Is it possible to die from pancreatitis? To answer this question, many factors must be taken into account - the form of the disease, the degree of neglect of the pathology, the individual characteristics of the patient. Without treatment and neglecting the disease, you can bring the disease to a fatal conclusion.
Mortality from pancreatitis has increased in recent years, due to several factors that modern doctors warn their patients about. To prevent the negative consequences of the development of the disease, you need to know its signs and symptoms. At their first manifestations, you will be able to contact medical institutions, receive first aid and the necessary treatment.
What types of diseases are there?
There are two types of pathology - chronic and acute pancreatitis.
Chronic pancreatitis manifests itself due to the acute form of the disease. The disease progresses over the years, becoming more and more deformed.
In the acute form, inflammation of the organ occurs almost instantly. The form of the disease is rare. At risk are more often male patients aged forty to fifty years. Chronic alcoholism is often a risk factor for this pathology.
Cause of death
Can a patient die from pancreatitis? In recent years, deaths from such a diagnosis have occurred less frequently - there are more opportunities for treatment.
The prognosis of chronic pancreatitis largely depends on the stage of the disease. In the first stage, death from pancreatitis occurs less frequently. In the third stage, death is more common. If pancreatitis is not treated, the prognosis is likely to be fatal.
Causes of death in different forms of the disease
Mortality is determined by the origin, form, and symptoms of the pathology. Each form of the inflammatory process has its own causes of death:
- Alcoholic pancreatitis. This disease predominantly kills young and mature men, since this category of the population is most susceptible to alcoholism. With regular consumption of ethyl alcohol, toxic degeneration of liver and pancreas tissue occurs. Necrosis develops in the tissues, organs suddenly fail, and the drunken person dies. Death is possible even in a dream. Moreover, in men who give up alcohol, the damaged gland is not restored.
- Acute pancreatitis. This form of the disease is characterized by severe symptoms and has the highest mortality rate. If treatment is not started immediately, the sick person burns out in a few days, sometimes even in one day. It happens that patients die within a week even after starting therapy. In the acute form, internal bleeding and extensive necrosis lead to death.
- Chronic pancreatitis. This form, if it lasts for a long time, is no less dangerous than the acute form. During exacerbations, processes occur that lead to severe complications. Also, the cause of death in the chronic form is often malignant degeneration of glandular tissues. Due to the long-term inflammatory process, cancer is characterized by an aggressive course and quickly reaches the terminal stage.
- Hemorrhagic pancreatitis. An inflammatory reaction accompanied by internal bleeding is extremely dangerous. Bleeding occurs due to ruptures of the vascular walls under the aggressive influence of pancreatic enzymes. The patient requires urgent surgical intervention; otherwise, due to excessive blood loss, hemorrhagic shock develops and death occurs.
- Pancreatic necrosis. The death of glandular tissues is caused by various reasons. In most cases, necrosis is observed in acute and alcoholic forms of the disease. In an inflamed and swollen gland, the lumen of the ducts decreases, which is why aggressive pancreatic juice cannot escape and begins to destroy tissue.
- Postoperative complications. In case of complications and necrotic changes, emergency surgery is performed. But even after a successful operation, death is possible due to bleeding, postoperative peritonitis, reactive pancreatitis, and infectious damage to the organ. If the patient has diabetes, then after the surgical procedure a hyperglycemic coma may occur due to improper insulin therapy or non-compliance with medical recommendations.
Symptoms of the disease
Death from acute pancreatitis occurs if the disease is advanced; suppuration occurs at the site of inflammation, which breaks through and infects the blood. At this stage, the consequences of the disease are irreversible. According to statistics, death occurs in 40% of cases.
Among the symptoms of acute pancreatitis, you need to pay close attention to the following: severe girdling pain in the navel area, extending to the hypochondrium, back, shoulder girdle; nausea, severe vomiting that does not bring relief; pallor and cyanosis of the skin; dry mouth, unpleasant aftertaste. Many patients are sure that death from pancreatitis is possible only with a strong increase in body temperature, but practice shows that in some cases the temperature, on the contrary, even drops.
Severe weakness, dizziness, temperature below 36.5 degrees, this is a reason to immediately consult a doctor. A white coating appears on the tongue, the patient is constantly thirsty, he is tormented by dry mouth, his lips are also dry and cracked, but after drinking water, vomiting immediately occurs, dehydration occurs, which is also one of the reasons that the person died from acute pancreatitis .
What is pancreatitis?
The pancreas is one of the most important organs, without the normal functioning of which natural human life is impossible. Its main functions are the production of certain hormones (for example, insulin, glucagon, somatostatin), as well as enzymes necessary for the breakdown of food.
Abuse of alcohol, unhealthy foods, and overeating become prerequisites for the development of an inflammatory process in the organ. As a result of this, the pancreas swells greatly, and its pancreatic juice loses the ability to be freely transported to the duodenum to begin work on digesting the food bolus. Lingering in the pancreas for a long time, fermentation is activated and begins to digest the pancreas itself, that is, the process of self-digestion is launched, which causes serious disruptions in the body and severe symptoms in the patient. There is a disruption in the digestive process and absorption of nutrients, in addition, general intoxication occurs, which negatively affects a person’s well-being.
It is these phenomena that characterize a disease such as pancreatitis. In medicine, this term is usually understood as the inflammatory process of the pancreas, in which the organ is destroyed under the influence of its own enzymes.
In addition to neglecting the principles of healthy eating, other circumstances can lead to such a development of events:
- Various pathologies of the gallbladder, biliary tract or liver;
- Gastritis, ulcerative lesions of the stomach or small intestine;
- Mechanical damage to the abdominal organs due to surgical operations or injuries;
- Diseases of infectious or viral etiology: mycoplasmosis, hepatitis, mumps, purulent-inflammatory processes, chronic tonsillitis, chronic liver failure, intestinal sepsis, chicken pox, dysentery;
- Unjustified or long-term use of certain medications: estrogens, glucocorticosteroids, antibiotics, diuretics;
- Diabetes mellitus and atherosclerosis;
- Poisoning by toxic household or industrial substances (acids or alkalis), chemical intoxication, helminthic infestations;
- Obesity;
- Congenital pathologies, in particular, narrowing of the ducts;
- The period of pregnancy, during which the uterus exerts significant pressure on the vessels, which may well provoke the development of inflammation of the pancreas;
- Imbalance of hormones, as well as any endocrine pathologies;
- Genetic predisposition, in which pancreatitis can occur even in infants;
- Malignant tumors.
You can guess that the pancreas is out of order by symptoms such as nausea, vomiting, flatulence and diarrhea. But the most important symptom is acute girdling pain in the abdominal area, which is most often localized in the left hypochondrium. In the most severe and advanced cases, the pain is so strong and unbearable that the patient has to be administered narcotic drugs. However, this is not why the diagnosis of pancreatitis is scary - the main danger is that the disease can be fatal.
Causes of death
We can safely say that the cause of death from inflammation of the pancreas is the carelessness of patients. They are forced to die from related problems arising from significant disruption of the functioning of all organs and systems. Some people develop pain shock, while others develop an abscess. Often in older people, the heart simply cannot cope with increasing loads. No one can predict how the disease will behave, but in a hospital setting under the strict supervision of highly qualified doctors, the patient has a much better chance of a quick full recovery and a long life.
If a patient is in critical condition, the main task of doctors is to stabilize him and remove him from the risk zone. This is achieved in different ways in intensive care conditions. At this time, minutes count, so you can’t hesitate. In order not to waste time, the fight against the main ailment begins there. doctors are doing everything possible to reduce inflammation of the pancreas and relieve the patient of pain. If they succeed, the patient is transferred to the gastroenterology department, where the further struggle for health continues.
To never get into this state, you need to listen to your body. Periodically occurring pain in the navel area should alert you. Even if it goes away over time and does not cause significant inconvenience, it is better to make a preventive visit to a specialist and undergo a full examination of the body. When a disease is detected at an early stage, it is much easier to deal with its manifestations and root causes, and the likelihood of death is minimized.
Symptoms of pancreatitis
Such depressing statistics should make people more attentive to their health. Therefore, you should pay close attention to the following symptoms, and if they appear, see a doctor immediately.
- Attacks of acute pain occur in the area of the ribs and lower abdomen;
- There is constant nausea and vomiting that does not bring relief;
- With prolonged inflammation of the pancreas, the patient experiences increased body temperature;
- The skin becomes pale; in rare cases, the skin may turn yellow;
- The appearance of belching, frequent hiccups;
- There is an unpleasant taste in the mouth, the mucous membrane constantly dries out;
- There is a decrease in blood pressure.
Is it possible to die from chronic pancreatitis?
Chronic pancreatitis is not so acute and noticeable, but it is more difficult to get rid of. A sharp deterioration in the patient's condition is observed if he does not adhere to nutritional rules. For any problems with the gastrointestinal tract, diet is the main tool for successful recovery. Often restrictions on the foods consumed are imposed for life. It is difficult for patients to put up with this; they allow themselves small weaknesses, not even imagining that some of them can lead to a sharp deterioration in their condition, even death.
Pancreatitis is often a consequence of gallstone disease. In this case, you need to get rid of the root cause of the disease. Stones are removed mechanically; doctors often resort to urgent or planned surgery to completely remove the gallbladder. Operations are not performed when the patient is in acute condition.
Sometimes chronic inflammation of the pancreas develops into cancer of this organ. The relationship between these two diseases has not been proven by science, but world-famous oncologists note that malignant neoplasms more often occur in patients who previously often suffered from inflammatory processes. If oncology is detected at stages 3-4, then the destructive processes in the body are already irreversible, death is a natural result of the disease.
The work of doctors during this period is aimed at prolonging the patient’s life, palliative treatment is carried out. Patients have the power to prevent a severe course of the disease; they only need to monitor their current state of health, do not forget about regular preventive examinations and timely visits to the doctor.
Is it possible to die from pancreatitis?
Doctors never tire of telling patients that acute pancreatitis is fatal. Death occurs within the first week if treatment measures are not taken in time. People who ignore warning signs die. Cholangiogenic (in the presence of stones in the bile ducts) and alcoholic forms of pancreatitis often lead to death.
Pancreatic juice from the pancreas enters the intestinal tract and is diluted with other substances. But if this does not happen due to clogged ducts, the secretion corrodes the tissue. Mutation of cells in an organ and changes in their structure are no less dangerous.
The development of acute pancreatitis, which leads to death in half of the cases, can be considered using the following example:
- The patient regularly drinks alcohol, eats fatty, spicy and salty foods, smokes and feels quite tolerable for a certain time. But colic begins in the stomach, a feeling of bitterness appears in the mouth, and I constantly feel sick.
- The symptoms disappear after a few days, and the events again unfold in the same circle: alcohol, junk food, cigarettes. The patient does not realize that the pancreas is giving an SOS signal, and it is not too late to change the situation for the better.
- Since no steps are taken, the destructive processes in the organ continue until an attack of pancreatitis makes one involuntarily think about the consequences of an unhealthy lifestyle.
If doctors are able to provide assistance in a timely manner, there is still a chance of avoiding death, but this does not always happen.
Alcoholic pancreatitis
Alcoholic pancreatitis develops due to alcohol abuse. The type and cost of alcohol does not affect the course of the disease. You can get sick from both beer and expensive cognac if you drink regularly.
In chronic pancreatitis, mortality has been recorded for twenty years. During this period, half of the population suffering from pancreatic disease dies. Moreover, people of mature and young age have to die. The causes of death are not the disease, but the diseases that appear due to alcohol abuse.
The effect of alcohol on the pancreas
As a result of alcohol entering the body, pancreatic cells are deformed. The cause is substances formed during the breakdown of ethyl alcohol or surrogates.
Pathogenesis
Cell deformation occurs through the activation of enzymes produced directly by the gland. Then the enzymes act on the organ itself. The result is necrosis, the death of large areas. The gland becomes inflamed and increases to pathological sizes. The pancreatic tissue is deformed and replaced by fat cells, destroying the endocrine system. Diabetes develops due to pathology.
Alcohol, which is abused by diagnosed patients, has an extremely negative effect on cells. Tobacco, which often accompanies alcohol, causes vascular spasms, which increases tissue damage. Foods filled with fats activate secretory activity, causing a harmful effect on the gland.
The functions associated with the functioning of the pancreas are interconnected. It is impossible to say that the patient died from pancreatitis without finding out the true cause of death.
Classification of pancreatitis caused by alcoholism
The pathology is divided into two stages - acute and chronic. As a result of one-time consumption of alcohol in large doses, intoxication of the body occurs. This happens in the acute form of the disease. Signs of the acute form of the disease are similar to those of a conventional diagnosis.
The causes of chronic pancreatitis are mostly due to alcohol abuse. Symptoms of this type of disease may not appear for a long time. If you drink alcohol in small doses but regularly, the disease progresses daily. With chronic pancreatitis, patients live without realizing the presence of the disease for many years.
How dangerous is alcoholic pancreatitis?
During attacks of pain, many patients complain of acute pain in the upper abdomen, arising in the back and hypochondrium. Painful sensations intensify in the “lying on your back” position.
Due to impaired absorption of nutrients into the body, patients experience a sharp weight loss. To avoid death, you need to consult a gastroenterologist.
What are the complications of the disease?
Complications that arise lead to the formation of cysts and abscesses. With pancreatitis, if the disease is not treated, adenocarcinoma, pancreatic cancer, develops. The result of the pathology is often fatal.
Is it possible to cure pancreatitis caused by alcohol?
Treatment of the disease occurs under the strict supervision of a number of doctors. Professionals in the field of gastroenterology, endocrinology, and surgery are considered competent. In severe cases, ask for help from a radiologist or psychotherapist.
The main condition for effective treatment is the exclusion of alcoholic beverages from the diet. You cannot drink beer or other low-alcohol drinks.
What can cause acute hemorrhagic pancreatitis?
This pathology is characterized by the death of pancreatic tissue. As a rule, with this type of disease, the mortality rate among patients is high. The cause of the disease is surgical interventions, various wounds and injuries, and alcoholism. With pathology, a sharp enlargement of the gland occurs, resulting in hemorrhage and the formation of blood clots.
If acute hemorrhagic pancreatitis is suspected, patients feel chills and the temperature rises. Vomiting and weakness in the body appear. Pain sensations radiate to the shoulder blades and back. Sometimes the pain reaches the heart area. As a result of pressure on the front of the abdomen, acute pain occurs. Most patients with this type of disease are in serious condition. If treatment is not provided in a timely manner, the patient runs the risk of dying.
Pancreatitis is a disease whose course can be controlled. If you follow doctors' recommendations, there is no risk of death. Among other things, you need to monitor your emotional state, follow healthy eating rules, avoid stressful situations and undergo scheduled examinations on time. It is possible to live with such a diagnosis if the patient has a desire to live.
Dangerous symptoms, when to call an ambulance
Death from pancreatitis is considered a real danger when a person does not notice the symptoms of the pathology. The symptoms are similar to those of other diseases of the stomach and intestines, so it is important to distinguish between them and diagnose them in a timely manner.
The initial and main manifestations of acute and chronic pancreatitis are:
- vomit;
- nausea;
- girdling pain in the abdominal area that occurs immediately. After a person eats.
In chronic pancreatitis, the symptoms do not develop so rapidly, but the duration of the pain is much longer, relative to the acute course. With pancreatic necrosis, pain that initially occurs in the peritoneum area then moves to the lower chest.
Most often, pancreatitis is accompanied by outbreaks of pain, the development of which is characteristic of the acute form of the pathology, the outcome of which is impossible to foresee.
Main signs of pancreatitis
Vomiting, nausea and girdle pain in the upper abdomen that appear immediately after eating are the first and main symptoms of chronic and acute pancreatitis. Moreover, even severe vomiting does not bring the patient the slightest relief.
In the chronic form of pancreatitis, the symptoms do not appear so sharply, but the painful processes last much longer than in the acute form. Pain that initially occurs in the abdomen further spreads to the lower chest.
Pancreatitis is often accompanied by paroxysmal pain, the occurrence of which is characteristic of the acute form of the disease, the outcome of which can never be predicted.
First aid
If the above symptoms appear, you should immediately call an ambulance. In acute pancreatitis, death occurs from collapse (a sharp drop in blood pressure and disruption of the blood supply to all organs) and painful shock. While the doctors are traveling, it is necessary to take measures to alleviate the condition of the sick person: put the patient on his side; give him an antispasmodic drug; do not give anything to eat; press an ice pack to your body in the area of the pancreas.
Thus, first aid consists of observing 3 rules: cold, hunger and rest. The patient is hospitalized. Emergency diagnostics are carried out, during which the optimal treatment option is prescribed. In case of extensive destructive processes in tissues, the only therapeutic method used is surgical intervention. After the operation, treatment is carried out with enzyme preparations and vitamins.
The patient is on a strict therapeutic diet. To recover, you need to give up bad habits, lose excess weight, and do not forget about physical activity. Movement is life. The patient must remember this constantly after discharge from the hospital. Bringing your weight back to normal and increasing physical activity to the best of your ability are the top priorities on the path to recovery.
Signs of severe forms of the disease
- Of the main types of the disease, the acute phase of pancreatitis is distinguished; it is considered a dangerous form in which the death of the patient occurs.
- With unbearable pain in the abdomen of different locations - near the navel, under the rib on the left side or on the right. Often the pain is girdling, radiating to the lumbar area, both shoulders, and sternum. The pain syndrome can be so severe that it provokes the development of pain shock with a change in consciousness, the formation of multiple organ dysfunction, which leads to death;
- Dyspeptic manifestations are characterized by nausea and vomiting that does not bring relief, increased formation of gases in the intestines, bloating, and diarrhea. A severe form of dyspepsia with prolonged profuse vomiting and diarrhea leads to dehydration of the body, and essential microelements and vitamins are lost. This often develops as a result of insufficient or untimely infusion treatment. Dehydration of body tissues and lack of minerals negatively affect the functioning of all organs and systems; in serious cases, this can lead to death;
- General intoxication syndrome is manifested by various severe symptoms that indicate damage to all body systems. The main manifestations of poisoning of the body are increased temperature, a weakened body, pressure decreases to the point of collapse, shortness of breath, skin changes - pallor, jaundice, icterus, headache and dizziness, impaired consciousness;
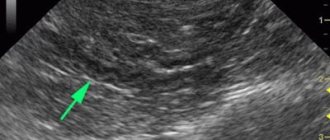
- Laboratory and instrumental tests worsen if there is severe inflammation of the pancreas. The CBC reveals obvious leukocytosis with a painful disorder of the leukocyte formula, a rapid increase in ESR due to inflammation. When the liver is affected or internal blood flow rapidly increases, the level of liver enzymes, amylase and other indicators that indicate damage to the organ increases. Ultrasound and computed tomography reveal symptoms of swelling, disorder of pancreatic tissue, abscesses and other painful disorders.
The onset of severe pain before the ambulance arrives cannot be dealt with using strong medications. It is also impossible to lower the increased temperature; vomiting occurs after eating. When the canals become clogged, many foci, purulent formations, and clots of coagulated skin are observed in the parenchyma. As a result of severe development of pancreatitis, both the pancreas fails and the functionality of the liver, kidneys, stomach, and intestines changes.
The cholangiogenic type develops immediately after eating food. This pathology is caused by the presence of excrement in the bile ducts. The course of the chronic alcoholic type of pancreatitis is often detected when the patient abuses alcohol too much.
Symptoms of this type appear quite clearly and occur if you eat fresh fruits, vegetables, or spicy or sour foods.
Early manifestations of the pathology are accompanied by endless constipation along with hypomotor dyskinesia of the colon and bile excretion passages. Constipation is often replaced by diarrhea. Diarrhea with this type is an invariable phenomenon and a typical symptom.
Death from pancreatic necrosis occurs in 1/3 of patients - these numbers are terrifying. Death with toxic pancreatitis of the gland is observed in 100% of cases.
The patient's death occurs within 7 days if treatment is not prescribed immediately. Patients who do not pay attention to emerging signs die. Often occurs as a result of cholangiogenic and alcoholic type of disease.
Let us look at the appearance of the acute form, which leads to 50% of deaths, using an example.
The patient constantly drinks alcohol and fatty foods, spicy and salty foods. He also smokes cigarettes, feeling normal for some time. However, colic occurs, bitterness in the mouth, and nausea is present all the time.
Signs of the disease go away after a certain period of time, and the person again drinks alcohol and smokes. Not understanding that the gland is signaling a problem, that it is not too late to change everything for the better.
Since no action is taken, the destruction of the pancreas continues until outbreaks of pathology force one to think about leading an unhealthy lifestyle.
It is important not to waste time if an acute course is suspected, so that the death of gland cells and the subsequent death of the patient from pancreatic necrosis does not occur.
Signs of acute pancreatitis
The main symptom that is always present with this diagnosis is severe and persistent pain, which is very difficult to relieve with analgesics. Often a painful attack is preceded by eating a large meal or drinking a lot of alcohol.
The following manifestations are also observed:
- severe nausea and vomiting that does not bring relief;
- bloating;
- dehydration;
- skin spots around the navel, which may have a bluish or yellowish tint.
- increased body temperature;
- chills.
People during an attack are restless, have rapid breathing and a rapid pulse. A decrease in blood pressure may occur. In purulent forms of the disease, severe intoxication occurs, which is accompanied by high fever, chills, and perspiration.
Such symptoms require immediate hospitalization and medical attention. The patient will not be able to make the patient feel better on his own. If you miss time, death is possible.
Causes of high mortality from pancreatitis
Can a patient die from pancreatitis? Recently, death from such a diagnosis has been observed less and less often, since more opportunities have opened up for the treatment of pancreatitis.
The outcome of exacerbation of the chronic form often depends on the degree of the disease. Death at stage 1 is rare. Often death comes to patients at stage 3 of the disease. If pathologies are not treated, death from pancreatitis is guaranteed.
These deadly pathologies are:
Alcohol-type pancreatitis - death with this type of disease most often occurs at a young age, especially men who are addicted to alcohol. If you regularly take ethanol, it will lead to toxic damage to liver and gland cells. With this form of pancreatitis, necrosis of the pancreas is observed and its functions are disrupted.
Death from the acute form with severe manifestations of symptoms is the highest. In patients, death occurs within the first 7 days from the onset of the disease, which happens even if therapy is started on time. The patient's death occurs due to exudate, massive necrosis of the pancreas, and internal bleeding.
Pancreatic necrosis is a pathology formed due to acute destructive pancreatitis, which appears as a result of drinking alcohol and eating harmful foods. As a result of inflammation, swelling of the pancreas or the presence of excrement in the excretory canals, their space narrows, and digestive juice, which is an aggressor for various tissues, is retained in the middle of the pancreas. Proteolytic enzymes cause disorder of the gland and organs that are adjacent to it.
When ulcers, fistulas, and ulcers form, the only solution to the problem is surgery.
Surgical therapy is carried out using several methods. The extent of surgical intervention will be determined by the degree of damage to the organ - necrotic tissue is excised, either one section, or rarely the entire organ.
Even if the operation was successful, the patient’s death may occur:
- in case of postoperative bleeding;
- reactive pancreatitis after surgery;
- infectious complications of the course, peritonitis;
- the presence of diabetes, complications, if replacement therapy is chosen incorrectly, or the doctor’s recommendations are not followed.
Death is often recorded in those patients who wait, hoping that the signs of pancreatitis will go away on their own.
Main causes of death from pancreatitis
Mortality due to inflammation of the gland depends on its type (etiology, pathogenesis, symptoms of the inflammatory process).
Alcoholic pancreatitis
Among those who died from alcoholic pancreatitis, many were young; this diagnosis was especially often given to men, since they are the ones who most often suffer from alcoholism.
Regular consumption of ethanol leads to toxic damage to the cells of parenchymal organs - liver, pancreas.
Alcoholic pancreatitis is characterized by the development of necrosis of the pancreas and disruption of its functions.
Acute pancreatitis
The statistics of death from acute pancreatitis with severe symptoms is considered the highest. Death occurs within the first week from the onset of the disease, sometimes even with timely initiation of therapy. The main conditions in which a patient dies due to acute pancreatitis are considered to be massive necrosis of the pancreas and internal bleeding.
Chronic pancreatitis
A long-term chronic inflammatory process in the pancreas is considered not as dangerous as an acute one. But, due to the inevitable damage to the organ during exacerbations, it is impossible to completely exclude the development of severe complications. In addition to death, during an exacerbation of the disease, death is also possible due to the development of a malignant tumor in the pancreas and the progression of cancer to stage 3-4, which cannot be cured.
Hemorrhagic pancreatitis
Inflammation of the pancreas, accompanied by bleeding, is a very dangerous pathological condition. It develops when the wall of a vessel is damaged due to the possible influence of pancreatic enzymes on it.
If internal bleeding (especially from a large artery) is not diagnosed in time and abdominal surgery is not performed, blood loss can quickly become massive, hemorrhagic shock will develop, and the patient will die.
Pancreatic necrosis
Necrosis (destruction) of pancreatic tissue occurs for various reasons. Most often this happens due to acute destructive pancreatitis that develops after abuse of alcohol or junk food. Due to inflammation, swelling of the gland or the presence of stones in the excretory ducts, their lumen decreases, and pancreatic juice, aggressive to any tissue, remains inside the pancreas itself. Proteolytic enzymes destroy the gland and adjacent organs.
With the lightning-fast course of pancreatic necrosis and untimely provision of assistance to the patient, death is almost inevitable.
Death after pancreatic resection
For the formation of abscesses, ulcers, fistulas, and the development of pancreatic necrosis, surgical intervention is considered the only effective treatment. The operation is performed in several ways. The volume of intervention depends on the degree of damage to the pancreas: excision of necrotic tissue, resection of one section or (less often) the entire organ. But even after successful surgical treatment, death is also possible for several reasons:
- Postoperative bleeding.
- Reactive postoperative pancreatitis.
- Infectious complications and postoperative peritonitis.
- Diabetes mellitus, its complications (hyperglycemic coma and others) due to incorrectly selected insulin replacement therapy or the patient’s failure to comply with the recommendations of the attending physician.
What are the prognosis for treatment?
The prognosis of chronic pancreatitis is often unfavorable. Pancreatic necrosis, or death of gland cells, is especially difficult to treat. A fatal outcome in the described case is likely.
To avoid tragedy, patients need to clearly understand that the causes of chronic pancreatitis depend on the quality of food. When diagnosed, you should not drink alcoholic beverages or eat fatty foods. The diet includes protein (mandatory) and a minimum amount of fat.
How long do people with pancreatitis live is a question that worries every sick person. Life expectancy is influenced by a number of reasons:
- Patient's age. The earlier a person gets sick, the higher the chance of recovery.
- Drinking pattern - how often ethanol is consumed.
- The degree of damage to the gland.
A young guy who recently turned 20 years old and does not drink alcohol can live with this diagnosis into old age. A man in his declining years who regularly drinks alcohol shortens his life by ten or more years.
Factors influencing life expectancy:
- Life expectancy depends on the form of the disease. Acute attacks are often fatal. In severe forms, death from pancreatitis occurs in thirty percent of patients.
- The severity of the disease affects the general condition of the body.
- Complications in the form of cyst formation, bleeding from a damaged organ, and problems with the gastrointestinal tract aggravate the situation, mainly in older patients. The mortality rate reaches 20%.
- Age category of patients.
- Regular, thoughtful treatment.
- Compliance with the doctor's requests for treatment.
- Consumption of products prescribed by a gastroenterologist.
- Refusal to drink strong and low-alcohol alcoholic beverages.
Is it possible to die from pancreatitis - true or false?
Death from pancreatitis, or more precisely from pancreatic necrosis, is possible. You can imagine it in the form of several stages, which follow one after another:
- The acute form of pancreatitis can develop reactively within a few days and pancreatic cells begin to die.
- Foci of necrosis appear. Cell death occurs due to the fact that the gland's enzymes begin to digest its own cells - this is called pancreatic necrosis.
- Areas of the gland that are attacked by their own enzymes become necrotic.
- The intestinal walls become inflamed and destroyed due to enzymes, bacteria and undigested intestinal contents infecting everything around.
- Bleeding occurs, and in some places the blood, on the contrary, coagulates and clogs the vessels.
- Damage to several vital organs (liver, kidneys, intestines, lungs) is observed.
- Cardiac and respiratory arrest occurs, especially quickly in elderly patients; the heart simply cannot cope with the load.
- The skin becomes pale grayish in color, the lips turn blue, the pupils stop responding to light, body temperature and pressure drop to a minimum level.
- Near-death sensations arise.
- Clinical death from pancreatitis is registered. Death from pancreatic necrosis is when the body’s own enzymes digest everything in its path, affecting organ after organ.
Death from pancreatitis can occur for the following reasons:
- The structure of tissues and cells of the gland changes pathologically.
- When foci of necrosis form in the pancreas.
- With reactive inflammation in the pancreas and rapid spread of cell death.
- When the pressure in the bile ducts and pancreatic ducts increases.
- When the sphincter of Oddi, the muscle that limits access to bile and pancreatic juices, closes, a large number of enzymes are released into the pancreas and its cells die.
- The main risk factor that leads to death is clogged pancreatic ducts, as well as a dangerous combination of alcohol and fatty foods at one time.
What leads to death in pancreatitis?
Such an unfavorable prognosis depends on many factors: the severity, pathogenesis, nature and type of the disease, as well as the severity of the symptoms that appear in the patient.
- Alcohol abuse. This circumstance is the cause of death of people at a young age, especially for men, since they are the ones most susceptible to alcohol dependence. The mechanism of this connection is quite simple. With the regular intake of ethanol into the body, intoxication of organs such as the pancreas and liver occurs, as a result of which their tissues are inevitably destroyed. As a consequence, necrosis occurs, that is, the death of those structures in which the lesions are localized. The combination of alcohol and fatty foods becomes a real rocket bomb, which is why the majority of attacks, including fatal ones, occur during the holidays.
- Acute pancreatitis is the most common cause of death. The pathology in its acute form is quite complex; the patient experiences severe symptoms of a pronounced nature: severe pain in the abdominal area, incessant vomiting, diarrhea, and physical exhaustion. The first week of an exacerbation is a rather difficult period for the patient, during which various kinds of complications can arise, for example, necrosis and internal bleeding, and against their background - death. It is noteworthy that this can happen even after a timely diagnosis and the start of proper treatment.
- Chronic pancreatitis. In itself, this form of the disease is not as dangerous as the acute phase. However, it is characterized by periods of remission, which sooner or later give way to exacerbations, accompanied by the same severe symptoms. In addition, in conditions of a sluggish ongoing inflammatory process, the risk of developing complicating factors increases significantly: it can be either a cyst or a malignant tumor.
In general, the onset of death is preceded by:
- Changes in the cellular structure of the pancreas with subsequent necrotic processes;
- The penetration of enzymes into the blood vessels located near the organ, which occurs due to the impossibility of the outflow of pancreatic juice into the duodenum and its forced search for an outlet - as a result, enzyme substances are carried throughout the circulatory system and the patient dies.
Sometimes such a destructive process only takes a few days or even hours to take a person’s life.
Is it possible to die from pancreatic necrosis - statistics
The incidence of death from pancreatitis in its acute form occurs in one third of patients - these numbers are terrifying. Death with infected pancreatic necrosis of the pancreas occurs in 100% of cases. The statistics of deaths from this disease speaks for itself.
A greater number of patients with suspected fatal pancreatic necrosis of the pancreas require urgent surgical intervention. Timely and competent assistance increases the chances of recovery. The surgeon drains or excises areas of necrosis, but often the necrosis spreads again. After surgery, the patient is admitted to the intensive care unit and continues to be treated conservatively to delay or prevent death as much as possible.
In conservative treatment, antibiotics are used, fasting is prescribed for several days, and nutrients, hemodez, and polyglucin are administered parenterally. The blood is cleansed of toxins and breakdown products by transfusion. Somatostatin is prescribed, a hormone that stops the breakdown of pancreatic cells.
So, pancreatitis is fatal - they can follow each other and this must be remembered, especially for elderly patients, you should follow a diet and not abuse alcoholic beverages, then you can extend your life for many years.
ETIOLOGY AND PATHOGENESIS
The main causes of chronic pancreatitis are alcohol abuse and cholelithiasis (just as in the case of acute pancreatitis). Alcohol is the main toxic factor for the pancreas. With gallstones, inflammation develops due to the penetration of infection from the bile ducts into the gland or due to the reflux of bile.
Causes and risk factors of chronic pancreatitis:
- Alcohol abuse . Daily consumption of two liters of beer or 100 grams of vodka after 3-5 years leads to changes in the tissues of the pancreas, and after 10-15 years – to chronic pancreatitis. Long-term toxic effects of alcohol on pancreatic cells cause their death. This leads to a decrease in secretory functions. Fibrous (scar) tissue grows in place of dead cells.
- Smoking increases the harmful effects of alcohol on the gland. Smokers are twice as likely to suffer from chronic pancreatitis. The greater the daily number of cigarettes and the length of smoking, the higher the risk of developing the disease.
- Diseases of the gallbladder , biliary tract and duodenum ;
- An abundance of fatty, spicy and fried foods , as well as a decrease in proteins and vitamins in the diet;
- Long-term use of certain medications (hormones, cytostatics) and individual hypersensitivity to drugs (usually sulfonamides, non-steroidal anti-inflammatory drugs, some diuretics);
- Impaired blood supply due to thrombosis, atherosclerosis, embolism of glandular vessels;
- Immune failures;
- Presence of specific gene mutations.