Production of hydrochloric acid in the stomach
What is this liquid needed for and what are the risks of disrupting its production? The importance of hydrochloric acid in the stomach is difficult to overestimate, because it is an important part of the digestive process. Changes in acidity lead to inflammatory diseases of the upper gastrointestinal tract, which require serious drug therapy.
Digestion is a complex function of the gastrointestinal tract, which is regulated by the nervous and endocrine systems. Food processing is carried out in several stages, starting with the oral cavity. The main breakdown of components occurs in the stomach. The main role is played by the secretion, which contains hydrochloric acid.
The importance of hydrochloric acid in the stomach can hardly be overestimated, because it is an important part of the digestive process
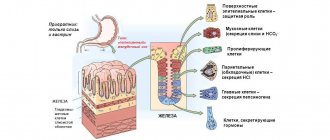
Hydrochloric acid plays a major role in the complex digestive system. The environment in the human stomach is provided by HCl. It is produced by parietal cells of the fundus and body of the organ. This is where most of it is formed. As it moves towards the antrum, the pH level decreases due to partial neutralization by bicarbonates.
What is the gastric compartment
Gastric juice is a substance with a sour taste. The average weight of gastric juice is from 1.002 to 1.007 g/cm3. No color. The acid index ranges from 0.9 to 1.5. The acidic reaction is caused by the hydrochloric acid content of gastric juice. Other characteristics are:
- water - approximately 99.5% (for this reason, its color is normally absent),
- presence of dry components of gastric juice - 0.5%,
- mineral components of gastric juice - salts of sulfuric, hydrochloric acids, sodium, calcium and other elements,
- the presence of enzymes that play an important role in digestion, creatinine and other components is detected.
The composition of gastric juice includes such highly active substances as:
- Pepsin-A ensures the hydrolyzing activity of gastric secretions into proteins.
- Pepsin-C metabolizes hemoglobin.
- Gelatinase dissolves gelatin and collagen.
- Chymosin promotes the breakdown of casein.
- Lipase is produced to digest milk fats.
- Lysozyme provides a bactericidal effect. Minor amounts of this enzyme are formed in the oral cavity.
- Urease breaks down urea.
- Castle factor plays an important role in digestion: it absorbs cyanocobalamin.
There are total, free and protein-bound hydrochloric acid. Their exact content is shown by the biochemistry of gastric contents.
Sometimes the color of the liquid may change. If it is yellowish, it means that there are bile impurities in the stomach. A red or brownish tint indicates that blood has entered the stomach. A putrid odor indicates that intense processes of decay or fermentation are occurring in this organ.
Important! If, according to the diagnostic results, the color of the stomach secretion changes in the patient, he needs to undergo an additional diagnostic examination. This condition may indicate the development of dangerous pathologies.
Production of hydrochloric acid in the stomach
The glands of the stomach produce gastric juice under the influence of hormonal substances and regulators of metabolic processes. The secretion contains several important components that ensure normal functioning of the gastrointestinal tract. The composition of gastric juice is represented by the following substances:
- hydrochloric acid;
- bicarbonates;
- enzymes - pepsinogens, pepsin isoforms;
- mucus;
- Castle factor, an enzyme for the absorption of vitamin B₁₂.
The parietal cells of the gastric glands produce hydrochloric acid in response to the entry of bolus food into the upper digestive tract. It provides the level of acidity that is necessary to break down nutrients and move them into the intestines.
Other components of gastric juice provide a protective role. These are bicarbonates and mucus. Accessory cells produce mucus, which concentrates on the surface of the mucous membrane. Its thickness is up to 6 mm. The gel contains alkaline components in an amount of 45 mmol/l.
Their task is to neutralize the acid of the food bolus, which promotes the opening of the sphincter of the pyloroduodenal zone and the movement of chyme into the duodenum. Important! Lack of bicarbonates and mucus gel contributes to increased acidity in the stomach.
Gastric acidity tests
For a long time in medicine, gastric acidity was determined by the fractional method, and many types of stimulants were used. The juice extracted from the stomach was subjected to a titration procedure using special dyes. The acidity level in this case is established based on the obtained juice sample outside the stomach. But today this method is no longer used, since its reliability is in doubt.
Today, in most clinics, two methods are used to study gastric juice and determine its acidity: probing and acidotest (probeless research method).
Probing the stomach using a special probe with a diameter of about 5 mm, through which the level of acidity is determined directly in the stomach.
If a person cannot tolerate the introduction of foreign objects into the stomach, then an acid test is used for testing, in which the acidity level is determined by the results of a urine test and its staining.
Hydrochloric acid production mechanism in the stomach
The formation mechanism begins from the moment a person catches the smell of food. The parasympathetic NS (nervous system) is activated, acetylcholine and gastrin irritate the receptors of the parietal cells, which leads to the onset of hydrochloric acid production. Its secretion occurs while food is in the stomach. After its evacuation into the intestine, synthesis is blocked by somatostatin.
As food moves forward, it enters first the acid-forming and then the acid-neutralizing zones of the stomach. They are separated by an intermediary zone, which corresponds to the transition of the fundus to the antrum. Therefore, a slightly acidic environment with a pH level of 4.0-6.0 is replaced by a strongly acidic environment, where the pH is less than 3.0.
The main acid-forming function is performed by hydrochloric acid in the stomach. Correction of acid formation is carried out by hormonal and biologically active components as the chyme moves. The fundic glands of the body and antrum secrete acid. The process is regulated with the help of histamine. This substance is produced when the walls of the organ are stretched by food.
Gradually, the concentration of gastric juice increases, which leads to the activation of somatostatin. It blocks the secretion of hydrochloric acid. Another neutralizing mechanism is bicarbonates, which make food alkaline. An optimal environment with low acidity is needed for the reflex opening of the sphincter and the creation of normal peristalsis in the stomach and duodenum.
Hypersecretion of hydrochloric acid causes retention of chyme in the stomach; its deficiency leads to its premature entry into the intestine. The process of fermentation and absorption of nutritional components is disrupted.
Regulation of hydrochloric acid secretion
Stimulation of hydrochloric acid secretion
parietal cells is carried out
directly
and
indirectly
through other mechanisms. [86]
Three-receptor parietal cell model [87]
The mediators that play the role of first intermediaries in the induction of HCl secretion include: [88]
1. Acetylcholine
2. Gastrin
3. Histamine
It is assumed that there is a strong obligatory interaction between the histamine and gastrin receptors and a weaker, optional interaction between the histamine and acetylcholine receptors.
H2 receptor antagonists block histamine receptors (according to [28])
Acetylcholine, histamine and gastrin are among the mediators that play the role of first mediators in the induction of HCl secretion.[89]
When hormones or effector substances interact with specific receptors localized on the cell surface, a second messenger is formed - cAMP or Ca2+ ions (calmodulin), which induces specific cell activity. [90]
It is assumed that as a result of the action of gastrin and acetylcholine with receptors, the intracellular concentration of Ca2+ increases, histamine increases the formation of cAMP [91].
Ca2+ and cAMP as “second messengers” stimulate HCl secretion.[92]
Directly
The secretion of hydrochloric acid by parietal cells is stimulated by cholinergic fibers of the vagus nerves, the mediator of which,
acetylcholine (AX), excites M-cholinergic receptors of the basolateral membranes of glandulocytes.
The effects of ACh and its analogues are blocked by atropine. Indirect stimulation of cells by the vagus nerves is also mediated by gastrin and histamine. [93] Gastrin [94] is released from G-cells, the main amount of which is located in the mucous membrane of the pyloric part of the stomach. [95] After surgical removal of the pyloric part, gastric secretion decreases sharply. [96]
The release of gastrin is enhanced by impulses of the vagus nerve, as well as local mechanical and chemical irritation of the pyloric part of the stomach.
Chemical stimulators of G-cells are products of protein digestion - peptides and some amino acids, extractives of meat and vegetables. If the pH in the antrum of the stomach decreases, which is due to an increase in the secretion of hydrochloric acid by the gastric glands, then the release of gastrin decreases, and at a pH of 1.0 it stops and the volume of secretion sharply decreases.
Thus, gastrin takes part in the self-regulation of gastric secretion depending on the pH value of the contents of the antrum. Gastrin most stimulates the parietal glandulocytes of the gastric glands and increases the secretion of hydrochloric acid.
A powerful chemical stimulant of gastric gland secretion is histamine .
Under the influence of histamine, gastric juice is formed, rich in hydrochloric acid and poor in enzymes. [97]
Histamine is produced in the ECL cells of the gastric mucosa. [98]
The release of histamine is mediated by gastrin. [99]
Histamine stimulates glandulocytes, affecting the H2 receptors of their membranes and causing the release of large amounts of juice that is high in acidity but poor in pepsin. [100]
The stimulating effects of gastrin and histamine depend on the preservation of the innervation of the gastric glands by the vagus nerves: after surgical and pharmacological vagotomy, the secretory effects of these humoral stimulants are reduced. [101]
Gastric secretion is also stimulated by the products of protein digestion absorbed into the blood. [102]
Inhibition of hydrochloric acid secretion
cause secretin, CCK, glucagon, GIP, VIP, neurotensin, polypeptide UR, somatostatin, thyroliberin, enterogastron, ADH, calcitonin, oxytocin, prostaglandin PGE2, bulbogastron, cologastron, serotonin (see Appendix 302161835 Table 9.2). [103]
The release of some of them in the corresponding endocrine cells of the intestinal mucosa is controlled by the properties of chyme. In particular, inhibition of gastric secretion by fatty foods is largely due to the effect of CCK on the gastric glands. Increasing the acidity of the contents of the duodenum inhibits the secretion of hydrochloric acid by the glands of the stomach. Inhibition of secretion occurs reflexively, as well as due to the formation of hormones in the duodenum. [104]
The mechanism of stimulation and inhibition of hydrochloric acid secretion by various neurotransmitters and hormones is not the same. Thus, ACh enhances acid secretion by parietal cells by activating membrane Na+, K+-ATPase, increasing the transport of Ca2+ ions and the effects of increased intracellular cGMP content, releasing gastrin and potentiating its effect. [105]
Gastrin enhances the secretion of hydrochloric acid through histamine, as well as by acting on membrane gastrin receptors and enhancing the intracellular transport of Ca2+ ions. Histamine stimulates the secretion of parietal cells through their membrane H2 receptors and the adenylate cyclase (AC)-cAMP system. [106]
[ND10]
Stimulators of pepsinogen secretion by chief cells
are cholinergic fibers of the vagus nerves, gastrin, histamine, sympathetic fibers ending on beta-adrenergic receptors, secretin and CCK.
Increased secretion of pepsinogens by the main cells of the gastric glands is carried out by several mechanisms. Among them are an increase in the transport of Ca2 +
into the cell and stimulation of Na
+,
K
+‑
ATPase; increased intracellular movement of zymogen granules, activation of membrane phosphorylase, which enhances their passage through apical membranes, activation of the cGMP and cAMP system.[107]
These mechanisms are activated or inhibited to varying degrees by various neurotransmitters and hormones, their direct and indirect effects on chief cells and pepsinogen secretion. It has been shown that histamine and gastrin influence it indirectly - they increase the secretion of hydrochloric acid, and a decrease in the pH of the stomach contents through a local cholinergic reflex increases the secretion of chief cells. The direct stimulating effect of gastrin on them has also been described. In high doses, histamine inhibits their secretion. CCK, secretin and β-adrenergic agonists directly stimulate the secretion of chief cells, but inhibit the secretion of parietal cells, which indicates the existence of different receptors for regulatory peptides on them. [108]
Stimulation of mucus secretion by mucocytes
carried out by cholinergic fibers of the vagus nerves. Gastrin and histamine moderately stimulate mukocytes, apparently due to the removal of mucus from their membranes with pronounced secretion of acidic gastric juice. A number of inhibitors of hydrochloric acid secretion - serotonin, somatostatin, adrenaline, dopamine, enkephalin, prostaglandin PGE2 - enhance mucus secretion. It is believed that PGE2 enhances the secretion of mucus by these substances. [109]
When eating and digesting, blood flow increases in the intensely secreting glands of the stomach, which is ensured by the action of cholinergic nervous mechanisms, peptides of the digestive tract and local vasodilators. In the mucous membrane, blood flow increases more intensely than in the submucosa and muscle layer of the gastric wall. [110]
Phases of gastric secretion [111]
Nervous, humoral factors and paracrine mechanisms finely regulate the secretion of gastric glands, ensure the release of a certain amount of juice, acid and enzyme secretion, depending on the quantity and quality of food taken, the efficiency of its digestion in the stomach and small intestine. The secretion that occurs in this case is usually divided into three phases. [112]
The initial secretion of the stomach occurs reflexively in response to irritation of distant receptors excited by the sight and smell of food, and the entire situation associated with its intake (conditioned reflex irritations). [113]
In addition, the secretion of the stomach is excited reflexively in response to irritation of the receptors of the oral cavity and pharynx by food taken (unconditioned reflex irritations). These reflexes provide triggering effects on the gastric glands. Gastric secretion, caused by these complex reflex influences, is usually called the first, or cerebral, phase of secretion (see Fig. 9.8). [114]
Gastric juice, secreted at the beginning of the act of eating, as well as under the influence of conditioned reflex stimuli, was called “appetizing” by I.P. Pavlov, preparing the stomach in advance for eating. [115]
The mechanisms of the first phase of gastric secretion were studied in experiments on esophagotomized dogs with a gastric fistula. When feeding such a dog, food falls out of the esophagus and does not enter the stomach, but 5-10 minutes after the start of imaginary feeding, gastric juice begins to be released. Similar data were obtained in a study of people suffering from narrowing of the esophagus and, as a result, undergoing gastric fistula surgery. Chewing food caused people to secrete gastric juice. [116]
Reflex influences
to the gastric glands are transmitted through the vagus nerves. After their cutting in an esophagotomyrrhized dog, neither imaginary feeding nor the sight and smell of food causes secretion. If the peripheral ends of the cut vagus nerves are irritated, gastric juice with a high content of hydrochloric acid and pepsin is observed. [117]
is also included in the stimulation of the gastric glands in the first phase .
Proof of this is the increase in gastrin content in the blood of people during imaginary feeding. After removal of the pyloric part of the stomach, where gastrin is produced, secretion decreases in the first phase. [118]
Secretion into the brain phase depends on the excitability of the food center and can be easily inhibited by stimulation of various external and internal receptors. Thus, poor table setting and untidiness of the eating area reduce and inhibit gastric secretion. Optimal eating conditions have a positive effect on gastric secretion. Taking strong food irritants at the beginning of a meal increases gastric secretion in the first phase. [119]
The secretion of the first phase is superimposed by the secretion of the second phase, which is called gastric, as it is caused by the influence of food contents while it is in the stomach. The presence of this phase of secretion is proven by the fact that putting food into the stomach through a fistula, pouring solutions into the stomach through it or a probe, and irritating its mechanoreceptors cause the secretion of gastric juice. The volume of secretion is 2-3 times less than during natural food intake. This emphasizes the great importance of triggering reflex influences,
carried out mainly in the first phase on the gastric glands.
In the second phase, the gastric glands experience mainly corrective influences.
These influences, by strengthening and weakening the activity of the glands, ensure that secretion corresponds to the quantity and properties of food gastric contents, i.e., they correct the secretory activity of the stomach. [120]
When food enters the stomach, the gastric phase of secretion begins. If you put meat through a fistula into the stomach, then after 30 minutes the secretion of gastric juice appears. This is the result of both mechanical and chemical irritations. Among the chemical factors, the most important hormone is gastrin,
which is formed in the wall of the pyloric part of the stomach in the form of inactive
progastrin.
[121]
Juice secretion during mechanical stimulation of the stomach is excited reflexively from the mechanoreceptors of the mucous membrane and the muscular layer of the stomach wall. Secretion decreases sharply after transection of the vagus nerves. In addition, mechanical irritation of the stomach, especially its pyloric part, leads to the release of gastrin from G cells. [122]
Increasing the acidity of the contents of the antrum of the stomach inhibits the release of gastrin and reduces gastric secretion. In the fundic part of the stomach, the acidity of its contents reflexively enhances secretion, especially the release of pepsinogen. Histamine has a certain importance in the implementation of the gastric secretion phase, a significant amount of which is formed in the gastric mucosa. [123]
Meat broth, cabbage juice, and protein hydrolysis products, when introduced into the small intestine, cause the release of gastric juice. Nervous influences from intestinal receptors on the gastric glands ensure secretion in the third, intestinal, phase. Excitatory and inhibitory influences from the duodenum and jejunum on the gastric glands are carried out with the help of nervous and humoral mechanisms that correct secretion. Nervous influences are transmitted from mechano- and chemoreceptors of the intestine. Stimulation of the gastric glands in the intestinal phase is primarily the result of the entry into the duodenum of insufficiently physically and chemically processed stomach contents. The products of hydrolysis of nutrients, especially proteins, that are absorbed into the blood take part in stimulating gastric secretion. These substances can stimulate the gastric glands indirectly through gastrin and histamine, as well as directly acting on the gastric glands. [124]
Inhibition of gastric secretion in its intestinal phase is caused by a number of substances in the intestinal contents, which, according to decreasing strength of inhibitory action, are arranged in the following order: fat hydrolysis products, polypeptides, amino acids, starch hydrolysis products, H+ (pH below 3 has a strong inhibitory effect). [125]
The release of secretin and CCK in the duodenum under the influence of the stomach contents entering the intestine and the resulting hydrolysis products of nutrients inhibits the secretion of hydrochloric acid, but enhances the secretion of pepsinogen. Gastric secretion is also inhibited by other intestinal hormones from the gastronomic group and glucagon, as well as serotonin. [126]
The production of hydrochloric acid in the stomach is stimulated
The main acid-forming function is performed by hydrochloric acid in the stomach. Correction of acid formation is carried out by hormonal and biologically active components as the chyme moves. The fundic glands of the body and antrum secrete acid. The process is regulated with the help of histamine. This substance is produced when the walls of the organ are stretched by food.
Gradually, the concentration of gastric juice increases, which leads to the activation of somatostatin. It blocks the secretion of hydrochloric acid. Another neutralizing mechanism is bicarbonates, which make food alkaline. An optimal environment with low acidity is needed for the reflex opening of the sphincter and the creation of normal peristalsis in the stomach and duodenum.
The production of hydrochloric acid in the stomach is normal
The concentration of HCl in the entire amount of synthesized digestive juice is an indicator of acidity. The symptoms of various gastrointestinal diseases depend on this indicator. The unit of measurement for this value is pH.
The concentration of HCl in the entire amount of synthesized digestive juice is an indicator of acidity
Acidity levels vary in different parts of the stomach. The mucous membrane in its lumen has this indicator 1.2-1.6 pH, and on the mucous membrane facing the epithelium 7.0 pH, that is, neutral. However, the average value is not taken into account when diagnosing. Much more important is the change in acidity per day in several parts of the stomach. Sometimes you need to find out what happens to her when using irritants and stimulants
There are certain acidity standards for the human stomach, deviation from which indicates a change in the healthy gastric environment (values are indicated in pH units):
- minimum – 8.3;
- normal in the body of the stomach (determined on an empty stomach) – 1.5-2.0;
- antrum - 1.3-7.4;
- epithelium – 7.0;
- maximum – 0.86.
The neutral value of an acidic environment corresponds to a value of 7.0. If the indicator exceeds this figure, then an alkaline environment is present, and if it falls below, it is acidic.
Production of hydrochloric acid in the stomach under stress
Stress stimulates excessive production of catecholamines - biologically active substances that enter the blood as a response to physical or psycho-emotional stress. The most famous of them are adrenaline and norepinephrine. These hormones help reduce the production of mucus, which helps protect the stomach from the negative effects of microorganisms, pepsin and hydrochloric acid.
By affecting the central nervous system, they can disrupt the motility of the digestive system and impair its blood circulation. Thus, stress can lead to inhibition of peristalsis and activation of aggressive factors (high concentrations of hydrochloric acid, increased production of pepsin, as well as the proliferation of helicobacter pylori bacteria). As a result, damage to the mucous membrane often occurs, inflammation develops, and with it pain occurs.
Drugs that reduce the production of hydrochloric acid in the stomach
Tablets for normalizing the acidic environment act primarily on the parietal cells, which are responsible for its formation. Then they stabilize the mucus production and bind the acid that has already been produced. Medicines that reduce acid levels are immediate and are divided into two groups:
- Antacids - absorb harmful particles, neutralizing acid levels. At the same time, they envelop the walls of the stomach and stimulate the production of protective mucus. The group of antacids includes Rennie, Gastal, Almagel, Maalox, and Phosphalugel. Antacids are sold without prescriptions and are used in emergency situations (heartburn, belching, epigastric pain), but the positive effect does not last long.
Antacids - absorb harmful particles, neutralizing the acid level
Alginates - promote the formation of a protective film on the walls of the stomach, absorb hydrochloric acid and remove it from the body, support the immune system. "Gaviscon", "Laminal", "De-nol", "Vicalin". The relief from alginates lasts longer.- Blockers. Almost everyone suffering from a high acidic environment suffers from heartburn. If antacids fail to restore the required level of acidity, the doctor may prescribe blockers that act directly on the cells. They inhibit their work, lower the level of acid that the body cannot cope with on its own, and contribute to the formation of a protective layer. These medications include Omeprazole, Esomeprazole, and Pantoprazole. The environment that forms after taking medications is ideal for healing ulcers, erosions and eliminating the inflammatory process.
Drugs that increase the production of hydrochloric acid in the stomach
Gastric acidity is presented in the form of basal and stimulated secretion, that is, the quantitative content of hydrochloric acid in the stomach on an empty stomach and after a test breakfast is determined. Acidity will be low if:
- basal acidity is noted at pH levels from 2.1 to 6.0;
- and stimulated - from 2.1 to 3.0.
If the decline in the secretory function of the stomach is noted even more, that is, basal more than 6.0, and stimulated more than 5.0, such gastritis is defined as anacid. Low stomach acidity requires treatment of the inflammatory process, restoration of parietal cells and their functions.
Increasing the concentration of hydrochloric acid is the main task in the treatment of gastritis of this form. For this purpose, not only drug therapy is used. Proper nutrition plays a big role in normalizing digestive processes.
To increase the acidity of gastric juice, complex use of medications is necessary.
- Cytochrome, Limontar, Pentagastrin - stimulate the secretory function of the gastric mucosa, helping to increase it;
- Pepsin, Panzinorm - drugs that replace hydrochloric acid;
- Festal, Creon - enzyme agents aimed at improving food digestion processes;
- Cerucal, Motilium - drugs that improve the motor function of the stomach and intestines;
- No-shpa, Spasmol - drugs that relieve spasms of smooth muscles;
- restorative treatment and vitamin therapy.
Often, against the background of insufficient production of hydrochloric acid by the stomach, Helicobacter pylori is activated. In this case, antibiotic therapy is introduced into the treatment - 2 or 3 drugs at the same time, mainly a complex of amoxycycline and tinidazole
Sources
https://med univer.com/Medical/Physiology/122.html
https://www.kor valol.ru/article/17
https://okishechnike.com/info/preparaty-povyshajushhie-kislotnost-zheludka/
https://yeste tika.ru/kakimi-zhelezami-vyrabatyvaetsya-solyanaya-kislota-pochemu-kisloty-v.html
https://xn- -201-5cd3baaocfczhn.xn--p1ai/bolezni-pishhevoda/solyanaya-kislota-v-zheludke-kak-vyrabatyvaetsya-funktsii-ee-kontsentratsiya.html
History of the study of gastric juice acidity[edit | edit code]
At the beginning of the 16th century, Paracelsus suggested the presence of acid in the stomach, believing that acid appears when drinking acidic water. The English physician and biochemist William Prout determined in 1824 that the acid contained in gastric juice is hydrochloric acid. He also introduced the concept of free
,
bound
hydrochloric acid and
total acidity of gastric juice
. In 1852, physiologist Friedrich Bidder and chemist Karl Schmidt published the book “Digestive Juices and Metabolism,” which laid the foundation for the titration method for determining the acidity of gastric juice and finally dispelled doubts that it is hydrochloric acid that is normally secreted by the stomach. Rigel in 1886 and Schüle in 1895 began to determine the acidity of gastric juice for the purpose of diagnosing and treating gastroenterological diseases.
One of the first to propose probing of gastric juice was the German doctor Adolf Kussmaul. The creation of clinical methods and gastric tubes for studying gastric secretion by aspiration methods (mainly by the efforts of the first gastroenterologists from Germany: Wilhelm von Leibe, Karl Ewald and Ismar Boas and the American trained in Germany Max Einhorn) actually formed a new medical discipline - gastroenterology.