What is sedation and what is the difference with general anesthesia?
Currently, the terms “anesthesia” and “sedation” are often confused , although these are somewhat different conditions. Even anesthesiologists do not always draw a clear line between these concepts.
Anesthesia is a technique of general anesthesia in which the patient is unconscious and drugs are used to relieve pain.
Mechanical ventilation is only necessary when muscle relaxants are used. And these drugs are given only for certain types of surgical interventions (for example, in neurosurgery, thoracic surgery, etc.). There is no need for them to carry out FGDS, and therefore anesthesia in such a situation does not look so scary.
Removal from this state occurs gradually. After stopping the medication, sleep usually lasts another 30 minutes to several hours.
Sedation is a patient’s condition that is most similar to the term “medicated sleep . In fact, it is one of the components of anesthesia (but without painkillers or muscle relaxants) . It is theoretically possible to put a patient under sedation with a single intramuscular injection. When performing FGDS, medications are used intravenously, which allows more accurate control of the depth of sleep.
To introduce the patient into this state, drugs from the group of benzodiazepines are used. These medications have pronounced hypnotic and anticonvulsant effects .
At the same time, they suppress the emotional component, which allows the patient to undergo the necessary procedure calmly and without fear. When administered intravenously, the effect occurs within 1-2 minutes.
Over many years of implementation, sedation has proven itself to be the best. Now this is a completely common and everyday technique. Patients tolerate it very well, and within a few hours they are completely back to their normal activities. And therefore it is carried out not only in specialized hospitals, but also in regular clinics or private diagnostic centers.
The main characteristics, advantages and disadvantages of the techniques are displayed in the following table:
| Anesthesia | Sedation | |
| Characteristic | Deep sleep with suppression of the gag reflex and pain sensitivity | Severe drowsiness, decreased emotionality |
| Number of drugs used | Several (usually 2-3) | One |
| Types of drugs | Sedatives, narcotic analgesics, muscle relaxants | Benzodiazepines (sedatives and hypnotics) |
| Wake up time | From 15 minutes to 2 hours | A couple of minutes |
| Complications after the procedure | Severe drowsiness, confusion, nausea, lack of coordination | Drowsiness, dry mouth, hiccups (pass quickly) |
10 recipes for treating gastritis in this article.
Indications for medicated sleep during gastric endoscopy
Sedation for fibrogastroduodenoscopy is indicated in the following cases:
- severe anxiety of the patient before the procedure;
- history of epileptic seizures
- Parkinson's disease;
- tendency to panic attacks.
Anesthesia is performed if , surgical intervention is planned (for example, stopping active gastric bleeding). This method is also preferable against the background of brain injuries and tumors affecting the central nervous system.
Help A separate indication for performing FGDS is the patient’s desire. Often he does not want to feel discomfort or pain during diagnosis, and if there are no contraindications, then they accommodate him.
Preparation
If anesthesia is required, the preparation is more thorough than for conventional gastroscopy. Over the course of a few days, a set of examinations is carried out to study the functioning of the main body systems:
- general blood analysis;
- biochemical blood test (sugar, glycated hemoglobin, bilirubin and its fractions, urea, creatinine with determination of glomerular filtration rate, total protein);
- X-ray of the chest cavity (if there are indications for pulmonary pathology);
- electrocardiography (in patients over 40 years old).
Both before sedation and before anesthesia, if there are concomitant pathologies, the degree of their compensation is determined. Tests are required to determine the presence of allergic hypersensitivity to the drugs that are planned to be used.
Important If a patient has diabetes, he or she needs to be switched to insulin injections for a short period of time.
Preparation necessarily includes a certain diet. The day before FGDS, the patient is advised to eat easily digestible food. The study is carried out on an “empty” stomach.
On the day of diagnosis, you are allowed to drink table water, but no later than an hour and a half before the start. In the morning, the patient takes all previously prescribed medications. If additional colonoscopy is required, then bowel cleansing (with the help of diet and laxatives) is first indicated.
To avoid complications, it is recommended to follow a diet after the procedure.
Features of preparation for gastroscopy under anesthesia
To undergo an FGDS with anesthesia without any health risks, the patient, in addition to the standard diet, will have to follow a number of other recommendations. At least a week before the study, a number of additional studies will have to be completed against the background of medicated sleep:
- take a blood test for coagulation and a general blood test;
- undergo tolerance tests for certain types of anesthetics;
- undergo electrocardiography;
- get advice from a therapist, and in the case of chronic diseases, from specialists.
Also, preparation for gastroscopy under anesthesia contains more stringent nutritional conditions on the eve of the procedure. If it is planned to use general anesthesia during FGDS, the patient on the eve of the examination will have to refuse not only food, but also drink. For gastroscopy in a dream, the same rules apply: you can only drink water the night before, and in the morning, 2-4 hours before the procedure, you can only wet your lips so as not to feel very thirsty.
Important! Before performing an FGDS under anesthesia, it is forbidden to take even medications recommended by a doctor. If they are vital, and omissions may negatively affect the condition, the possibility of taking them should be discussed with a gastroenterologist and anesthesiologist.
How is sleep research done?
Mechanical ventilation is not required during sedation, nor is urinary catheterization.
Sedation, unlike anesthesia, can be carried out in a regular manipulation room.
Since the patient is put under anesthesia in situations where, after receiving the results of FGDS, the possibility of surgery is envisaged, the manipulation is carried out in the operating room. Then the anesthesiologist monitors the patient's condition.
It is important that the room is equipped with everything necessary to monitor the patient’s condition.
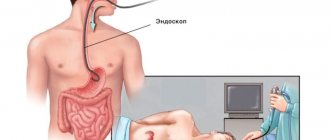
The patient lies down on a special couch. The necessary drugs are administered intravenously. After achieving medicated sleep, the endoscopist gradually inserts a probe equipped with a video camera through the mouth. Alternately, he examines the inner walls of the duodenum, stomach and esophagus. A rapid test is performed for the presence of Helicobacter pylori infection.
If an ulcer, neoplasm or significant changes in the mucous membrane are detected, a tissue sample is taken for cytological examination. The device also measures acidity parameters in various parts of the digestive system.
The duration of the manipulation is 5-10 minutes.
What is FGDS and what pathologies does the examination reveal?
FGDS is a modern method for studying the human digestive system, during which the condition of the mucous membrane is studied and pathological changes in the structure of epithelial tissues are detected.
With the help of fibrogastroduodenoscopy, it is possible to perform not only high-quality diagnostics of the gastrointestinal tract, but also to select samples of biological material for the purpose of further laboratory research.
Carrying out FGDS involves the use of special medical equipment in the form of a gastroscope, the component of which is a probe equipped with a digital video camera.
A distinctive feature of fibrogastroduodenoscopy is that, compared to other methods of endoscopic examination, this type of diagnosis allows one to study the functional state of the stomach and the walls of the duodenum. In some cases, FGDS is used to study the biliary tract.
Using FGDS, you can detect pathologies of the gastrointestinal tract:
- erosion of the mucous membrane;
- polyposis;
- pyloric stenosis;
- benign and cancerous tumors;
- gastritis, accompanied by atrophic and degenerative processes in the gastrointestinal tract;
- Crohn's disease;
- ulcerative lesions of the stomach, as well as the mucous membrane of the duodenum.
Fibrogastroduodenoscopy reveals any changes in the external condition of the walls of the stomach and duodenal cavity. In most cases, conducting this type of study is enough to make an accurate diagnosis of the presence of a particular disease of the digestive system.
Features of the procedure in children
Typically, sedation or anesthesia is used for children under 6 years of age when they react negatively to the offer to undergo an endoscopic examination.
Anesthesia for a child allows the doctor to carry out diagnostics in a calmer environment without external pressure, reduces the risk of accidental injury (due to sudden movements of the baby) and improves information content .
But on the other hand, it is necessary to take a more careful approach to calculating the required dosage of drugs. Here the specialist takes into account the child’s age and body weight.
Contraindications
Anesthesia during FGDS is dangerous if the patient has the following conditions:
- allergic reaction to drugs used for anesthesia;
- hemorrhagic stroke in the last 6 months;
- signs of heart failure;
- acute myocardial infarction (or unstable angina);
- diseases of the respiratory system, which are accompanied by a decrease in blood oxygen saturation (pneumonia, bronchial asthma, COPD);
- severe anemia;
- congenital or acquired (for example, while taking medications) blood clotting disorders;
- severe renal failure (decrease in glomerular filtration rate below 30 ml/min);
- high blood pressure;
- uncompensated diabetes mellitus (a preliminary switch to insulin is required);
- unstable hemodynamics (compensation state required).
Additionally, it is necessary to take into account the characteristics of the drugs that are planned to be used to induce anesthesia for the patient.
Contraindications for performing FGDS under sedation are almost identical to those under anesthesia.
barbiturates are almost always used . These are similar to barbituric acid, which have a pronounced inhibitory effect on the central nervous system.
They cannot be used if the following conditions exist:
- glaucoma (risk of increased intraocular pressure);
- intolerance to benzodiazepines;
- pregnancy period;
- recent use of alcoholic beverages or drugs;
- myasthenia gravis;
- hypercapnia (increased carbon dioxide levels in the blood);
- psychical deviations;
- sleep apnea syndrome (episodes of stopping breathing due to snoring);
- impaired liver function (cirrhosis, hepatitis, cancer);
- coma state.
If a patient has contraindications for the administration of anesthesia, he should pay attention to methods that will make it easier to tolerate FGDS or try other research methods, for example, an x-ray of the stomach.
Contraindications to the use of various types of anesthesia
All types of anesthesia have contraindications, which are also taken into account by the doctor when choosing an anesthetic for gastroscopy. The use of any type of anesthesia for FGDS is impossible if the drugs are intolerant. Local “freezing” can cause swelling of the larynx, which can cause asphyxia. To make sure there is no allergic reaction, an allergy test must be performed before using them. If it is not possible (for example, the procedure is performed urgently), local anesthesia during gastroscopy is replaced with sedation.
The EGD procedure during sleep also has a list of contraindications. These include:
- pregnancy;
- early childhood (up to 3 years);
- neuromuscular diseases and epilepsy;
- hyperexcitability;
- increased cranial pressure.
Any sedative drug that is used to perform FGDS during sleep becomes dangerous when used against the background of alcohol intoxication. Therefore, when a patient is admitted for an emergency gastroscopy in a drunken state, the option of medicated sleep is not considered by doctors as a priority method of pain relief.
General anesthesia for FGDS has more extensive contraindications than drug-induced sleep and local “freezing”. In addition to the previously listed health disorders, these include heart disease, acute inflammatory and infectious processes in the oropharynx and larynx, and pulmonary diseases.
Possible complications
Sedation is usually easy to tolerate. The patient wakes up within 3-5 minutes after completion of the procedure. He remains under medical supervision for about another hour, and then he can safely go home.
On the day of the study, he is prohibited from driving or doing work that requires increased concentration or precise movements. Among the complications most often noted:
- allergic reactions to the drug;
- dizziness;
- general weakness;
- decreased performance;
- drowsiness;
- decreased blood pressure (hypotension), increased heart rate (tachycardia);
- decreased clarity of vision;
- emotional lability (state of anxiety, depressed mood);
- feeling of dry mouth, hiccups, decreased appetite.
Side effects from sedation usually go away quickly. And by the end of the day the patient feels as usual.
Help The period after the introduction of anesthesia is much more difficult. The awakening process lasts from 30 minutes to 2 hours. During the day, the patient must be under close medical supervision.
The most common complications that occur are:
- allergic reactions;
- respiratory depression;
- aspiration pneumonia (due to stomach contents entering the respiratory tract);
- nausea and vomiting;
- tremor (shivering) of the hands and feet;
- pain in the head and peripheral muscles;
- drowsiness;
- fluctuations in blood pressure;
- burning sensation of the skin;
- increased blood sugar levels;
- psychoemotional disorders;
- impaired coordination of movements, pronounced swaying when walking;
- difficulties in orientation in space and time.
The process of returning the patient to a normal state is longer. Some side effects from medications can last up to 48 hours.
Local anesthesia
As already mentioned above, for this type of anesthesia, drugs based on lidocaine and its analogues are used. The advantages of this method are the patient’s clear consciousness and the possibility of his reaction to sharp pain in the stomach or duodenum, for example, if damaged by an endoscope. Lidocaine and its derivatives do not lead to complications and are well tolerated by patients, with the exception of individual intolerance.
The drug reduces the gag reflex, which slightly calms the person undergoing the examination. After the procedure, the effect of the anesthetic used wears off within approximately 20 minutes, and this allows the patient to immediately go about his business, including driving a car. This method is suitable for gastroscopic examination, and in parallel with any surgical or therapeutic measures, the following types of anesthesia are more often used.
Drugs used
For sedation, medications from the group of benzodiazepines are used. In domestic conditions, diazepam is most often used.
This drug has pronounced hypnotic and anti-anxiety effects. Diazepam is also effective in preventing cramps and relaxing peripheral muscles. The drug is administered intravenously or intramuscularly 10-15 minutes before the start of the procedure.
Benzodiazepines tend to accumulate in the body and the patient becomes addicted to them . However, this happens with regular daily use . Even if endoscopic examination is performed under sedation every week, these effects do not develop.
When performing FGDS, it is impossible to use inhalation medications for anesthesia, so they are administered exclusively intravenously . Typically, several medications are needed:
- A general anesthetic is a drug that acts on the synapses of the brain in such a way that the patient is immersed in a deep sleep-like state. In practice, representatives of several pharmacological groups are used: barbiturates (thiopental, hexobarbital), NMDA agonists (ketamine), phenol compounds (propofol).
- Narcotic analgesic - used to completely relieve pain in the patient and suppress the gag reflex (although the drug itself can cause nausea as a side effect). Modern analgesics are all from the opioid group. Main drugs: ramifenthalil, sufentanil.
- Muscle relaxant (usually peripheral action) - used for FGDS very rarely. They affect the transmission of nerve impulses to peripheral muscles, which leads to their relaxation. The main disadvantage is respiratory depression, so they can be used only in conditions where mechanical ventilation is possible. Modern representatives: Mivacron, Rocuronium Kabi.
Possibility of transition from sedation to anesthesia
In clinical practice, situations sometimes arise when sedation alone is not enough to conduct a diagnostic examination. Then, with careful preliminary preparation, the patient can be put under anesthesia. However, for this the following conditions must be met:
- availability of written consent of the patient or his legal representative (spouse, parents);
- sufficient equipment of the manipulation room for general anesthesia;
- presence and conduct of the procedure by a qualified anesthesiologist;
- conducting a preliminary test for the absence/presence of an allergic reaction to drugs that will be used for anesthesia;
- lack of a simpler diagnostic alternative (presence of an emergency condition).
In the opposite direction, the patient is practically not transferred from anesthesia to sedation.
Cost of FGDS under anesthesia, where to do it
The table below shows the average cost of FGDS with anesthesia, as well as the types of institutions that conduct this type of diagnosis.
| Where to do fibrogastroduodenoscopy | Average cost of examination |
| State clinic | In state-owned medical institutions, this type of diagnosis is free, but a referral from the attending gastroenterologist is required. |
| Private clinic | 3450 rub. |
FGDS is a modern method of diagnostic examination of the upper gastrointestinal tract, which allows you to detect the painful condition of the digestive system. Fibrogastroduodenoscopy is performed under local anesthesia. In 98% of cases, local anesthetic sprays are used, which are applied directly to the surface of the throat mucosa.
The average duration of FGDS ranges from 20 to 40 minutes. depending on the health of the patient’s stomach and duodenal walls. The high information content of this diagnostic method is confirmed by positive reviews from patients.
Gastroscopy and colonoscopy in one session
Most often, FGDS and colonoscopy (FCS) are prescribed in the presence of bleeding in the digestive tract of unknown localization. Therefore, they can be completed simultaneously during a session of sedation or anesthesia . However, the following nuances need to be taken into account:
- The time required to complete the diagnostic program will be significantly longer (more than 1 hour).
- Additional preparation is required before a colonoscopy - the use of laxatives, cleansing enemas and diet.
- Colonoscopy has its own contraindications (violation of intestinal integrity, peritonitis, diverticulitis).
There is a common belief that colonoscopy under sedation should not be performed because the patient cannot communicate when he or she is in pain. Supposedly, this prevents damage to the intestinal wall.
However, the frequency of injuries during endoscopic research methods depends solely on the qualifications of the doctor who conducts them . Whether he will use “medicated sleep” or not does not matter.
You can also find this information in the video:
Complications after FGDS
Fibrogastroduodenoscopy is a safe procedure that extremely rarely causes negative consequences.
Violation of the examination protocol and errors on the part of the doctor performing the diagnosis can lead to the following complications:
- damage to the walls of the stomach and duodenum;
- opening of bleeding inside the gastrointestinal tract;
- infection of the digestive system by pathogenic microorganisms (if the rules of sterility of medical equipment were not followed);
- rupture of the esophagus, the elimination of which requires surgical treatment;
- perforation of the stomach or duodenum;
- deep damage to the gastrointestinal mucosa with further development of the ulcerative process;
- cardiac arrest or paralysis of the muscles responsible for the act of breathing (this complication occurs in patients whose central nervous system is suppressed by general anesthesia).
Patients who, after completing FGDS, feel severe pain inside the abdomen, chest, find blood during bowel movements, or experience dizziness, should immediately seek medical help. The appearance of such symptoms indicates the presence of complications of fibrogastroduodenoscopy.
Where can I make it and what is the best price?
The greatest opportunities for undergoing FGDS under anesthesia or sedation are in Moscow . In the capital, more than 100 public and private clinics conduct this medical examination. After making an appointment, a preliminary consultation with a specialist will be required, during which he will examine the patient, conduct tests for allergies to medications and explain the main nuances of preparation. The cost of diagnostics is 2-3 times higher than the price of a regular FGDS and ranges from 5-13 thousand rubles . a colonoscopy is also performed at the same time , then the cost increases by 3-6 thousand rubles.
In St. Petersburg, examination can be done in more than 50 medical centers. The price of FGDS under sedation or anesthesia in private clinics ranges from 3.6 (Ambulance) to 14.2 (Euromed Clinic) thousand rubles. If the patient wishes, it is possible to perform a colonoscopy in one session for 7-20 thousand rubles.
Also, FGDS under anesthesia is carried out in 20 medical institutions of Kazan (Hospital No. 7, City Children's Hospital No. 1, and others). The cost is 4.5-12 thousand rubles. An additional colonoscopy will cost 3-5 thousand rubles.
In Yekaterinburg, FGDS under sedation can be performed in several private medical, Paracelsus) and public hospitals. The price of diagnostics is 5-9 thousand rubles, and with colonoscopy – 8-13 thousand rubles.
Why is the procedure done under anesthesia?
Fibrogastroduodenoscopy is performed under local or general anesthesia in order to obtain the following result:
- reduce the patient’s discomfort as the gastroscope probe moves into the larynx;
- eliminate the manifestation of pain at the time of damage to the mucous membrane of the esophagus;
- prevent the occurrence of panic and feelings of fear.
- prevent the gag reflex and cough;
FGDS under anesthesia is quick and comfortable. Patients who undergo this type of examination using local anesthesia have only positive reviews and also indicate a complete absence of pain.