How to distinguish constipation from intestinal obstruction?
When a person is constipated, a number of symptoms occur:
- Inability to go to the toilet for several days. During defecation, you have to strain very hard, use physical assistance or medications.
- There is an abundant accumulation of gases in the abdomen, which cause flatulence.
- Abundant accumulation of feces causes a feeling of discomfort in the abdomen.
When the body cannot get rid of feces, a blockage has formed somewhere. This is why constipation is a symptom of obstruction.
Intestinal obstruction (symptoms in adults may vary depending on the type of illness) occurs with the first symptoms like constipation , with the addition of new ones:
- Severe abdominal pain. They are accompanied by painful cramps in the abdomen. They arise abruptly, and there is no clear understanding of the location of the pain.
- Partial swelling. There is a clear swelling of a certain part of the abdomen where the obstruction has formed.
- Nausea and vomiting. This happens due to poisoning of the body. Long-term intoxication of the body can worsen the patient’s condition and contribute to death.
Constipation indicates the presence of partial obstruction. The main difference is that constipation is a more tolerant form of obstruction that can be treated with medication.
How to treat intestinal obstruction in older people
Taking any independent action is strictly prohibited! Giving an enema and taking painkillers will not lead to a positive result; they can worsen the situation. You need to urgently go to the hospital for help. They will empty the abdominal cavity with a probe by inserting it into the mouth or nose. If necessary, antispasmodics are prescribed, a novocaine blockade is performed, and a siphon enema is administered.
If droppers with saline solutions do not help (this indicates a mechanical type of pathology), then an emergency operation is performed.
What should relatives do at the first symptoms of the disease in elderly people?
Place the patient on a comfortable bed and place a basin near him to collect the vomit. Call an ambulance, do not take any further action. Do not give painkillers or laxatives under any circumstances.
Causes of constipation
The movement of food occurs due to contraction of the intestinal walls. Impaired peristalsis may be accompanied by relaxation of the muscle layer or prolonged spasms. The cause of the onset of the disease may be:
- surgical intervention;
- taking medications;
- accompanying illnesses;
- formation of nodules, twists;
- tumors;
- hernias;
- the presence of stones in the gall bladder;
- entry of foreign objects;
- bruises, hematomas;
- rib fractures;
- problems with blood vessels;
- traumatic brain injuries;
- presence of helminths.
Symptoms of intestinal obstruction in older people
An elderly person begins to complain of pain in the abdomen, first points to a certain area, then begins to feel painful spasms throughout the entire volume of the peritoneum. At this time, nausea begins, and later vomiting appears. Trying to go to the toilet leads nowhere. On the contrary, diarrhea may develop. The worst thing is if it occurs with blood inclusions. The face and body are covered with cold sweat, the skin becomes noticeably pale, and the person assumes a “fetal” position. He may lose consciousness from pain and intoxication. In such cases, he urgently needs to be taken to the hospital or an ambulance is called. Most likely he will have surgery.
Types of intestinal obstruction
| View | Characteristic | Classification |
| Acute | Impaired release of digested food from the stomach to the anus. This is a collective term that combines a number of intestinal diseases in a complicated form. Requires mandatory medical intervention; if left untreated, death is possible. | |
| Partial | Occurs when the passage of feces through the intestines is disrupted; this process is chronic. The reasons for its occurrence may be related to: neoplasm, postoperative period or adhesive disease. | The disease occurs in a periodic manner. At the moment of exacerbation, the following appears: increased accumulation of gases, stool disturbances, pain, nausea. |
| Paralytic | There is a deterioration in the functioning of the intestinal muscles and a decrease in tone, and complete paralysis is also possible. This situation does not arise independently; it appears due to a number of serious diseases. | The disease occurs in several directions:
|
| Obstructive | Poor output of intestinal contents that does not involve the mesentery. Compression occurs in the intestinal tube due to factors acquired during life. | Blockage occurs due to the impact of a foreign body. It forms both inside the intestine (fecal or gallstones, tumors) and outside (cyst, tumor).
|
| Mechanical | A closure of the intestinal tube is created in a separate area, and the exit of the intestinal contents is blocked. |
|
CONGENITAL INTESTINAL OBSTRUCTION
Congenital intestinal obstruction in children accounts for 10-15% of the total number of acute intestinal obstruction.
In newborns, the etiological factors of congenital intestinal obstruction are malformations of the intestinal tube in embryogenesis (atresia, stenosis, duplication), defects that are associated with impaired innervation and blood supply of the intestinal tube (congenital pyloric stenosis, megaduodenum, neurogenic ileus and Hirschsprung's disease), rotational anomalies and those , which develop as a result of incomplete rotation of the intestinal tube - Ladd syndrome (volvulus of the midgut with compression of the duodenum by peritoneal cords that fix the high-lying cecum).
One of the causes of congenital intestinal obstruction may be developmental anomalies of other organs. This is an abnormal development of the pancreas, which covers the duodenum in the form of a clamp, which narrows its lumen, an aberrant vessel, diaphragm defects, cysts and tumors, anomalies of the vitelline duct.
Malformations of the intestinal tube are formed during the period of organogenesis - the first 3-4 weeks of intrauterine development, when the processes of formation of the intestinal wall and intestinal lumen occur. During development, the intestinal tube goes through the stage of epithelial proliferation, as a result of which the intestinal lumen completely closes. In the future, the process of vacuolization should normally lead to the restoration of its lumen, but under certain conditions this phase is disrupted and the lumen of the intestinal tube remains closed. If recanalization is impaired in a small area, it is closed by a thin membrane - membranous atresia. If the lumen of the intestinal tube closes over a long distance, atresia is formed in the form of a fibrous cord. Sometimes it occurs due to underdevelopment of the corresponding branch of the mesenteric vessels.
Atresia can be single or multiple. More often, these defects occur in areas of complex embryonic processes - the major duodenal papilla, at the junction of the duodenum and the small intestine, in the distal ileum.
The transition from the primary embryonic position - the phase of physiological embryonic hernia - occurs by rotation of the intestinal tube. Disruption of this process (its delay) at different stages leads to the occurrence of various defects, which can be the cause of intestinal obstruction. In case of delayed rotation at the first stage, the child is born with incomplete rotation of the intestines. In this case, the midgut (from the duodenum to the middle of the transverse colon) remains fixed at one point in the projection of the origin of the superior breech artery. The loops of the small intestine are located in the right half of the abdominal cavity, the cecum is located in the epigastric region under the liver or in the left hypochondrium, and the large intestine is on the left. As a result of this fixation, conditions arise for the development of volvulus around the root of the mesentery and for the development of acute strangulation intestinal obstruction.
If the second stage of rotation is disrupted, the cecum, which is located in the epigastric region, is fixed by embryonic cords in front of the duodenum, compressing it. A possible combination of compression of the duodenum and volvulus around the superior mesenteric artery - Ladd syndrome is complete, in the absence of volvulus - incomplete. The atypical location of the cecum along with the appendix complicates the diagnosis of acute appendicitis in older children and even adults.
If the third stage of turnover is disrupted, the fixation of the intestinal loops changes, which leads either to the formation of folded defects or to the formation of various depressions and pits in which the intestinal loops can be pinched. Accordingly, such anomalies are considered false or true internal hernias.
Developmental anomalies of other organs that lead to intestinal obstruction are special in nature. Meconium ileus occurs due to congenital cystic fibrosis of the pancreas. Insufficient enzymatic activity and the absence of pancreatin contribute to an increase in the viscosity of meconium, which clogs the lumen of the ileum in front of the ileocecal valve (bauginian valve).
According to the classification of S.Ya. Doletsky , during the diagnosis and determination of treatment tactics, it is necessary to take into account the types of congenital intestinal obstruction, namely complete and partial, which in turn is divided into high, small intestinal and low - large intestinal.
The following malformations are classified as high: atresia of the duodenum, the initial part of the small intestine; internal stenosis of the duodenum, external stenosis - Ladd syndrome or its individual components; ring-shaped pancreas; aberrant vessel.
Small intestinal include: ileal atresia, internal ileal stenosis, duplication (enterocystoma); strangulation in a congenital defect of the mesentery; true internal hernias; isolated midgut volvulus; false internal hernias; meconium ileus.
Anorectal malformations are classified as low.
According to the classification of G.A. Bairov, these defects are divided into acute, chronic and recurrent. Each of them refers to high or low intestinal obstruction.
Prenatal diagnosis of congenital intestinal obstruction consists of determining the level of α-fetoprotein, ultrasound, and examining the amniotic fluid for karyotype. All this allows, in some cases, to detect a risk group among pregnant women and raise the question of terminating the pregnancy.
Polyhydramnios occurs in 50% of all cases of high intestinal atresia; its presence is an indication for fetal ultrasound.
An increase in the concentration of bile acids in the amniotic fluid during polyhydramnios is a diagnostic sign of intestinal atresia.
Another technique involves collecting amniotic fluid and is called amniocentesis. To enter the amniotic cavity, a needle is used to pierce the mother's abdominal wall and uterus and approximately 20-50 ml of fluid is removed. This procedure is usually not performed until the 14th week of pregnancy due to insufficient fluid supply before this time. The fluid is analyzed for α-fetoprotein. This substance is a fetal protein, which is present in high concentrations in the amniotic fluid with abdominal defects, gastroschisis, and omphalocele. This protein is also present in maternal serum, where it can be detected, although with less certainty than in amniotic fluid.
The clinical picture of congenital intestinal obstruction largely depends on the level and type of intestinal obstruction. With high intestinal obstruction in newborns, from the first hours of life, vomiting occurs, sometimes continuously, with bile impurities, if the obstruction is localized below the major duodenal papilla (Fig. 1, 2). The phenomena of exicosis and aspiration pneumonia develop very quickly. Children with high congenital intestinal obstruction usually experience meconium passage. If the site of the obstruction is located higher from the major duodenal papilla, the amount and color of meconium are unchanged and its discharge is observed on the 4th day. With low intestinal obstruction, the amount of meconium is much less, its consistency is more viscous, grayish in color. These features are due to the impossibility of passage of bile and amniotic fluid into the distal parts of the intestines. With atresia and subtotal stenosis, there is a one-time discharge of altered meconium or discharge in small portions during the first 2 days.
Rice. 1. Types of duodenal membranes (according to G. A. Bairov): by type: a - solid; b, c - multiple; by localization: d - suprapapillary; d - infrapapillary; in shape: e - transverse; g - leukoid; h – saccular.
Rice. 2. Options for impaired patency of the duodenum with malformations of the pancreas (scheme according to G.A. Bairov):
a - ring-shaped pancreas;
b — claw-shaped head of the pancreas;
c - an additional lobule of the pancreas in the wall of the duodenum, which narrows the intestinal lumen
The behavior of a child with high intestinal obstruction on the 1st day is normal. As the general condition deteriorates, the child refuses to feed.
In dynamics, there is a progressive decrease in body weight to 250 g in the 1st day. On the 2nd day, the first signs of dehydration appear.
A change in the configuration of the abdomen is determined. In the upper sections (epigastric region) it is swollen, in the lower sections it is sunken. The abdomen is usually soft and painless. In the presence of intestinal volvulus, the child is restless, the abdomen is tense and painful.
X-ray examination begins with a survey radiograph of the abdominal organs in direct and lateral projections in a vertical position of the child. With high intestinal obstruction, a direct projection shows two gas bubbles with horizontal levels of liquid in a correspondingly distended stomach and duodenum; a similar picture is determined on photographs in a lateral projection. The diagnostic value of the study increases if a barium sulfate solution is administered: 1 teaspoon of barium sulfate is dissolved in 30-50 ml of expressed breast milk. Other parts of the abdominal cavity are not visualized due to the lack of gas in the intestinal loops.
The presence of the indicated x-ray picture and clinical data gives grounds to consider the diagnosis of high intestinal obstruction as undoubted, but for its final confirmation G.A. Bairov suggests performing irrigography (40-60 ml of water-soluble contrast agent) to clarify the location of the colon. If the colon, which is partially filled with contrast material, is located on the left, the newborn should be considered to have midgut volvulus. Clarifying the cause of obstruction makes it possible to justify the correct calculation of time for preoperative preparation.
Differential diagnosis must be carried out with other congenital diseases that have similar clinical signs.
Pylorospasm manifests itself in the first days after birth by vomiting, which is inconsistent and less frequent than in the case of congenital intestinal obstruction. There is no admixture of bile in the vomit during pylorospasm, as in case of duodenal obstruction above the major duodenal papilla. Survey radiographs in two projections make it possible to clarify the diagnosis due to the symptom of two cups characteristic of congenital intestinal obstruction and the absence (or small amount) of gas in the intestinal loops.
Congenital pyloric stenosis, which is characterized by partial intestinal obstruction, has similar symptoms: swelling of the epigastric region with visible gastric peristalsis, constant vomiting, scanty bowel movements, and malnutrition. At the same time, constant bile staining of stagnant vomit completely excludes the presence of congenital pyloric stenosis in the child. To confirm the diagnosis, an X-ray examination of the abdominal organs is performed, during which a large gas bubble is detected in the projection of the dilated stomach, and a uniform distribution of gas is determined in the intestinal loops. To clarify the diagnosis, an X-ray examination with a contrast agent is performed.
With a congenital diaphragmatic hernia, vomiting may be observed, but signs of dysfunction of the respiratory and cardiovascular systems come to the fore. X-ray examination indicates movement of intestinal loops into the chest cavity.
Birth trauma to the brain is manifested by vomiting mixed with bile, meconium passage is not impaired. In case of brain injury, symptoms of damage to the central nervous system are determined. The diagnosis is confirmed by x-ray and ultrasound.
With low congenital intestinal obstruction, all symptoms of the disease develop more slowly: first, bloating appears, and there is no passage of meconium. After inserting a gas tube or giving an enema, the newborn produces pieces of colorless mucus. Vomiting begins later, from the 3rd day of life. The vomit is colored with bile, then acquires a meconium character and an unpleasant odor - “fecal vomit”. On the 2nd - 3rd day after birth, motor agitation appears, the baby knocks his legs, refuses food or sucks very sluggishly. The condition gradually worsens, symptoms of intoxication increase, the skin acquires a gray-earthy color; the child is lethargic, adynamic, the abdomen is enlarged, intestinal peristalsis increases, and becomes visible through the anterior abdominal wall. Percussion reveals a tympanic tone of percussion sound over the entire abdominal wall, and auscultation reveals rare, dull bowel sounds.
Disturbances in water-electrolyte metabolism and toxicosis develop slowly if there is no necrosis and perforation of the overstretched blind end of the intestine with the development of meconium peritonitis. The child's condition is deteriorating sharply: continuous vomiting, increased body temperature, the anterior abdominal wall is pasty; pronounced venous pattern, soft tissues of the perineum and groin area are swollen and hyperemic. The anterior abdominal wall is tense. A plain X-ray of the abdominal organs shows swollen loops of intestines with multiple levels, which is typical for obstruction of the ileum and colon. In case of obstruction of the jejunum and ileum, meconium ileus, several large gas bubbles and wide fluid levels are determined. Perforation of the dilated section of the intestines above the site of obstruction is radiographically characterized by the presence of free gas in the subphrenic space of the abdominal cavity.
If low intestinal obstruction is suspected, it is advisable to inject a water-soluble contrast agent into the rectum, and a sharply narrowed large intestine is determined by x-ray.
Differential diagnosis of low congenital intestinal obstruction is carried out with paralytic intestinal obstruction and Hirschsprung's disease.
Paretic intestinal obstruction is characterized by a slow onset against the background of a severe underlying disease (peritonitis, pneumonia, sepsis, enterocolitis, etc.). A baby's meconium passes normally after an enema or gas tube. The introduction of a contrast agent into the rectum during an x-ray examination helps in the differential diagnosis, while in case of paretic intestinal obstruction, a well-formed rectum and sigmoid colon with a normal lumen are detected.
In case of Hirschsprung's disease (with the exception of acute decompensation), in contrast to congenital intestinal obstruction, it is possible to achieve the removal of gases and feces using a conservative method (abdominal massage, insertion of a gas outlet tube, administration of an enema). The final diagnosis is confirmed by contrast X-ray examination in two projections - with Hirschsprung's disease, the expansion of the lumen of the colon is determined with the presence of a narrowed zone of aganglionosis.
Chronic intestinal obstruction develops mainly due to stenosis of the duodenum, compression by the annular pancreas or embryonic cords. Stenoses of the distal parts of the digestive system may occur much less frequently, more often due to a tumor process.
Clinical manifestations of partial intestinal obstruction: vomiting occurs, the child is calm, appetite is reduced, body weight does not increase. The diagnosis is confirmed by X-ray contrast examination of the digestive system with barium sulfate (orally). Characteristic is suprastenotic dilatation of the intestine with retention of barium sulfate in it.
Recurrent intestinal obstruction is most often associated with midgut volvulus or intestinal compression in an internal hernia, and has a wave-like course with periods of exacerbation with signs of acute intestinal obstruction. The child is excited, complains of abdominal pain, takes a forced position; in severe cases, painful shock develops.
Palpation reveals sharp pain in the navel area, peritonitis, and increased peristalsis. After an enema, all signs temporarily disappear.
Treatment of congenital intestinal obstruction remains a pressing problem in pediatric surgery. The result of treatment depends on timely diagnosis, adequate surgical correction of the malformation, individual preoperative preparation and rational management of the postoperative period.
If the diagnosis is made in a timely manner, on the 1st day after birth, then preoperative preparation lasts 3-6 hours. A puncture of the subclavian vein is performed (according to Seldinger); the child is warmed, cardiac drugs are administered, oxygen therapy is carried out, a gastric tube is inserted through the nose to evacuate the contents and lavage the stomach in order to prevent aspiration pneumonia.
If the child’s hospitalization is late, on the 2-3rd day after birth, preoperative preparation lasts up to 12-24 hours in the absence of congenital midgut volvulus. In this case, due to the risk of intestinal necrosis, the duration of preoperative preparation is reduced to 3-4 hours. During the preoperative period, children are in an incubator at a temperature of 28-32°C, constantly receive oxygen, and infusion therapy is actively carried out (10% glucose solution , protein drugs) and anti-inflammatory therapy.
With low intestinal obstruction, preoperative preparation lasts 2-3 hours, which is due to severe complications that develop early (intestinal perforation, peritonitis), the purpose of preoperative preparation is to warm the child, administer cardiac drugs, vitamins, antibiotics, gastric lavage, in severe cases (with presence of intoxication and hyperthermia) - active infusion therapy.
Chronic and recurrent intestinal obstruction should be attempted to be operated on as planned. The degree and duration of preoperative preparation largely depend on the general condition of the patient and the degree of endogenous disorders.
Surgical intervention for congenital intestinal obstruction in newborns: a right-sided paramedian incision up to 9-10 cm long is performed. The nature of the intervention depends on the type of obstruction. In case of atresia and internal stenosis of the jejunum and ileum, resection of the atretic intestine is performed along with its expanded section (by 15-20 cm), since this segment is functionally defective. Sometimes the diameter of the afferent colon is reduced using intestinoplication, which preserves the absorptive surface of the mucous membrane. For the small intestine, end-to-end anastomosis is physiological. For better comparison of the ends of the intestinal loops, the Rehbeіn technique of wedge-shaped excision of the antimesenteric edge of the distal end of the intestine is used. A single-row screw-in suture is applied with atraumatic needles.
For atresia and internal stenosis of the duodenum, a longitudinal duodenotomy is performed 1 cm above the site of the obstruction. The septum is circularly excised until the mucous membrane passes to the intestinal wall. After determining the location of the major duodenal papilla, circular sutures are applied to the mucous membrane. The duodenal wound is sutured with a double-row suture (Fig. 3).
In recent years, an advantage has been given to end-to-end duodeno-duodenoanastomosis with wedge-shaped resection of the dilated wall. In the case of a wide ring of the pancreas, bifurcation of the pancreato-biliary duct, when the papilla fateri opens slightly in the upper part of the lower segment of the duodenum, duodenojejunostomy is used on a short loop “side to side” with single-row inverted sutures with PDS, Maxon 6/0 sutures (T.I. .Danshin, 2003). We must remember about technical errors: injury to the papilla of Vater, which requires plastic surgery of the papilla of Vater, and an unstitched window of the mesentery of the colon above the anastomotic suture line, where both afferent and efferent loops of the intestine can be infringed.
For Ladd syndrome, surgery consists of eliminating midgut volvulus by rotating the intestines around the mesentery clockwise and cutting the embryonic cords that compress the lumen of the duodenum. There is no need to try to restore the normal position of the cecum and its fixation in the right iliac region, since such manipulations complicate the operation and lead to relapse of intestinal obstruction (Fig. 4). T.I. Danshin et al (2003) form the duodenojejunal flexure by tucking the duodenum under the superior mesenteric artery and overlapping the lower horizontal branch of the 12th duodenum with the parietal peritoneum.
During operations for an annular pancreas (Fig. 5) and an aberrant vessel, a bypass retrocolic anastomosis between the duodenum and jejunum is indicated.
In case of meconium ileus, to eliminate intestinal obstruction, resection of the most dilated and meconium-filled area is performed using double ileostomy according to Mikulicz (Fig. 6) and Y-shaped anastomosis, followed by washing the intestinal lumen with pancreatic enzymes and retroperitoneal closure of the fistula.
| Rice. 3 Duodenotomy with excision of the membrane: a - excision of the membrane, b - suturing of the mucous membrane, c - preservation of the membrane at the level of the major duodenal papilla. |
Rice. 4. Ledd’s operation (scheme according to G. A. Bairov): a - straightening of the volvulus by turning the intestinal loops counterclockwise; b - intersection of the strands of peritoneum, which compress the duodenum; c - transfer of the colon to the left
Small 5. Duodenojejunostomy for annular pancreas (scheme according to G.A. Bairov)
Rice. 6. Double ileostomy according to Mikulicz (scheme according to G. A. Bairov)
In the postoperative period, parenteral nutrition is administered for 3-4 days. The stomach is constantly drained with a thin probe through the nasal passage. Oral feeding begins only after intestinal motility has been restored and bowel movements have appeared.
After surgery for intestinal obstruction, children are under clinical observation: an increase in body weight is determined over time; adjust feeding; They treat dysbiosis, enzyme deficiency and anemia.
In severe forms of small intestinal obstruction after large resection of the terminal part of the small intestine and the ileocecal valve, short bowel syndrome occurs. Enteral feeding leads to diarrhea, steatorrhea, dehydration and malnutrition. Long-term parenteral nutrition promotes the recovery of children. Metabolic disorders occur much less frequently. But the family of such a child must be provided with socio-psychological support.
Mortality during surgical treatment of newborns with intestinal malformations has gradually decreased to 10.6% in recent years (T.I. Danshin, 2003). Its main causes are: prematurity, pulmonary pathology, combined severe anomalies of other organs, heart failure, septic complications that worsen the course of the underlying disease.
Causes
Intestinal obstruction can occur for various reasons.
For ease of initial diagnosis, they are divided into groups:
- The list is large, it includes all diseases that provoke changes in the surface of the intestinal tube, resulting in internal obstruction.
It includes diseases such as:
- intestinal tuberculosis;
- tumor;
- Crohn's disease;
- ascariasis.
- Diseases of the second group can cause poor blood flow in the intestinal tissues.
This group includes, for example:
- intestinal volvulus;
- intestinal hernia (internal, external);
- the entry of one part of the intestine into another (intussusception).
- The third group includes diseases that cause disruption of the nerves in the intestinal tissues.
These include:
- stroke;
- injury;
- hyperocalea.
- The fourth group includes pathologies caused by external influences on the intestines, due to which it is compressed.
For example:
- cyst;
- tumor.
The list of causes of intestinal obstruction includes the 10 most common diseases:
- intestinal tumors;
- abdominal diseases;
- hypokalemia;
- stroke;
- surgical operations in the abdominal area;
- fecal and gallstones;
- the appearance of hernias (external, internal);
- non-standard intestinal development;
- mesenteric diseases;
- the formation of cysts in and near the intestines.
Symptoms of intestinal obstruction in adults
Intestinal obstruction (symptoms in adults proceed mainly according to one development pattern) has its own special symptoms.
Initially, the first main symptoms appear:
- pain occurs in the navel area;
- infrequent bowel movements and gas accumulation in the abdomen;
- nausea and vomiting.
Pain and heaviness in the abdomen - this symptom always accompanies a patient with intestinal obstruction in an adult
After a day without treatment, complications appear, the list is added with new symptoms:
- strong contraction of the intestines (peristalsis);
- bloating due to accumulated gases and feces in the intestines. The abdomen takes on a firmer shape, different from its previous appearance;
- strong rumbling and noise appears;
- dehydration appears;
- dry mouth.
If for any reason treatment was not started after the appearance of all symptoms, then after 3 days the patient’s condition worsens significantly:
- accumulated masses poison the body and cause intoxication;
- fever appears;
- a state of shock may occur.
It is important to remember that the sooner the doctor begins treatment, the greater the chance of a positive outcome. And also some symptoms differ in their expression from other diseases, so you can suspect the presence of intestinal obstruction as early as possible:
- The vomit becomes yellow in color with a distinct stool odor. This situation arises if obstruction is present in the small intestine.
- If the process of intestinal blockage occurs in the colon, then there is constant nausea, without vomiting. There is bubbling, fluid flowing and rumbling in the stomach.
- Diarrhea appears with bloody admixture. This happens infrequently and indicates the presence of bleeding inside the intestines.
Why does the intestine become obstructed?
Intestinal obstruction occurs when peristalsis stops. Peristalsis is wave-like contractions that help push food through the large intestine and small intestine.
Intestinal obstruction is caused by damage to the nerves that stimulate its function. This often happens after surgery under anesthesia, infection, blood flow problems, injury, medication, or changes in microflora.
Factors that increase the risk of intestinal obstruction include:
- abdominal or spinal surgery;
- intestinal damage or injury;
- abdominal bleeding;
- infections such as: peritonitis, appendicitis, kidney infection, and diverticulitis
- pneumonia;
- severe generalized infections such as sepsis;
- heart attack or stroke;
- imbalance of electrolytes, especially potassium and calcium;
- disorders that affect muscle function;
- use of certain medications, such as narcotic pain relievers, blood pressure medications, or chemotherapy;
- family history of obstruction, heredity
Symptoms of intestinal obstruction are easily diagnosed
And first of all this:
- bloating
- pain
- vomit
- convulsions
- hiccups
- inability to defecate or pass gas
Stages
| Stage | Characteristic | Symptoms | Stage duration |
| Initial (ileus cry) | Manifested by pronounced abdominal pain |
| Until 12 – 16 hours |
| Intoxication | Poor circulation and the appearance of severe intoxication in the body |
| Does not exceed 36 hours |
| Peritonitis | Associated with the process of severe inflammation and poisoning of the body. |
| From 36 hours onwards |
Signs of intestinal obstruction
An early and obligatory symptom of acute intestinal obstruction is abdominal pain. The pain can occur suddenly without any warning signs, be “cramping”, and usually it does not depend on food intake. At first, attacks of pain during acute intestinal obstruction are repeated at approximately equal intervals and are associated with the physiological wave-like movement of the intestine - peristalsis. After some time, abdominal pain may become constant.
With strangulation obstruction, the pain is immediately constant, with periods of intensification during a wave of peristalsis. In this case, the subsidence of pain should be regarded as an alarm signal, since it indicates the cessation of intestinal peristaltic activity and the occurrence of intestinal paresis (paralysis).
With paralytic intestinal obstruction, abdominal pain is often dull, bursting.
Symptoms vary depending on the height of the food obstruction - in the esophagus, stomach, duodenum or large intestine. Retention of stool, including its absence for several hours, and lack of passage of gases are early symptoms of low intestinal obstruction.
When mechanical compression, paresis or narrowing is located in the area of the upper intestines, mainly at the onset of the disease, with partial patency of the intestinal tube, under the influence of therapeutic measures, the patient may have a bowel movement due to bowel movement located below the obstacle. Nausea and vomiting are often observed sometimes repeated, indomitable, increasing with increasing intoxication.
Sometimes there is bloody discharge from the anus.
Upon careful examination, you can notice significant bloating and pronounced asymmetry of the abdomen, peristalsis of the intestines visible to the eye, which then gradually fades away - “noise at the beginning, silence at the end.”
General intoxication, weakness, loss of appetite, apathy - these symptoms are observed in most patients with gradual progression of intestinal obstruction from partial to complete.
First aid for intestinal obstruction
Intestinal obstruction in 60% of cases requires surgical intervention. Therefore, an adult should immediately seek help.
It is necessary to monitor the patient’s symptoms and also carry out the following manipulations:
- put the patient to bed;
- measure body temperature;
- track changes in heart rate;
- measure pressure;
- It is allowed to give some water in small portions.
Diagnosis of intestinal obstruction
Diagnosis begins with a physical examination and a review of the person's medical history. A doctor may use a stethoscope to check a person's bowel activity. Absence of bowel sounds or unusually quiet sounds may indicate a bowel obstruction. Depending on individual cases, your doctor may recommend tests, which may include:
- blood tests to check electrolyte levels, liver and kidney function, and blood counts;
- endoscopy, in which the doctor uses a special camera to look inside the intestines;
- radiography.
Doctors may use a substance called contrast, which is given through an enema. The contrast allows doctors to see the intestines more clearly when performing imaging tests.
Diagnostics
When a patient is admitted to the hospital with suspected obstruction, the initial examination and diagnosis is carried out by a surgeon. He decides whether it is an operational case or not.
To examine the patient, the following procedures are performed:
1. Collection of information about the patient (history).
2. Initial examination.
It includes a visual examination and examination of the abdomen:
- Feeling the abdomen with your fingers (palpation) - the doctor examines the abdomen and finds the exact location of the source of pain.
- Tapping on the abdomen (percussion) - thanks to tapping on the abdomen, the doctor determines the necessary information by sounds.
- Listening to the abdomen (auscultation) - noises in the patient’s abdomen are determined.
3. The patient's temperature, pressure, pulse are checked, and the oral cavity is examined.
4. After the procedures, the surgeon prescribes an x-ray examination using one or more methods:
- Radiography performed standing, without additional preparation. In severe cases, the procedure is performed lying on the left side.
- Schwartz test - half a glass of contrast liquid (100 ml) is drunk, after which an x-ray is taken. It shows in more detail where the blockage is in the intestines.
- Probe enterography - contrast fluid enters the duodenum thanks to a catheter placed.
5. Ultrasound examination. Allows you to view the condition of the abdominal cavity in real time.
6. Collection of blood for tests. The patient is examined for general and biochemical indicators; venous blood is required for examination.
Can intestinal obstruction be treated without surgery?
About 35 – 40% of cases are cured with medication. After examining the patient, bowel cleansing is prescribed.
This can be done in several ways, depending on where the problem is:
- If the source of the congestion is in the upper part of the intestine, then tubes are installed through the nose to the gastrointestinal tract.
- If the outbreak is in the lower part (large intestine), then an enema is given, with the help of which the intestinal contents are emptied using warm water introduced by a special probe.
These manipulations primarily help relieve the load on the intestines and remove the cause of its poisoning from the body. Next, drug treatment is introduced.
When a patient sees a doctor, treatment decisions are made quickly. If the chosen plan does not bring results within a few hours, then surgery is prescribed.
Acquired intestinal obstruction in children.
Intestinal obstruction
(from ileus-Latin, eileos - ancient Greek - to rotate) - stopping the passage of contents through the gastrointestinal tract.
OKN classifications:
According to the mechanism of occurrence:
1. Functional a) spastic, b) paralytic;
2. Mechanical: a) Strangulation, b) Obstruction, c) Mixed.
By level of obstruction:
1. Small intestine.
2. Colon
Stages of development of CI.
1 - the initial stage (“ileus cry” according to Kochneva O.S., 1984) or stage (“impaired intestinal passage” according to Eryukhin I.A., Petrov V.P., Khanevich M.D., 1999) is manifested by intense pain syndrome, which, depending on the form of obstruction, can last from 2 to 12 hours.
2 - intermediate stage (toxic or stage of acute disorders of intramural hemocirculation according to Eryukhin I.A., Petrov V.P., Khanevich M.D., 1999). It is based on disturbances of intramural hemocirculation and manifests itself as endotoxicosis. Lasts from 12 to 36 hours.
3 - late stage (peritonitis), occurs after 36 hours and is characterized by the extreme severity of clinical manifestations caused by associated peritonitis.
This division is very arbitrary, since the stage of CI largely determines the severity of the patient’s condition and the probable prognosis of the disease.
With dynamic obstruction, there is no mechanical obstacle to the movement of intestinal contents. It is difficult or does not occur at all due to impaired intestinal motility. Dynamic obstruction is divided into spastic and paralytic.
Functional (dynamic) intestinal obstruction
occurs as a result of a violation of the tone of the muscular lining of the intestine due to various reflex effects on the motor function of the intestine from organs located in the abdominal cavity or outside it, with pathological changes in the central nervous system, with disturbances in the water-electrolyte balance, acid-base state.
In spastic form
chyme does not move through the intestine due to intestinal spasm in one of its sections. It can be caused by: hepatic and renal colic; lead poisoning; porphyria; ascariasis, diseases of the central nervous system (for example, hysterical ileus). Currently, this form is very rare. In former times, it was, as a rule, a complication of ascariasis, which was very common among the child population. Under certain conditions, in particular after eating any food unpleasant for roundworms, they intensified their motor activity, curled into balls, to which the intestines responded with a long-term spasm in the area of this ball - spastic obstruction of the intestine developed, clinically resembling mechanical obstruction. It was usually resolved by conservative measures - the prescription of antispasmodics and cleansing enemas, after which many parasites were eliminated. Sometimes it was necessary to operate on children and remove tens and hundreds of roundworms by enterotomy.
Paralytic
obstruction in a surgical clinic occurs quite often. Reasons for the development of paralytic CI:
· diseases of the peritoneum and abdominal organs, blunt trauma to the abdomen;
diseases and injuries of the retroperitoneal and pelvic organs
diseases and injuries of the central nervous system
diseases of the lungs and cardiovascular system
intoxication and metabolic disorders: hypokalemia, hyponatremia,
· use of medications: ganglion blockers, anticholinergics
· uremia
diabetic ketoacidosis, diabetic neuropathy
lead poisoning
· porphyria
sepsis
The most common type of dynamic intestinal obstruction in a surgical clinic is postoperative intestinal paresis. There is an idea that spasm and intestinal paresis are components of a single process that transform into each other. Damage to peristalsis in such cases probably depends not so much on toxic damage to the muscular lining of the intestine, but on an increase in the tone of the sympathetic nervous system.
Treatment of paresis aims to break vicious circles by affecting all areas of pathogenesis. Treatment should be comprehensive (prozerin or its analogues alone are not enough, and in practice I often encounter this error when I consult children with intestinal paresis - they are usually invited to decide on the issue of excluding a surgical cause for this condition).
Complex treatment of paresis includes correction of:
Ø hypokalemia - drip administration of potassium chloride;
Ø hypovolemia and other disorders of salt metabolism - infusion therapy;
Ø hypoxia - prescribing oxygen therapy;
Ø reduction of intra-abdominal pressure - by introducing a permanent probe into the stomach and emptying the final sections of the colon with hypertensive enemas;
Ø improvement of microcirculation - by prescribing antispasmodics or prolonged epidural anesthesia.
Only against this background do peristalsis stimulants—prozerin and its analogues—have their effect.
Mechanical obstruction
is divided into two large groups: strangulation and obstruction.
To strangulation
obstructions include: volvulus, nodule formation, intestinal strangulation by adhesions and cords, or strangulation in the internal hernial orifice and pockets. Its distinctive feature is the presence of a violation of microcirculation in the intestinal wall as a result of strangulation or compression of the intestine together with the mesentery and its neurovascular trunks, which leads to a sharp disruption of blood circulation, up to intestinal gangrene.
Obstructive obstruction
may be caused by:
1. compression of the intestine by tumors of other organs, lymph node packages, inflammatory infiltrates;
2. bends of the intestine with adhesions and cords;
3. blockage of the intestinal lumen by tumors, gallstones, balls of roundworms, coprolites and enteroliths;
4. cicatricial stenosis due to ulcerative or inflammatory processes in the intestine.
In the etiology of intestinal obstruction, one should distinguish between predisposing factors that create the basis for its development and producing factors.
Predisposing factors include: anatomical and pathological changes in the abdominal cavity and directly in the intestine:
a) anomalies of intestinal development (duplications, diverticulitis, common mesentery of the small intestine and cecum, fissures and windows in the mesentery, etc.);
b) adhesions, cords, adhesions;
c) foreign bodies, scars and intestinal tumors;
d) excessive mobility of organs (long sigma, mesentery).
Producing factors include: increased intestinal motility caused by increased food load (large meals after fasting, etc.), enterocolitis, drug stimulation of peristalsis, a sudden increase in intra-abdominal pressure during physical stress.
Pathogenesis.
With acute intestinal obstruction, complex and diverse disturbances of the body’s activity occur:
1. Violation of mesenteric and organ hemocirculation, leading to ischemia and destructive changes in the intestinal wall, disruption of the intestinal barrier function.
2. Development of the syndrome of excessive colonization of the small intestine (increased concentration of bacterial flora, migration of microflora from distal to proximal sections, development of anaerobic microorganisms). A decrease in the barrier function of the epithelium leads to transepithelial migration of microorganisms and their toxins into the abdominal cavity and blood.
3. Violation of the motor and evacuation function of the intestine (hypertonicity of the sympathetic nervous system, hypoxic damage to the intramural nervous system, metabolic disorders in the muscle tissue of the intestinal wall, inhibition of the muscle activity of the intestinal wall by endotoxins of microorganisms, disruption of the secretion of serotonin and motilin by cells of the APUD system).
4. Violation of the secretory-resorptive function of the intestine (circulatory disorders cause hypoxia of the mucous membrane and cause degenerative processes in it).
5. Violations in the immune system, because The gastrointestinal tract is the most important organ that carries out the body’s anti-infective defense and is an essential component of the overall immune system.
6. Development of symbiont cavity digestion with the inclusion of enzymatic activity of microorganisms in this process, which leads to incomplete hydrolysis of protein products and the formation of biologically active polypeptides.
7. Endogenous intoxication due mainly to disruption of the barrier function of the intestinal wall. Initially, it is compensated by the detoxification function of the liver, but as the process progresses and the functional potential of the liver is depleted, microcirculatory disorders develop in other organs and tissues, and cellular metabolism is disrupted.
Mixed
forms of OKN have signs of both obstructive and strangulation varieties of ileus. A striking example of a mixed type of acute intussusception is intussusception, which is predominantly found in children. During intussusception, a section of the intestine, together with the mesentery, is embedded in the adjacent section of the intestine, and the intestinal lumen is obstructed by its own wall, and compression of the marginal vessels leads to acute ischemia of the invaginated intestine.
Adhesive
intestinal obstruction occupies a special place among other forms of ileus. Currently, this is the most common (in 78-86% of cases) type of acute intestinal obstruction. Abdominal adhesions can lead to the development of various types of acute intestinal tract. These forms differ in the mechanism of occurrence, clinical picture and surgical tactics for them. With the adhesive-dynamic form of OKN, effective conservative treatment is possible, while strangulation and obstructive forms will most likely require surgical intervention.
INTUSSUSCEPTION
Intussusception
- a common cause of intestinal obstruction in early childhood. This pathology was first described by Paul Barbette from Amsterdam in 1674. Jonathan Hutchinson performed the first successful operation on intussusception in a 2-year-old child in 1871. In 1876, Hirschsprung published a paper on the conservative treatment of intussusception by creating hydrostatic pressure. In the United States, Ravitch promoted the treatment of intussusception with a barium enema. His monograph, published in 1959 and covering all aspects of this problem, became a classic work on intussusception.
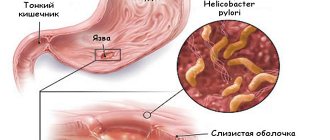
Pathogenesis. Intussusception is the penetration of one section of the intestine into another, usually proximal into distal, along the course of peristalsis. The mesentery of the proximal section also penetrates into the distal section and is compressed, resulting in venous obstruction and edema of the intestinal wall. In most cases, intussusception occurs at the ileocecal angle, starting directly at or near the ileocecal valve, with the distal ileum inserting into the proximal colon. Less commonly, ileo-ileal or colonic intussusception occurs.
It is difficult to detect specific features that would be characteristic specifically of ileocolic intussusception. After its elimination, a pronounced thickening of the wall of the distal ileum is usually observed. Although this thickening is partly due to secondary edema, there is a clear hypertrophy of lymphoid tissue in the intestinal wall. It has been suggested that the etiological factor of such hypertrophy may be adenovirus or rotavirus. The initial thickening of the intestinal wall sometimes plays a leading role in the development of intussusception. Mesenteric lymph nodes of the terminal ileum are also significantly enlarged after disinvagination. It is possible that this increase is not secondary, but primary.
Approximately 5% of patients, especially with ilioiliac intussusception, have some predisposing factor. The main one is Meckel's diverticulum. In addition, there may be polyps, intestinal duplications, lymphomas, submucosal hematomas (with Henoch's disease) and hemangiomas.
In older children, the cause of intussusception may be lymphosarcoma. With cystofibrosis, intussusception sometimes also occurs, which is facilitated by the presence of dense stool in the terminal ileum. The average age typical for intussusception in CF is 9 years.
Frequency. Intussusception usually occurs in the first year of life, mainly in children aged 5-10 months, with a clear predominance in boys. The incidence of this disease ranges from 1.5 to 4 cases per 1000 newborns.
Clinical manifestations. Intussusception in typical cases occurs in healthy, strong babies. The child suddenly begins to worry sharply, pulling his legs towards his stomach. After a few minutes the anxiety attack stops and the child again appears completely normal and quite active. Such attacks occur every 10-15 minutes and are pronounced. The child reaches out to his mother, climbs and presses against her chest, where he calms down somewhat until the next painful attack (s-m-monkey). Upon external examination of the child, he looks wary, even his sleep is superficial. At the beginning of anxiety, normal stool may be passed. Sometimes parents note the discharge of stool in the form of mucus of a slightly dark red color - “currant jelly”. In some cases, vomiting of undigested food occurs quite early. If the attacks continue, the vomit may become colored with bile. Some children become very lethargic and sleepy between attacks.
At the onset of the disease, the function of vital organs, according to examination, is usually not impaired. During an episode of pain, hyperperistaltic sounds are sometimes heard. A sausage-shaped formation may be detected in the abdomen. Rectal examination in some cases reveals the apex of the intussusception and blood-stained mucus. In rare cases, when examining the anus, prolapse of the intussusception can be seen.
If intestinal obstruction is prolonged, then dehydration and bacteremia develop, which leads to tachycardia and fever. Sometimes a vivid picture of hypovolemic shock occurs.
Diagnostics. X-rays in horizontal and vertical positions show low gas filling in the right lower quadrant of the abdomen or signs of intestinal obstruction - dilated intestinal loops with fluid levels. It should be noted that this picture is not specific to intussusception.
Some medical centers use ultrasound to diagnose intussusception. The sonographic appearance of intussusception was first described in 1977. Since then, many works have appeared describing such signs of intussusception as the “target” or “pseudo-bud” symptom. The “target” symptom is the presence on a cross section of two rings of low echogenicity, separated by a hyperechoic ring. The “pseudo-kidney” symptom is visible on a longitudinal section and consists of hypo- and hyperechoic layers layered on top of each other. This picture is due to the presence of edematous intestinal walls involved in intussusception.
If typical attacks of pain and stools in the form of currant jelly are observed, then you should immediately resort to irrigography, without wasting valuable time waiting for sonography data.
In most medical centers, barium irrigography is the main method for diagnosing intussusception. If this examination is carried out in compliance with all the rules, then complications are extremely rare. A sign of invagination is the presence of a spiral shadow.
Treatment. Once the diagnosis of intussusception is made, first of all, a nasogastric tube is inserted into the stomach for decompression and infusion therapy is started. If the diagnosis is completely clear and the duration of the disease exceeds 24 hours, then antibiotics are prescribed. They take blood for analysis (full) and group. If a child has vomiting and the disease has been for a long time, electrolytes are determined. Radiographs are taken in horizontal and vertical projections.
If the child's condition is stable and there are no signs of peritonitis, then a barium enema is performed, which has both diagnostic and therapeutic value. When trying to straighten the intussusception, sedation of the patient can provide significant assistance. A lubricated straight catheter or Foley catheter is inserted into the rectum and held in place by squeezing the buttocks and holding the baby in place. Barium is injected into the rectum from a height of 1 meter above the patient's level. Intestinal filling is observed using an image intensifier. Constant hydrostatic pressure is maintained until disinvagination occurs. If the outline of the barium remains unchanged (the barium “stands” in place and does not move further) for 10 minutes, the barium is released. The procedure can be repeated twice or three times. During attempts at hydrostatic straightening of the intussusception, you should not perform any manipulations (palpation) on the abdomen.
As a rule, straightening to the level of the ileocecal valve is quite easy, after which it is at this level that there is usually some delay in the penetration of barium into the distal part of the small intestine. Hydrostatic straightening of the intussusception is effective in 42-80% of cases.
Air can be used instead of barium to diagnose intussusception and expansion. Pneumatic spreading is widely used in China, with a reported success rate of 90% of cases. The procedure for introducing air into the rectum is controlled using an image intensifier. The maximum safe air pressure is 80 mmHg. Art. for small children and 110-120 mm Hg. Art. — for older patients. Air straightening requires less time than barium straightening. If pneumoperitoneum develops due to intestinal perforation, it is necessary to proceed to open laparotomy.
If complete expansion of the intussusception is achieved using a hydrostatic or pneumatic method, the child requires dynamic inpatient monitoring. Liquid food is prescribed. The patient can be discharged home after a few days if there are no complications.
Surgical treatment. Indications for surgical treatment:
1. Signs of peritonitis;
2. Age over 1 year;
3. Small-small intestinal intussusception;
4. Ineffectiveness of conservative techniques or complications during their implementation;
5. The period from the onset of the disease is more than 12 hours (in rare cases more than 24 hours);
6. Recurrence of intussusception.
After preoperative preparation, the operation begins.
Transverse incision in the right lower quadrant of the abdomen. Access allows you to easily remove intussusception into the wound. To reduce swelling, gentle pressure is applied to the intussusception. The invaginated intestine is “milked” into its normal position using delicate massaging movements. To avoid damage to the intestinal wall, the proximal and distal segments should never be pulled in different directions. If it is not possible to eliminate the intussusception manually or if after straightening there are signs of intestinal gangrene, resection and end-to-end anastomosis are indicated. If there is any doubt about the viability of the intestine after straightening the intussusception, the intestine is covered with warm napkins and re-examined after 10-20 minutes. In cases where organic causes of intussusception are discovered (tumors, Meckel's diverticulum, etc.), resection is performed. If there are changes in the appendix, then an appendectomy is performed.
Modern methods of disinvagination include:
· pneumatic or hydrostatic straightening of intussusception under ultrasound control;
· pneumatic or hydrostatic straightening of intussusception under videolaparoscopy control;
Laparoscopic disinvagination.
Forecast. The recurrence rate of intussusception ranges from 8 to 12%. Relapses occur mainly after hydrostatic expansion. The treatment of children with relapse should be approached on a purely individual basis. In older children, the first relapse requires surgical treatment, since in the older age group there is a higher incidence of small intestinal tumors as a cause of intussusception.
Treatment of intestinal obstruction at home
Only cases of partial obstruction are treated at home.
The treatment process is divided into several stages:
- If the obstruction is caused by a mechanical effect, then the patient, upon entering the hospital, undergoes a bowel cleansing procedure and drug treatment in the hospital, and at home is prescribed diet No. 4.
- If the cause is functional, with spasms in the intestines or partial paralysis: a number of medications are prescribed that can restore proper intestinal motility.
- In some cases, antiviral drugs are prescribed.
- In agreement with the doctor, a course of laxative medication is prescribed.
What is intestinal obstruction
This is a pathology that implies a complete or partial disruption of the release of food and liquid. The provoking factor is mechanical or functional reasons. The exact “culprit” determines the type of obstruction (mechanical, dynamic). The disease itself occurs in two forms - acute and chronic.
The disease has several types, such as:
- paralytic (relaxation of the intestinal walls);
- spastic (increased contractions and spasms).
The mechanical cause is divided into two subtypes: obstructive (compression of the walls), strangulation (compression of the intestinal walls with impaired vascular nutrition).
This condition is classified as severe because the mortality rate during the disease is 20%. In medical practice, surgeons note intestinal obstruction in only 3% of episodes.
Drugs
Drugs that help in the conservative treatment of intestinal obstruction:
1. Restoring the normal amount of fluid in the body:
- Methuselah.
- Quintasol.
2. Relieving spasms and cramping pain in the intestines:
- Drotaverine.
- Atropine.
- No-shpa.
3. To improve regional blood circulation:
- Rehydration.
- Reopoliglyukin.
- Pentoxifylline.
4. Replenishment of protein levels in the body:
- A mixture of amino acids.
- Albumen.
- Protein hydrolyzate.
5. Restoring intestinal motor function:
- Neostigmine.
- Distigmine bromide.
- Sorbitol.
6. Relieving intoxication of the body and reducing the risk of developing purulent-septic complications:
- Hemodez.
- Mannitol.
- Disol.
Intestinal obstruction - treatment
Treatment for intestinal obstruction depends on the cause and severity of the blockage. Complete mechanical obstruction usually requires surgical intervention.
Treatment methods for intestinal obstruction:
Drug treatment
. Opioids can cause constipation. If this happens, laxatives will help.
Observation
. The obstruction may need to be monitored for several days and often resolves with time. During this time it is necessary to limit food and drink. Doctors may give fluids intravenously to prevent dehydration.
Nasogastric tube.
This is a narrow tube that is inserted through the nose into the stomach. It removes liquid and gas trapped in the stomach, relieving pressure. This relieves pain and vomiting.
Operation
. Surgeons can remove blocked or damaged areas of intestine. In some cases, strictureplasty may be required, where the surgeon will widen the narrowed section of the intestine.
Therapeutic enema
. The nurse or doctor will administer medications or water into the intestines to induce bowel movements for severe constipation.
Use medications that can reduce discomfort:
- anti-nausea medications to prevent vomiting;
- painkillers;
- antibiotics to fight bacterial infection.
Diet
After the operation, the patient is excluded from eating and drinking for 12 hours. Afterwards, using a dropper, a nutrient solution is administered for 1 to 2 days.
After this time, if the patient is still unable to eat on his own, then an umbrella is inserted through the mouth for nutrition.
After removal of the foreign tubes, you are allowed to eat only fermented milk products and baby food from jars. If you have an obstruction, you need to eat in small portions, but often. Depending on the condition, light, unsalted, liquid foods are gradually added to the diet.
If the transition proceeds without complications, then the patient is prescribed a diet close to No. 4. It is designed to prevent food accumulation in the intestines. You need to steam, boil or bake without oil.
The diet is allowed to include:
- Meat broths are cooked low-fat and without salt.
- Grinded dishes.
- Porridge-like food, it is prepared with water and without salt.
- Meat is introduced into the diet in the form of cutlets and meatballs.
- Dairy products.
- Butter, but not more than 5 - 7 g per day.
- The omelette is light.
- Kissels and fruit jellies.
- Drinks – rosehip infusion, green tea.
All foods that can lead to the formation of problems in a new way are excluded from the diet:
- Flour products.
- Fatty food.
- Salting.
- Smoked products.
- Canned food (fish, meat and legumes).
- Raw vegetables.
- Heavy porridges (barley, barley, millet).
- Products with coarse fiber (cabbage, radishes).
- Drink: milk, coffee, sparkling water.
Intestinal obstruction (symptoms in adults and signs of its development are reduced if you follow the prescribed diet) can be cured. The diet is designed to reduce the load on the intestines, eliminate heavy foods and reduce the amount of their consumption.
Physical exercise
After the operation, physical exercises are introduced on day 2. To begin with, the set of exercises is designed for a lying position. When the patient sits down on his own, the exercises move to stage 2.
A set of exercises aimed at combating the occurrence of intestinal obstruction and postoperative recovery:
1. Lying position.
- Breath. A good breath is taken, and the exhalation is a little longer. Repeat 5 – 8 times.
- Coughing workout. Inhale through your nose, without opening your mouth, exhale with coughing movements. You need to lightly press down on the ribs with your hands.
- Warm up your arms. Extend your arms along your body. With each inhalation, raise your hand, and as you exhale, return it to the starting position. Do 5 times on each hand.
- Leg warm-up . Pull your toes towards you as much as possible, then away from you. The exercise is repeated 10 times.
- Sliding your heel along the bed, bend your leg at the knee. Repeat with each leg 4 times, then with both legs simultaneously do 3 times.
2. Sitting position.
- Bend your arms at the elbows, press your hands to your shoulders. In this position, the elbows rise to the side; do the exercise 6–8 times.
- Place your hands on the bed and move your legs, imitating walking, duration 2 – 3 minutes.
- Without lifting your heels from the bed, pull your toes towards you, then lower them away from you. The exercise is done 10 times.
After surgery, it is recommended to repeat the set of exercises about 6 times a day. The exercises are performed slowly so as not to harm the fresh seams. The duration of one complex is 6 – 8 minutes.
When the patient begins to get out of bed, the load is increased by walking. Initially, you can walk around the ward, then the corridor, then move on to walking along the street.
Folk remedies
The use of traditional methods should be discussed with your doctor.
The most popular remedies for intestinal obstruction:
- For 1 liter of water you need 0.5 kg of fresh plums. Having previously removed the seeds, they are filled with water and cooked on the stove for about 1 hour. You need to take the product 2 times a day, 100 ml.
- For 1 liter of hot water, take 1 kg of sea buckthorn. Pour water over the berries and stir until they are well saturated with water. Drain the liquid and squeeze the juice from the berries. Take the composition once a day, 100 g.
- Butter (20 g) is placed in half a glass of hot milk. Enemas are given from the resulting mixture.
- For 3 liters of boiling water, take 300 g of beets cut into slices. Pour water over the beets and leave for 3 hours. Then add 0.5 tsp. dry yeast, sugar (100 g) and mix. You need to infuse the prepared liquid for a day. Use half a glass of the composition every day.
- Dried apricots 40 pcs., 20 tbsp. l. raisins, 20 pcs. figs and 20 pcs. prunes. All ingredients are thoroughly washed with boiling water, then you need to grate them and mix thoroughly. Take 1 tbsp of the mixture in the morning before meals. l.
Intestinal obstruction (congenital)
Intestinal obstruction (congenital) is one of the most common causes of emergency surgery in children during the neonatal period. The development of congenital intestinal obstruction, as a rule, is based on anomalies in the development of the intestinal tube (duplication, atresia, Meckel's diverticulum, etc.).
There are many causes of the disease. These include malformations of the intestine, when the intestine is a cord, or looks like a bunch of sausages, or there are membranes in the lumen that interfere with the passage of food masses and feces, there may be an atypical position of the intestine in the abdominal cavity (volvulus), as well as anomalies of other abdominal organs cavities and kidneys.
Intestinal obstruction is divided into high, when the obstruction is in the initial part of the intestine, and low, when the lesion begins from the final part of the jejunum and below. In this case, the causes may be not only developmental defects, but also internal hernias - protrusions of the intestines through natural openings into various intra-abdominal pockets (the region of the cecum - the section of the intestine where the small intestine passes into the large intestine; the bursa of the omentum - the cavity in which the omentum is contained - a fold of the peritoneum, rich in blood vessels and adipose tissue and playing a protective role in diseases of the abdominal organs).
High intestinal obstruction manifests itself a few hours after birth, less often - at a later date (in the first days of life). The main symptom is persistent vomiting mixed with bile or greens. Children lose weight, dehydration and intoxication increase.
Urination is scanty. The abdomen is usually not distended and often appears sunken (scaphoid). Bloating, if observed, occurs after feeding and only in the area along the midline of the abdomen directly under the sternum (); after vomiting, the bloating disappears.
When probing the stomach, the amount of contents significantly exceeds the norm, as a rule, with admixtures of bile and intestinal juice, but impurities may be absent if the initial part of the duodenum is affected. With high intestinal obstruction, if the underlying parts of the intestine are not affected, meconium may pass during the first days.
Low intestinal obstruction also manifests itself in the first hours and days of life and is characterized by significant bloating and tension in the abdomen. You can often see by eye an increased movement of the dilated intestines over the obstacle. Vomiting is less frequent, but always of a stagnant nature, with a foul odor (). Meconium does not pass from the first days of life. The diseases are rapidly progressing, the condition is serious.
Recognition:
To clarify the diagnosis, find out the nature of the course of pregnancy (complications of pregnancy, polyhydramnios), assess the general condition of the child (the presence of intoxication, weight loss greater than physiological parameters, the presence and localization of abdominal bloating, movement of intestinal loops, tension in the abdominal muscles), perform stomach probing and analyze the amount of and the nature of the contents, the rectum is examined, as well as an x-ray examination.
Clinical picture of high intestinal obstruction.
The leading symptom is vomiting, which appears on the first day (usually even in the first hours) of life. Vomiting is profuse, with gastric contents (sometimes mixed with bile), infrequent (once every 3-4 hours). If, without suspecting intestinal obstruction, the child began to be fed, then vomiting is associated with feeding and occurs soon after it. The amount of vomit approximately corresponds to the amount of milk received during feeding, and sometimes exceeds the amount of feeding. Excessive vomiting can quite quickly lead to excisosis and the development of aspiration pneumonia.
Treatment:
At the slightest suspicion of intestinal obstruction, the child is urgently transferred to a surgical hospital, having first washed the stomach and left a permanent gastric tube to remove the contents.
The prognosis depends on the timeliness of the diagnosis and the surgery performed. With early treatment it is more favorable. The exception is children with multiple atresias, when the intestine is affected in several places over a large area.
How to treat intestinal obstruction at home
Since intestinal obstruction is one of the serious diseases, it cannot be treated at home. Any actions blur the picture and make it difficult to determine the correct diagnosis.
Actions that are not recommended to be done at home:
- Taking painkillers may make it difficult to pinpoint the source of pain.
- Take a laxative.
Inexperienced intervention may distort the exact causes of obstruction. If you suspect it, you must call an ambulance and go to the hospital for examination and determine a treatment regimen.
When is surgery necessary?
If the patient suffers from mechanical intestinal obstruction, then mandatory surgical intervention is required.
The main reasons for its appearance:
- tumors;
- volvulus;
- the appearance of a node in the intestines;
- adhesive disease;
- stones;
- ingrowth of one part of the intestine into another;
- strangulated hernia;
- foreign objects.
Surgical treatment of intestinal obstruction
The main objective of the operation is to eliminate the cause of obstruction, remove the main obstacle and reduce the risk of postoperative complications. The main actions of the surgeon begin with preparing him for the operation and undergoing the preoperative washing procedure.
Next in order:
1. The patient is given anesthesia with muscle relaxants.
2. An incision is made in the abdomen to provide full access to the intestinal area.
3. The entire intestine is examined, since in some cases the congestion occurs in more than one place.
4. If the operation is urgent and it was not possible to free the intestines in advance, this is done at the time of the operation using an incision in the intestine or through a feeding tube.
5. After freeing the intestine, the surgeon begins to eliminate the cause itself.
The procedure can be carried out in several ways, depending on the type of problem:
- An incision is made in the intestinal wall at the site of the obstruction, it is removed and the intestine is sutured. The procedure is possible if the obstacle is, for example, a foreign object or a gallstone.
- If the problem arises during the appearance of a strangulated hernia, the doctor reduces them.
- Part of the intestine is removed if a tumor has formed in it, or if this area of tissue is covered with necrosis.
- If after examination it turns out that it is not possible to remove the blockage in a simple way, the bypass anastomosis technique is used.
6. Checking the condition of the intestines. If the operation is performed correctly, the intestinal tissues are pink and all vessels allow blood to pass well. If any doubt arises, the error must be corrected immediately.
7. Colon lavage.
8. Final removal of purulent intestinal contents.
9. Stitching the incision.
Intestinal obstruction (symptoms in adults may reoccur after surgery) occurs due to poor diet or inactive lifestyle. To reduce the risk of recurrent obstruction, you must carefully follow your doctor's recommendations after surgery.
What needs to be done to save a person with intestinal obstruction?
The development of intestinal obstruction is an indication for urgent hospitalization in a surgical hospital, where the following is immediately performed:
- abdominal radiography,
- ultrasound examination of the abdominal organs
- irrigography is an x-ray examination with a contrast barium suspension introduced into the intestines using an enema.
In our clinic, we often use liquid contrast to better contour the bowel and to prevent barium from entering the peritoneal cavity during subsequent surgery. If the diagnosis is confirmed and/or severe clinical symptoms of peritonitis are present, emergency surgery is performed after very short preoperative preparation.
In the absence of symptoms of peritoneal irritation (peritonitis), conservative therapy is carried out for some time (up to a day) under the supervision of a surgeon:
- rehydration,
- administration of protein solutions, electrolytes,
- administration of antibiotics,
- release of the upper parts of the digestive tract by tube gastric lavage,
- intestinal lavage,
- pain relief, etc.
If there is no effect from conservative treatment, it is necessary to perform surgery as planned. If it is possible to remove the cause of obstruction, a diagnostic laparotomy with intestinal resection is performed. During the operation, an inspection of the abdominal cavity is required to clarify the cause of the development of acute intestinal obstruction and determine the total scope of the operation.
If adhesions, volvulus, loop nodes, or invaginations are detected during an audit of the abdominal organs, they are eliminated. If possible, cytoreductive surgery is performed to remove the primary tumor focus that caused the development of acute intestinal obstruction.
According to existing rules, removal of the intestine in case of obstruction should be carried out at a certain distance above and below the site of obstruction (obstruction). If the diameter of the connected segments is not significantly different, an “end to end” anastomosis is performed; if there is a significant difference in the diameters of the adducting and efferent sections of the anastomosis, a “side to side” anastomosis is performed. In our clinic, we use both classic hand-suturing techniques for the formation of anostoses, and modern stitching devices such as staplers.
In case of severe general condition of the patient or the impossibility of forming a primary anastomosis for other reasons, for example, due to an advanced tumor process, the formation of a “tumor shell”, a large extent of the section of resected intestine, accumulation of a large volume of fluid in the abdominal cavity (ascites), on the anterior abdominal A hole is formed in the wall - a colostomy, into which the adducting and efferent segments of the intestine are brought out - a “double-barrel stoma”.
Depending on the section of the intestine from which the colostomy is formed, this surgical intervention has a different name:
- ileostomy - when removing the small intestine,
- cecostoma - blind,
- ascendo-, descendo- and transversostomy - respectively, ascending, transverse and descending sections of the transverse colon,
- with sigmostomy - from the sigmoid colon.
During surgery on the sigmoid colon, called the “Hartmann operation,” the efferent segment of the colon is always sutured tightly and immersed in the abdominal cavity.
Postoperative period
Intestinal surgery is considered major, and the recovery process takes a long time. The patient is sent to the intensive care unit and is under constant monitoring.
A number of procedures must be carried out daily:
- The intestines are washed through the inserted probe, which remains after the operation. With its help, accumulated liquids and gases are removed. This reduces the risk of re-intoxication.
- Introducing fluids into the body to prevent dehydration.
- Feeding occurs through tubes.
- Droppers with antibacterial agents.
- Physiotherapy.
- Dressing the wound.
- Anesthesia.
If no complications arise, then after 4–5 days the patient is removed the tube and allowed to eat on his own. The diet includes only liquid food.
Complications
The outcome after surgery directly depends on the patient’s condition upon admission. If the patient is admitted in a serious condition with obvious intoxication of the body, the risk of death increases to 40%, this is due to extensive intoxication of all organs.
The remaining 60% are at high risk of developing postoperative complications, such as:
- peritonitis;
- wound suppuration;
- abscess.
And also in rare cases, it is possible for all operated patients to develop such complications as:
- bleeding;
- spread of adhesive disease;
- the appearance of fistulas;
- seam tears.
Intestinal obstruction is a serious disease, its symptoms should not be ignored. In 60-65% of cases, drug treatment has to be abandoned and urgent surgery is prescribed. If the first signs of illness appear in a child or adult, you must immediately call an ambulance.
Author: Irina Efanova
Article design: Mila Friedan