Patient's complaints
Already from the first complaints of the patient, it is possible to accurately diagnose acute or chronic inflammation in the pancreas, thereby making a differential diagnosis at the interview stage. The following complaints indicate the disease:
- The pain is intense, occurring half an hour after eating fatty or fried foods, or after drinking alcoholic beverages. They are encircling in nature, spreading throughout the abdomen with irradiation into the lower back and shoulder blade. The pain syndrome persists for a long time and is not relieved by taking the usual analgesics.
Important! Not all patients experience pain. In 15% of cases, the pathology is painless or asymptomatic, which leads to errors in diagnosis.
- Complaints of belching, vomiting, flatulence, loose, frequent stools. Digestive disorders are caused by atony of the duodenum and the backflow of pancreatic juice into the ducts. For both acute and chronic pancreatitis, vomiting is specific and does not bring relief. On the contrary, the patient continues to feel nausea. In this case, there is a bitter taste in the mouth or a bitter taste in the vomit.
- Weight loss, muscle weakness, vitamin deficiency. These complaints are caused by pancreatic enzyme deficiency.
- Thirst, dry mouth, “hungry” fainting are symptoms characteristic of diabetes mellitus. They are due to the fact that the affected organ does not produce enough of the glucose-lowering hormone insulin.
General blood analysis
If the development of chronic or acute pancreatitis is suspected, a general blood test is always prescribed. It provides the most extensive information about the condition of the pancreas. However, a diagnosis cannot be made based solely on the results of this study. Additional examination of the patient will be required.
For cholecystitis or pancreatitis, a general blood test shows the following results:
- decreased red blood cell levels;
- decrease in hemoglobin level;
- increased erythrocyte sedimentation rate;
- a strong increase in the level of leukocytes (in these diseases the level of leukocytes is 2-3 times higher than normal);
- increase in hematocrit.
Blood test values for pancreatitis in women and men may increase or decrease. Such changes are caused by the development of inflammatory processes in the pancreas and the release of toxic substances into the blood. And in order to understand what indicators indicate the development of this disease, you first need to know their norm. Normal blood counts are shown in the table below.
Normal blood test results
History taking
An equally important stage for making a diagnosis. The patient is asked about the time of onset of pain and whether its occurrence is associated with food intake. In chronic pancreatitis, pain is constant or occurs after eating fatty and fried foods, as well as other errors in the diet. The first pain sensations appear after 30-40 minutes. after eating. It is also important how the patient stopped the pain attack and whether it helped him. In an acute process, the pain is more intense.
The doctor asks whether there was a decrease in appetite on the eve of the exacerbation, a feeling of dryness or bitterness in the mouth. In acute pancreatitis, the patient has all these symptoms. The time of onset of dyspeptic disorders and the nature of vomit are also significant for making a diagnosis. Another criterion for diagnosis is the nature of the stool. In both acute and chronic pancreatitis, the stool is liquid, yellow, with an admixture of fat in the stool (steatorrhea).
Visual inspection
When examining, pay attention to the skin. In chronic biliary-dependent pancreatitis, due to obstructive jaundice, the skin, sclera, and oral mucosa may be jaundiced.
Then the doctor palpates the abdomen, and the patient notes pain at the point of projection of the gallbladder onto the abdominal wall. An enlarged gallbladder that can be easily palpated will also help to suspect the diagnosis of chronic biliary-dependent pancreatitis.
On examination, the following symptoms are noted: absence of pulsation of the abdominal aorta during palpation (due to swollen pancreas), positive phrenicus symptom (pain that occurs in response to palpation between the legs of the sternocleidomastoid muscle), thinning of the subcutaneous fat in the area projections of the pancreas.
Signs of acute inflammation
Pain in the epigastric region is a symptom indicating acute pancreatitis. Differential diagnosis in the presence of this sign is carried out immediately, because the pain is often so strong that people cannot lie or sit quietly. Only after diagnostics and an accurate diagnosis can specialists take any measures to alleviate the condition of patients.
Another common sign of acute inflammation of the pancreas is vomiting, which in most cases is repeated. It does not bring relief to sick people. Their condition only worsens due to vomiting. Other symptoms of acute pancreatitis include:
- pallor of the skin, acrocyanosis (the skin acquires a bluish color);
- bloating;
- retention of gases, stool;
- severe weakness.
Laboratory diagnostic methods
Determination of amylase content in blood
This is not a sufficiently informative study, since amylase in the blood in acute pancreatitis is determined only on the first day of the disease. Amylase enters the blood from destroyed pancreatic cells. An increase in this enzyme does not always speak in favor of pathology, since most of this compound enters the blood from saliva, and not from the gland. However, if the patient was admitted within the first hours of the onset of pain and a biochemical blood test showed an increase in amylase levels, then this allows one to suspect the disease.
Determination of pancreatic enzymes in a blood test
The main enzymes studied are lipase and elastase.
Important! All indicators (inflammation increases). This more sensitive analysis, however, does not allow us to speak with complete certainty about acute or chronic pancreatitis, since these compounds are also found in large quantities in other organs.
Functional tests
Designed to evaluate the excretory function of the pancreas. There are direct (probe) and indirect studies. In this case, the conclusion indicates which type of secretion predominates in the patient. In acute pancreatitis, enzyme function sharply decreases, which leads to hyposecretion of all hormones and digestive enzymes.
Stool analysis
It is produced to determine the quantitative content of fat in it. Under conditions of hyposecretion, digestion is disrupted, which leads to disturbances in the breakdown and absorption of nutrients. A sign indicating chronic pancreatitis will be the content of undigested fats in the stool (steatorrhea). After this, the quantitative ratio of fats to other undigested nutrients is determined. A test is used to determine the content of elastase in stool. These studies are highly specific for pancreatic disease.
Biochemical urine analysis
Determination of amylase (diastase) content in urine. Also a highly specific assay that is simple and inexpensive to use. It is prescribed as soon as a patient with acute or chronic pancreatitis is admitted to the hospital. There are no clear boundaries for the increase in diastase in the urine, since the level of the enzyme will depend on the severity of the disease and how much of the organ has undergone necrosis and decay. In an acute process, the amount of amylase exceeds the normal level by 5-10 times.
Differential methods for identifying the disease
“Acute abdomen,” as pancreatitis is popularly called, is similar in symptoms to a number of other diseases. They can be differentiated by distinctive symptoms:
- An attack of intestinal obstruction is diagnosed by cramping pain syndrome. An x-ray of the peritoneal area is prescribed, which demonstrates visually noticeable swelling of the large intestine, and not an enlargement of the pancreas.
- Cholecystitis is more characterized by pain that “shoots” into the right forearm. Pancreatic pain syndrome is very similar, but more often resonates in the rib on the left. Only an ultrasound examination, which finds the specific location of the inflamed area, can reliably differentiate these two similar pathologies.
- A perforated ulcer is recognized by its “board-shaped” abdomen, which is uniformly hard. It is more comfortable for the patient to lie on his back, in an equal position (whereas with pancreatitis, the sufferer wants to curl up). A plain X-ray of the abdominal cavity will indicate gaseous accumulations.
In addition to gastrointestinal diseases, the symptoms of pancreatitis are sometimes confused with cardiovascular problems. For example, older people are more likely than younger people to get mesothrombosis, which begins with pain similar to pancreatic pain. Doubts are dispelled by angiography and laparoscopy.
Mandatory electrocardiography helps to avoid myocardial infarction, which is done both in the hospital (immediately upon the arrival of the ambulance) and on an outpatient basis (based on the first complaints of the patient).
Table of main blood parameters that change during pancreatitis
| Index | Values for pancreatitis |
| Amylase In blood: In urine (diastasis): | ≥150 units/l ≥320 units |
| Lipase | ≥ 60 IU/l |
| Elastase in 1 g of feces | ≤ 200 µg |
| Blood leukocytes | ≥9x109 |
| ASAT | ≥37 U/l |
| AlAT | ≥45 U/l |
| Total protein | ≥83 g/l |
| C-reactive protein | ≥5 mg/l |
| ESR | ≥20mm/h |
| Direct bilirubin | ≥8 µmol/l |
| Indirect bilirubin | ≥19 µmol/l |
Instrumental diagnostic methods
By and large, all patients with this disease undergo instrumental examination only with an ultrasound examination of the abdominal organs. This is due to the fact that the diagnosis can be easily made after interviewing, examining the patient and obtaining laboratory tests. Ultrasound is a high-quality and reliable first-line study, as it is inexpensive and highly informative. All other studies are of little information and are not highly effective for diagnosis. Their use is justified only when it is not possible to visualize the affected parts using ultrasound examination or when there is a suspicion of the presence of a space-occupying formation in the organ (cancerous tumor, cyst, pseudocyst). In this case, the question arises about the surgical operation and the extent of resection.
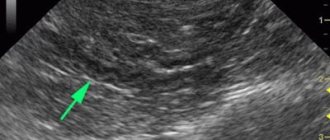
Ultrasound examination
"Gold standard" for diagnosis. The doctor will easily see diffuse changes in the tissue of the affected organ, thickening and swelling of the pancreatic capsule. In chronic pancreatitis, calcifications and petrifications, areas of parenchyma destruction, are detected. The advantage of this study is that it makes it possible to assess the condition of other organs (gallbladder, liver and their ducts). This is important when the outflow of secretions is impaired due to stones and the presence of cholecystitis, since in this case all the conditions for the development of the disease are created.
Important! Currently, new methods of ultrasound diagnostics have been developed. In particular, endoscopic ultrasound and intraductal ultrasound of the pancreas. These studies make it possible to insert sensors into the stomach or into the ducts themselves, and the doctor can study in more detail and give an opinion on the condition of the organ. The disadvantage of these studies is their invasiveness, which exacerbates inflammation and organ destruction.
CT scan
Most often, this study is prescribed when complications occur. X-ray examination allows you to study in detail the structure of an organ (including the circulatory system), assess the degree of destruction, and determine the amount of living and healthy tissue.
Endoscopic retrograde cholangiopancreatography (ERCP)
For biliary-dependent pancreatitis, ERCP is performed. A special probe is inserted into the main duct, the opening of which opens on the large duodenal papilla, and a contrast agent is supplied. After this, the patient is given an x-ray. Such an examination allows you to assess the patency of many (even the smallest) ducts, determine the presence or absence of stones and other possible obstacles (strictures, adhesions, kinks). During the examination, small stones can be removed, which will then be removed naturally. This surgical method is minimally invasive, so it is now preferred.
Rarely used instrumental diagnostic methods
- Fibrogastroduodenoscopy (FGDS) - allows you to assess the condition of the major papilla of the duodenum, evaluate the final sections of the duct itself, and evaluate the functionality of the sphincter of Oddi.
- Plain radiography of the abdominal cavity is a study used for differential diagnosis. Often, with this disease, there are no changes in the image, except in cases where petrification (areas of calcification) have already formed in the pancreas. This sign allows us to fully guarantee that the patient has chronic pancreatitis.
- Laparoscopy. More of a therapeutic rather than a diagnostic method. It is used in controversial situations when the above studies could not completely visualize the affected organ. During diagnosis, various surgical procedures can be used for therapeutic purposes.
Prevention of pancreatitis
It is quite possible to prevent the development of pancreatitis. First of all, you need to look after your health. Some diseases of the biliary tract and gall bladder, diseases of the gastrointestinal tract provoke inflammation of the pancreas. If your health worsens and suspicious symptoms appear, you should immediately consult a doctor, take the necessary tests and undergo prescribed examinations.
Another important preventative measure is to reduce alcohol consumption. Experts advise even completely healthy people not to drink alcohol-containing drinks in large quantities. If you have diseases of the gastrointestinal tract, you should completely avoid alcohol.
In conclusion, it is worth noting that pancreatitis (clinic, diagnosis, treatment of this disease) is a current medical topic. If you experience symptoms indicating inflammation of the pancreas, you should consult a doctor. An advanced disease can lead to serious life-threatening complications.