CAUSES OF ENTERITIS
The causes of acute and chronic enteritis differ. Acute occurs in a short time after the occurrence of the etiological factor, and in the case of chronic, pathogenic conditions have a long-term effect in the small intestine.
The following factors can lead to acute enteritis:
- acute bacterial or viral infection (cholera, salmonellosis, typhoid fever);
- poisoning with toxic substances;
- consumption of poisonous foods (berries, mushrooms, etc.);
- abuse of fatty, fried, spicy foods;
- allergies to food or medications.
Chronic enteritis develops due to:
- parasite infestation;
- long-term use of drugs that negatively affect the intestinal mucosa;
- bad eating habits: eating rough food, fatty, spicy foods;
- chronic poisoning with heavy metals and caustic substances.
In addition, the development of chronic enteritis is promoted by smoking, renal failure, a tendency to allergies, atherosclerosis, enzymopathies, autoimmune processes, and inflammation of the mesenteric vessels.
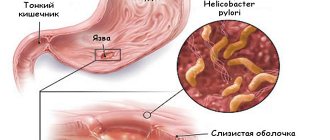
What is chronic enteritis
A disease called “Chronic enteritis” is an inflammatory process of a chronic nature, usually located in the small intestine. In the presence of the disease, damage to the mucous membrane occurs. There is progressive as well as recurrent enteritis. The disease is especially common in countries where hot climates prevail; it is less common in countries with temperate climates.
Classification
Chronic enteritis has a fairly broad classification:
- By etiology – primary and secondary.
- By localization - total and segmental (ileitis, duodenitis, jeunitis).
- According to morphological characteristics - without atrophy, with moderate atrophy and with severe atrophy.
- According to clinical signs - according to the severity of the course, according to the phases of the course, according to the nature of the disorders.
Severity
Chronic enteritis can occur in 3 degrees of disease severity:
- I degree. The disease occurs in a mild form; the main signs of the disease can be observed in the patient. At the same time, general well-being does not change much. The disease is diagnosed by conducting a scatological examination. Some patients lose slight weight.
- II degree. The disease is of moderate severity. There are pronounced signs of the disease on the face. Some symptoms are permanent. About 50% of patients lose about 10 kilograms of weight. With persistent and long-term treatment, you can achieve an improvement in your well-being.
- III degree. The disease is severe. Patients are underweight (weight loss exceeds 10 kilograms). Visible mucous membranes and skin are dry. There are signs of a- or hypovitaminosis. Signs indicating intoxication of the body increase (weakness, sweating, decreased appetite, tachycardia), the terminal phalanges on the fingers thicken, and the nail plates change shape. Some patients begin to suffer from osteoporosis, and signs of other diseases appear.
Patients are poorly able to tolerate viral or other bacterial diseases. Often, the deterioration of patients' condition is associated with alcohol consumption, poor diet, and sometimes physical activity.
CLASSIFICATION OF ENTERITIS
According to the location of the inflammatory process, enteritis can be divided into the following types:
- Duodenitis - an inflammatory process that forms in the duodenum;
- Jejunitis - inflammation affects the jejunum;
- Ileitis - the disease is localized in the ileal region of the small intestine.
Based on etiology, infectious and non-infectious enteritis are distinguished. Infectious, of course, is much more common. Food and water can be sources of pathogenic microbes. Bacteria enter the gastrointestinal tract due to non-compliance with basic hygiene standards.
According to the nature of the disease, acute and chronic forms are distinguished. Acute enteritis is dangerous due to severe dehydration of the body due to vomiting, diarrhea and profuse sweating.
Chronic nonspecific enteritis
Chronic enteritis is an inflammatory disease of the small intestine with disruption of its activity, which is expressed in premature digestion and absorption process, dystrophy, degenerative changes, as well as atrophy of the intestinal mucosa and disruption of the entire functionality of this organ.
Chronic enteritis in adults and children can be primary or secondary. The causes of the primary disease include:
- The medical history includes acute intestinal infection of a nonspecific type.
- Violation of the nutritional regime - abuse of spicy types of dishes, overeating, dry food, carbohydrate foods.
- Toxic effects on the surface of the intestinal mucosa caused by alcoholic beverages, medicinal chemicals, and contact with poisons.
- Allergic reactions.
- Ionizing radiation.
- Insufficiency of the ileocecal valve in the area where the small intestine meets the large intestine. This also includes the presence of a large duodenal nipple, ischemia of the intestinal wall, as well as anomalies of intestinal development, especially in children.
Secondary causes of chronic enteritis include:
- Presence of diseases of the digestive system.
- Diseases of the endocrine system, respiratory organs and blood circulation, as well as decreased immunity.
SYMPTOMS OF ENTERITIS
Acute enteritis is manifested by diarrhea, vomiting, loss of appetite, abdominal pain, fever, rumbling, and flatulence. Due to frequent watery stools and vomiting, a person develops a clinical picture of dehydration. The patient feels weakened, a white coating appears on the tongue, and dry skin is observed.
A sharp drop in blood pressure, tremors of the limbs, and tachycardia are possible. With chronic enteritis, extraintestinal manifestations are added: in particular, anemia due to impaired absorption of nutrients.
Restoration of normal microflora
If enteritis is a consequence of past infections or its exacerbations are associated with reinfection with intestinal infections and helminthic infestation, then in this case antibacterial/antiviral/anthelminthic agents are prescribed: erythromycin, chloramphenicol, and so on, depending on the cause of infection.
As a rule, almost all patients with chronic enteritis have dysbacteriosis . To eliminate this condition, the following is recommended:
- "Colibacterin";
- "Bifikola";
- "Bifidumbacterina";
- "Bactisuptila";
- "Lactobacterin";
- "Biosporina".
These drugs include “good” bacteria inherent in a healthy person; they help reduce the manifestations of dysbiosis and achieve remission of enteritis . Therapy with these drugs usually lasts up to 1.5 months.
Adsorbents, coating and astringents
These groups of drugs are mandatory for patients with enteritis and have severe diarrhea.
Astringents . The astringent effect of the drugs is realized due to their ability to precipitate proteins with the formation of albuminates, form a protective film and reduce inflammation.
Among these agents, the most effective are: calcium carbonate and basic bismuth nitrate.
Drugs with a sorbing effect are prescribed for severe exacerbation of the disease, which is accompanied by severe intoxication. The most popular among sorbents are: “ Enterodez”, “Polyphepan”, “Activated Carbon”, “Belasorb ”.
DIAGNOSIS OF ENTERITIS
Questioning and examining the patient will give the doctor the opportunity to make a preliminary diagnosis. But the final verdict can only be made after a series of studies:
- laboratory examination of stool - coprogram;
- functional tests (to detect carbohydrates and other substances in blood, urine and saliva);
- biochemical blood test (to identify signs of malabsorption syndrome - impaired absorption of nutrients);
- endoscopic examination with biopsy (allows us to identify atrophic phenomena in the mucous membrane of the small intestine);
- enterography is an X-ray examination with the introduction of contrast (detects changes in the folded structure, segmental lesions and tumor formations, ulcers).
Search results
VORONEZH STATE MEDICAL
ACADEMY NAMED AFTER
N.N. BURDENKO Department of Pediatric Infectious Diseases
Head department - prof. Kokareva S. A. Teacher – ass. Podshibyakina O.V.
Perelygin Denis Alekseevich.
Acute intestinal infection of rotavirus etiology, abortive form, mild enteritis. ARVI. Acute simple bronchitis, mild course.
Date of supervision: 10/06/2010 Curator: student L-501 group full name. Zimin Maxim Viktorovich
2010-2011 academic year Passport section
- Perelygin Denis Alekseevich, 2 years 4 months The child is disorganized, does not attend preschool institutions Date of admission to the hospital: 10/3/10 Diagnosis on admission: OKI of the type of acute enteritis. Clinical diagnosis: Acute intestinal infection of rotavirus etiology, abortive form, mild enteritis.
- ARVI. Acute simple bronchitis, mild course.
Anamnesis of life.
Born at 41 weeks. The first child in the family. Delivery through the birth canal. Labor is induced and fast. Body weight at birth was 3 kilograms 800 grams. Attached to the breast on the first day, she took the breast willingly. There were no signs of purulent ampholyte. When performing a culture from the oropharynx, group B Staphylococcus aureus was detected and specific treatment was carried out. Breastfeeding, later switched to mixed. Physical and mental development was within the age norm. Allergy history: food tolerance is good, previously received medications are well tolerated. The living conditions in the family are good, the family is mother, father. They live in a two-room apartment. The child’s parents and relatives did not suffer from tuberculosis or sexually transmitted diseases. Family history: maternal grandmother has type 2 diabetes mellitus.
History of the disease.
For up to a year, he suffered from intestinal rotavirus infection every 3 months. He was treated at the Liskinsky Central District Hospital. On average, I get ARVI once every 2 months. 08/07/09 – participant in an accident. TBI. Moderate brain contusion. Fracture of the occipital bone. Recovery without neurological consequences. See a neurologist.
Epidemiological anamnesis.
10 days before hospitalization, the child’s father was visiting his grandmother, who, according to the mother, “was poisoned”, after which three days later he suffered a short-term episode of ARVI (2 days of erased manifestations - mild nasal discharge without signs of malaise). The stool did not soften. Three days later (09.30.10) the child fell ill with ARVI. The mother shows no signs of infection.
Real illness
09/30/10 – cough, mucous discharge from the nose, difficulty in nasal breathing appeared. The body temperature increased to 37.5 o C. The appetite deteriorated, the child became less active. As a treatment, the mother used marispan, irs 19. By October 3, 2010, the body temperature decreased, mucous discharge from the nose decreased, and nasal breathing became free. The low-grade fever subsided, appetite improved, and activity returned. 3.10.10. from 9:00 in the morning frequent, liquid, watery, yellow stools appeared with a frequency of 1 time per 10 minutes. In total, I had bowel movements about 20 times during the day. No intoxication syndrome, nausea, or vomiting were observed. Gentamicin, interferrin, and furazolidone were used as self-medication. By 15:00, the parents sought medical help at OKB No. 2 of the Voronezh region due to persistent diarrhea. The patient was hospitalized in the department of intestinal infections.
Objective research.
At the time of supervision, the general condition is satisfactory. The child’s constitution is normosthenic, subcutaneous fat tissue is developed satisfactorily. Height - 87 cm, weight - 12 kilograms 700 grams. The skeletal system is without deformations, developed according to age. Peripheral lymph nodes are not palpable. The skin is clean, of normal color, skin turgor is preserved. Mucous membranes without pathology, pale pink color. The tongue is coated with a whitish coating. Hyperemia of the pharynx. The palatine tonsils are not enlarged. Breathing is puerile with a hard tint, rare dry wheezing is noted on exhalation. NPV - 28 per minute. The pulse is satisfactory, 118 per minute. Heart sounds are rhythmic and sonorous. Pathological noises are not heard. The abdomen is soft, elastic, moderately swollen, unpleasant sensations on palpation in the umbilical area. The stool is unformed, of normal color, mucous, 2-3 times a day. Peritoneal symptoms are negative. Free fluid in the abdominal cavity is not detected. The liver and spleen are not enlarged on percussion. The lower edge of the liver is 2 cm below the costal arch, which corresponds to the age and physiological norm. Sleep, restful, strong. Good appetite. Body temperature 36.8-36.9 Meningeal symptoms are negative. Diuresis is normal.
7.10.10.
The child's position is active, the general condition is satisfactory. Temperature – 36.8. The skin is clean. The tongue is moist and covered with a white coating. The abdomen is soft, palpable, painless, moderately swollen. The liver and spleen are not enlarged. The stool is unformed, of normal color, mucous. 3 times a day. The breathing is puerile with a hard tint, rare moist rales are heard, disappearing after coughing. NPV - 28 per minute. Heart sounds are sonorous, rhythmic, heart rate - 114 per minute. Diuresis is normal.
8.10.10
Moderate condition. The child's position is active. Temperature – 36.7. The skin is clean. The tongue is moist, covered with a white coating at the root. The abdomen is soft, palpable, painless. On auscultation, moderate peristaltic sounds are heard. The liver and spleen are not enlarged. Unformed stools, without pathological impurities, 2 times a day. small volume. Breathing is puerile, rare moist rales are heard, disappearing after coughing. NPV - 26 per minute. Heart sounds are sonorous, rhythmic, heart rate - 110 per minute. Diuresis is normal.
Laboratory data
General blood analysis.
Red blood cells 4.9x10 12 /l Hemoglobin 140 g/l Color index 0.90 Leukocytes 6.2x10 9 /l ESR 4 mm/h Eosinophils 2% Band neutrophils 2% Segmented neutrophils 55% Lymphocytes 37% Monocytes 4%
General urine analysis
Transparent, straw yellow color. Relative density – 1.025 Protein – 0.19. Epithelium – absent Leukocytes – units in the field of view Ketone bodies – absent Salts – oxalate – a little
Blood chemistry
Total bilirubin - 7.5 bound - 0 free - 7.5 Thymol test - 2.7 U AlAT - 17 U/l AST - 37 U/l Glucose - 4.9 mmol/l Amylase - 5.4 mg.
Scatological examination of stool
Color yellowish-brown Density not shaped. pH 7.0 Mucus moderate Leukocytes 3-5 in p/z. Red blood cells 0-1 in p/z. Epithelium - Starch - Intestinal fiber - Undigested fiber - Neutral fat - fatty acids + Yeast - No protozoa detected. No parasites were found.
Microbiological examination of stool
No pathogenic intestinal microflora was identified.
Analysis of stool for worm eggs
Result: not detected.
Rationale for diagnosis
Based on clinical manifestations (acute onset of the disease, repeated loose stools mixed with mucus, absence of intoxication and vomiting), data from laboratory research methods (scatological examination - disaccharidase deficiency, microbiological examination of feces for pathogenic microflora - not identified), data from the history of the present disease (onset diseases such as a respiratory infection, an illness in a grandmother like gastroenteritis), a clinical diagnosis can be made: Acute intestinal infection, rotavirus etiology, abortive form, mild enteritis. And also taking into account the presence of pathological processes in the respiratory system: ARVI. Acute simple bronchitis, mild course.
Differential diagnosis
Differential diagnosis is carried out with salmonellosis, yersiniosis, shigellosis. The development of these diseases is possible in children of this age group, in the presence of certain epidemiological conditions. It is necessary to differentiate this disease of the patient from salmonellosis. Common, in addition to the acute onset, intoxication syndrome, abdominal pain, vomiting, will be possible changes in the general blood test - leukocytosis, changes in the general scatological analysis. Salmonellosis, however, is characterized by febrile temperature, often of a wavy nature, and liquid, repeated stools of a dirty greenish, “swamp” color. The next disease in the differential diagnosis is shigellosis. Shigellosis is also often characterized by an acute onset, vomiting, intoxication syndrome, and headaches. Pain in the abdomen, however, is localized in the left iliac region and is cramping in nature, intensifying before the next bowel movement. The stool becomes more frequent, over time it loses its fecal character, an admixture of blood and mucus appears, and possible prolapse of the anus as a result of repeated false urges to defecate. On examination, a sharply painful sigmoid colon is characteristic, compacted on palpation; splashing noise and rumbling are detected during examination. There is a gradual increase in temperature. Vomiting is intermittent in mild forms, often once. What matters, as a rule, is the previously weakened general condition of the child. Intestinal yersiniosis is characterized by an acute onset and repeated vomiting. Pain syndrome in the abdomen. Typical for yersiniosis is the localization of pain in the umbilical region or in the right iliac region; peritoneal irritation syndromes, increased frequency of stools that are greenish in color, fetid odor, and mixed with mucus may be positive. In scatological analysis, signs of digestion disorders may be in excess of leukocytes and red blood cells. The main point in carrying out a differential diagnosis is the isolation of a specific pathogen during bacteriological examination or an increase in the titer of specific antibodies during serological reactions such as RA, RNGA, ELISA method with paired sera. etc.
TREATMENT OF ENTERITIS
Both acute enteritis and exacerbation of chronic enteritis are best treated in a hospital setting. There the patient is prescribed:
- dietary nutrition;
- drinking plenty of water;
- antidiarrheals;
- correction of intestinal microflora.
If infectious enteritis is suspected, antibacterial drugs should be included in the treatment regimen.
For patients with enteritis, diet table No. 4 is recommended. This is a gentle diet with the exception of milk, coarse fiber, fatty, smoked, and canned foods.
During remission of chronic enteritis, patients are prescribed:
- enzymes;
- adsorbents;
- pre- and probiotics.
Patients with enteritis - both during exacerbation and in remission - are recommended to take gastroenteroprotectors with rebamipide. These are drugs that restore the mucous membrane of the gastrointestinal tract. They reduce the level of inflammation, prevent pathogenic bacteria from attaching to the mucous membrane, improve blood circulation in it and stimulate the production of mucus.
Treatment
A gastroenterologist will help you get rid of chronic enteritis. Since the disease has a long and severe course, which is accompanied by frequent relapses, treatment will consist of a complex, including:
- diet therapy;
- medications;
- physiotherapy;
- traditional medicine recipes (strictly in consultation with your doctor).
Dietary ration
The goal of diet therapy is to launch tissue restoration processes in the small intestine, normalize its function and metabolism, eliminate fermentation and putrefaction in the digestive tract, and improve the general condition of a person.
The diet is selected taking into account the severity and other features of chronic enteritis. During the acute period, you should not eat food that irritates the mucous membranes.
The menu of a person who has been diagnosed with chronic enteritis consists of lean meats, poultry, and fish. Boil, bake, steam the meat. Allowed to use:
- chicken;
- turkey;
- young lamb;
- a rabbit.
To prepare soups, weak meat or fish broth is used. The best option is vegetable or mushroom broth. Vegetables must be well boiled, finely chopped or ground. Among dairy products, the consumption of kefir, yogurt, fresh low-fat cottage cheese and cottage cheese dishes is allowed.
Cooking porridges is allowed with low-fat milk or water. Do not use meat broth. The cereal should be well cooked. Millet and pearl barley are prohibited. Pasta is allowed in limited quantities.
Allowed use:
- zucchini;
- pumpkins;
- potatoes;
- carrots;
- beets;
- cauliflower and white cabbage.
The latter product is included in the diet if a person tolerates it well. Before use, vegetables are boiled, stewed, or steamed. They are also used for pudding, casseroles, and purees. You can add greens to vegetables. Finely chop it first.
Fruits and berries must be ground. You can use compote, jelly, jelly, mousse. It is preferable to bake apples. If a person tolerates citrus fruits well, two tangerines or one orange are allowed per day.
For chronic enteritis, a limited amount of marmalade, marshmallows, marshmallows, honey, and jam is allowed. Exclude flour products and white bread. No more than 2 times every 5-7 days, one non-hot cheesecake or a piece of pie with filling (meat, fish, egg, rice, apples, apple jam) is allowed. People with chronic enteritis should not abuse coffee, cocoa, or milk.
After the condition improves, the doctor may expand the diet. However, even during remission it is necessary to use with caution:
- any vegetables and fruits not included in the list of permitted ones;
- legumes;
- nuts;
- dairy products;
- spices;
- fried foods;
- bread;
- conservation.
It is required to limit as much as possible or completely eliminate carbonated drinks, fatty meat and fish, cold or hot dishes, alcohol, kvass.
Medications
Drug therapy involves the following goals:
- eliminate the pathological bacteria that caused the disease;
- normalize the microflora in the affected area of the intestine;
- correct disturbed water-electrolyte balance;
- eliminate symptoms;
- replenish the required amount of vitamins and microelements.
For chronic enteritis, the following is prescribed:
- antibacterial agents (if the bacterial etiology of the disease is proven);
- adsorbents;
- eubiotics (restore the physiological intestinal microflora);
- astringents;
- enveloping agents;
- vitamins;
- antispasmodics;
- probiotics;
- hormonal drugs;
- immunomodulators.
Physiotherapy
Physiotherapeutic treatment is prescribed in the absence of exacerbation of chronic enteritis. It includes:
- paraffin applications;
- ultraviolet irradiation;
- inductotherapy;
- acupuncture.
Thanks to such procedures, blood circulation improves, the functioning of the nervous system is stabilized, and intestinal function is activated.
ethnoscience
The use of traditional recipes is possible only after agreement with the attending physician. This treatment is not used as an independent method, but serves as an addition to drug therapy.
You can eliminate unpleasant symptoms and other problems with chronic enteritis using various infusions and decoctions.
- Mix one tablespoon of ground blueberry leaves, three tablespoons of chamomile, two tablespoons of cinquefoil root. Pour boiling water (0.7-1 l) over two tablespoons of the mixture. Cook over low heat for 15 minutes. Let it brew for an hour and a half. Take the resulting decoction 100 ml 2 times a day 20 minutes after meals.
- Pour one teaspoon of crushed calendula flowers into a glass of boiling water. Leave for an hour and a half. Take 3 times a day, 50 ml.
- Mix 2 tablespoons of crushed mint leaves, calendula flowers and chamomile. Pour one and a half tablespoons of the resulting mixture into two glasses of boiling water. Leave for an hour. Then strain. Take 150 ml 3 times a day before meals.
- Combine 200 g of honey with 50 ml of aloe juice, 100 ml of dry red wine. After thorough mixing, place in a dark place for 3-4 days. Take the resulting infusion once a day, 10 mg, half an hour before meals. Course duration – 3 days. Then the dosage is increased to one tablespoon and three doses per day.
PREVENTION OF ENTERITIS
To avoid enteritis, you should follow basic hygiene recommendations:
- Wash your hands properly - for at least 30 seconds;
- Do not drink tap water;
- Prepare food in clean dishes;
- Meat and fish products must undergo high-quality heat treatment;
- Fish and meat must be checked for freshness and washed with water before cooking;
- Be sure to store vegetables and meat separately - on different shelves of the refrigerator, in closed containers.
Also, the prevention of enteritis includes proper nutrition, timely treatment of diseases of the gastrointestinal tract, and taking medications only as prescribed by a doctor.
Prevention
Prevention of chronic enteritis should be aimed at reducing the risks of exacerbations. It includes :
- giving up alcohol and smoking;
- diet;
- timely treatment of all concomitant diseases;
- proper processing of food before eating it;
- compliance with personal hygiene rules;
- taking medications as prescribed by a doctor;
- excluding self-medication.
For patients with a history of chronic enteritis , sanatorium-resort treatment and regular examination by a gastroenterologist are recommended.