables with boiled fish or rabbit (serving no more than 350 grams). For the next 12 hours, fasting is observed.
A light dinner before FGS of the stomach means that in 12 hours the stomach has time to process the food eaten.
Indications for the procedure
What is the purpose of the research? Indications for prescribing gastroscopy are:
- Painful sensations in the abdominal cavity of unknown etiology, recurring with a certain frequency.
- Symptoms of obstruction of the esophagus.
- Foreign body in the digestive canal or suspicion of its presence.
- Regular heartburn and belching of air or acidic stomach contents.
- Appetite disorders.
- Suspicion of gastric cancer, inflammatory processes and ulcerative lesions of the mucous membrane.
- The need for examination before abdominal surgery.
- Critical weight loss of unknown origin.
- Diseases of the liver, pancreas and other gastrointestinal organs.
- Persistent nausea.
- Other indications are at the discretion of the attending physician.
FGS of the stomach under anesthesia
The use of anesthesia during gastroscopy is possible not only if there are indications, but also at the request of the patient (if there are no contraindications for it).
FGS of the stomach with anesthesia is recommended:
- during surgery;
- children from 3 to 6 years old;
- sensitive and receptive people.
After gastroscopy with the use of drugs for anesthesia, the patient requires a recovery period and several hours to be under medical supervision, therefore, the length of stay in the institution and the cost increases.
There is an alternative option for the procedure under anesthesia - this is FGS with sedation (i.e., during sleep). Sedation (putting the patient into a half-asleep state exactly for the duration of the procedure using “laughing gas”) eliminates the moral and physical inconveniences of gastroscopy: salivation, gag reflex, etc. After it, you cannot immediately get behind the wheel of a car.
How to check the stomach without FGS in an adult?
When examining the hollow organs of the digestive system (without swallowing the tube), the following are used:
- X-ray;
- Ultrasound;
- computed and magnetic resonance imaging.
These methods have one significant drawback - a limited list of diagnosed diseases of the esophagus, stomach and duodenum. They do not provide a visual picture of the mucous membrane of the esophagus, stomach and intestinal wall (except in cases of large ulcerative lesions).
An alternative to FGS can only be capsule endoscopy - an innovative method that uses a capsule with a video camera to examine the digestive tract.
However, it also has its drawbacks - it is an expensive procedure, there is no way to take a biopsy sample, the camera is not controlled (dangerous lesions can be missed), if bleeding is detected, you will still have to resort to invasive manipulations, sometimes the capsule is removed using an endoscope.
Unfortunately, to the question: “What can replace FGS?” – there is only one answer: It is not possible to check the condition of the esophagus, stomach and duodenum with the provision of adequate therapy without FGS or FGDS.
When and why is FGDS needed?
Gastroscopy is prescribed to people with suspected ulcers, oncological processes of the gastrointestinal tract, gastritis, as well as in the presence of negative symptoms:
- lack of appetite;
- sudden weight loss;
- burning in the throat, sternum;
- feeling of acidity, bitterness, nausea, vomiting;
- anemia;
- difficulty swallowing;
- pain, heaviness in the epigastric zone.
During the examination, using an endoscope, it is possible to identify neoplasms, hidden bleeding, and ulcerations of the mucous membrane in the area of the esophagus, stomach, and duodenum. If needed? material is taken from these tissues for further research or special preparations are administered.
The duration of the manipulation is no more than 10 minutes. If necessary, local anesthesia is used.
Can the procedure be stopped? if the patient has serious pathologies of the esophagus and there is a risk of perforation, or when the preliminary preparation for the examination was carried out poorly.
Important recommendations: how to prepare for gastric FGS
Proper preparation for the examination is the most important condition for effective gastroscopy!
Attention!
Errors at the stages of preparation for FGS complicate the procedure, reduce its comfort and information content!
To avoid mistakes, you need to carefully listen to the recommendations of a gastroenterologist, who will explain how to prepare for FGS of the stomach, what you should not eat, and also how to go through this procedure comfortably.
Step-by-step preparation for the FGS is divided into general and local events.
General preparation for FGS is the doctor’s area of responsibility:
- Identification of possible contraindications to FGS.
- Assessing and weighing possible risks.
- Drug correction of conditions potentially dangerous for the procedure (severe angina, arrhythmia, arterial hypertension, respiratory failure, bleeding after minor operations with low platelets in the blood test, etc.). Corrective therapy is prescribed several days before the procedure.
- Elimination of possible allergic reactions to local anesthetics. Be sure to report any allergic reactions to medications.
- Identification of diseases that may affect the choice of drug preparation for the study (for some pathologies, the use of certain medications is contraindicated). Provide the doctor with all required medical documentation.
- Psychological preparation consists of developing an optimistic attitude. This will reduce discomfort during insertion of the gastroscope. If a person cannot overcome fear, the doctor prescribes sedatives and sedatives.
Effective preparation for FGDS includes the following steps:
- Report all medications you take. Due to the procedure, your medication regimen may change or temporary discontinuation may be necessary.
- If the patient has esophagitis or inflammatory diseases of the upper respiratory tract, appropriate therapy is prescribed. Sanitation of these pathways is important for smooth insertion of the endoscope.
- 2-3 days before the test, completely eliminate alcohol, fried and fatty foods, and foods that cause flatulence should be removed from your diet. To prevent flatulence and disturbances in the passage of food, enzyme preparations and sorbents are prescribed. For example: Creon, Espumisan, Enterosgel, etc.
- Dinner the night before the FGS should be no later than 18.00-19.00 hours.
- On the morning of the test, you should not eat anything (if the test is scheduled before lunch).
- You cannot drink sparkling mineral water.
- In the morning you can: brush your teeth, take lozenges in your mouth.
- To undergo the procedure, prepare comfortable clothes in which you can lie down, bend your legs and not be embarrassed.
- There is no need to paint your eyelashes and lips before the procedure. Makeup can deteriorate and cause inconvenience to the doctor during manipulations.
By undergoing FGS or FGDS, you give the attending physician the opportunity to make a diagnosis as accurately as possible and create an effective treatment regimen for the identified pathology. Remember that proper preparation is a responsibility shared by two people: the patient and the doctor.
© The material was prepared with the participation of doctor, candidate of medical sciences Stepura V.P.