Why and in what cases is tube feeding organized?
As a rule, a tube is installed for food intake:
- if it is impossible to get adequate nutrition through the mouth during radiation treatment (pain, swelling);
- if necessary, isolate the oral cavity from food intake (grade III mucositis);
- with swallowing problems and the risk of developing aspiration pneumonia;
- after operations on the larynx, esophagus (in this situation, a probe is also necessary for decompression).
Positive aspects of tube feeding:
- You will be able to take enough food regardless of your appetite and taste; as you know, during treatment, appetite is often reduced and taste sensations are distorted.
- Food will not irritate the oral mucosa and cause pain.
- Your condition will not be complicated by aspiration pneumonia.
- You will not lose weight or your strength.
- You will be able to continue treatment without interruption.
Remember that proper and sufficient nutrition reduces the number of treatment complications and allows you to complete radiation therapy as planned and feel well.
Nutrition options for a patient with a gastrostomy tube
The daily food intake should be 2.5 liters or more, depending on the patient’s condition and weight. The food for feeding the patient must be different - the diet must include fiber, protein and other beneficial substances.
There are 3 options in total:
- baby food;
- semi-liquid and pureed food;
- enteral mixtures.
Enteral nutrition
Enteral food refers to mixtures intended for administration through a gastrostomy tube into the gastrointestinal tract.
In pharmacy chains you can find ready-made mixtures for enteral nutrition:
- Nutrien;
- Nutricomp;
- Nutrilon.
The price for one serving of feeding is about 150 rubles. The advantages of the formula feeding algorithm are the natural composition and the correct ratio of minerals and vitamins.
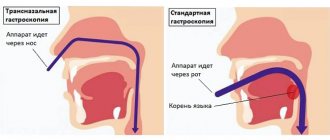
What is a nasogastric tube?
This is a tube made of a special non-toxic material. The end of the probe is smooth, sealed and rounded so as not to injure the mucous membrane, and there are round holes on the sides to facilitate the introduction of nutrition into the probe.
Probes come in different sizes, and the doctor selects the appropriate one for each patient. There are marks on the probe indicating its length; you can use them to control its location. The probe is installed for various periods - up to three weeks. If longer tube feeding is required, then percutaneous endoscopic gastrostomy is performed.
Gastrostomy feeding at home
In general, the technique of feeding at home does not differ from the above. Sometimes the patient is allowed to chew food on his own. After this, it is diluted in a glass with liquid and, already diluted, poured into a funnel. With this option, reflex excitation of gastric secretion is preserved.
After the procedure, the probe should be rinsed with warm water, and the patient should be given the opportunity to rinse his mouth. Therefore, in order to spit out water, it is necessary to provide an appropriate container. Caring for the gastrostomy tube after feeding also involves carrying out hygienic procedures so that no food particles remain in the tube and the hole itself. The funnel should be boiled in a soda solution (two percent) for 15-20 minutes. Then it needs to be dried and covered with a napkin.
How is a nasogastric tube placed?
This manipulation is performed by the attending physician or a doctor in the endoscopy department when there is a need for endoscopic control. The probe, under local anesthesia, is inserted through the nasal passage into the pharynx and slowly moves into the stomach, while the patient helps the doctor by making swallowing movements. When setting, there is no need to resist, as this brings even more discomfort.
In what cases is a gastrostomy tube placed?
Gastrostomy placement is indicated for the following conditions:
Permanent gastrostomy:
- Inoperable tumor of the pharynx or esophagus.
- Tumor of the mediastinum compressing the esophagus.
- Tumor of the inlet of the stomach.
- Cicatricial narrowings of the esophagus that cannot be bougienaged.
- Patients with damage to the nervous system whose swallowing reflex is impaired (patients with stroke, myasthenia gravis, amyotrophic lateral sclerosis, brain tumors).
A permanent gastrostomy can provide the patient with almost complete enteral nutrition, and for a long time. It can be classified as palliative surgery - it prolongs a person’s life without eliminating the underlying problem. The quality of life, of course, deteriorates, but mainly not because of the presence of gastrostomy, but because of the underlying disease.
Temporary gastrostomy:
- Chest wounds with damage to the esophagus.
- Severe maxillofacial injuries.
- Esophageal-tracheal or esophageal-bronchial fistula.
- Burns of the esophagus during healing and restoration of patency.
- In some cases, after extensive abdominal surgery (gastric resection, elimination of acute intestinal obstruction) for decompression and aspiration of gastric contents.
- For the period of preparation for operations on the esophagus or stomach in severely malnourished patients, if it is obvious that this period will be long enough.
Temporary gastrostomy allows you to provide adequate nutrition for a period of temporary inability to eat naturally. A temporary gastrostomy is formed in such a way that it can be removed in the future without repeated extensive surgery.
How will you feel?
Slight pain in the nasal cavity, pharynx and vomiting are possible, but not all patients experience this. It is important to listen to your doctor's commands and breathe properly through your mouth. Almost all patients tolerate both this manipulation and treatment with an installed probe satisfactorily. Don't worry, nasal breathing will continue. Sometimes it takes 2-3 days to get used to the probe. In extreme cases, the doctor may prescribe painkillers, antiemetics and antispasmodics. At first, you need to listen to yourself and understand what position you should be in in order to reduce discomfort in this area. The main thing is to remain calm and remember that this is a necessary and temporary measure. According to many patients, their fears about inserting a probe were greatly exaggerated.
Endoscopic gastrostomy
There is a technique for percutaneous endoscopic gastrostomy. The main condition for this is the patency of the esophagus so that an endoscopic tube can be inserted. This intervention does not require general anesthesia and is quite simple at first glance: a gastrostomy tube is inserted through a small puncture of the abdominal wall.
However, this operation is quite difficult for surgeons and requires honed skills. Performed by two surgeons.
- An endoscope is inserted through the esophagus into the stomach. Under visual control, the doctor selects an area on the anterior wall of the stomach that is most suitable for a puncture and presses the end of the endoscope into it.
- Another surgeon finds this place from the outside, palpating the abdominal wall. For better visualization, the lights in the operating room are turned off so that the illuminated end of the endoscope is visible.
- Local anesthesia is performed with a solution of novocaine or lidocaine.
- From the outside, the abdominal wall and the wall of the stomach are pierced with a trocar, and a conductor (thread) is inserted into its lumen. Using an endoscope, the thread is captured and removed through the mouth.
- A gastrostomy tube is attached to the end of the thread.
- Along the guidewire, the tube is inserted into the stomach.
- Using an endoscope, the correct installation is checked.
- The tube is fixed.
Features of nutrition through a gastrostomy tube
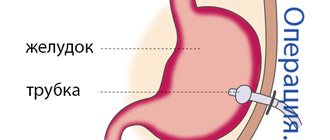
What is a gastrostomy?
Percutaneous gastrostomy is a special system for feeding through the anterior abdominal wall and an artificial entrance to the stomach cavity.
How is percutaneous endoscopic gastrostomy performed?
- The entire procedure is performed under anesthesia. At the first stage, esophagogastroduodenoscopy is performed to exclude pathologies of the upper gastrointestinal tract that prevent the installation of a gastrostomy tube.
- An endoscopist performing an examination of the stomach determines the most convenient place for installing a gastrostomy (the anterior wall of the lower third of the body of the stomach) and uses the endoscope to “illuminate” the place where the gastrostomy is installed on the skin.
- The assistant doctor, guided by endoscopic “illumination,” makes a small (about 7-9 mm) incision at the site of the planned installation of the gastrostomy tube and inserts a thin plastic pointed rod into the stomach.
- The rod inside has a channel through which a conductor is inserted into the lumen of the stomach. The endoscopist grabs the guidewire with forceps and, removing the endoscope, removes the thread from the stomach and esophagus into the patient’s oral cavity. The other end of the thread is held by a medical assistant.
- A gastrostomy tube is attached to the withdrawn part of the guidewire. The assistant doctor, by pulling the thread from the opposite end, ensures the movement of the gastrostomy tube through the esophagus into the stomach. In this case, the gastrostomy tube is brought to the surface of the skin and fixed to it with a plate, and the flat rubber part (cannula of the gastrostomy tube) is pressed tightly against the wall of the stomach from the inside. Thus, the anterior wall of the stomach is connected to the skin of the anterior abdominal wall, and water and nutritional mixtures can be injected directly into the lumen of the stomach through a plastic tube.
- This minimally invasive procedure lasts about one hour and is performed under constant endoscopic control in order to avoid complications.
- During the first 24 hours after the gastrostomy tube is installed, you should not administer nutritional mixtures or any other liquids through it.
How will you feel?
Minor pain is possible, which can be easily relieved with painkillers prescribed by your doctor.
Important: feeding through a gastrostomy tube can only be started after the permission of the attending physician. The amount of food and frequency of administration in the first days are discussed additionally!
How to care for a gastrostomy tube?
- Regularly change the sterile dressing placed around the incision site between the skin and the restraint. During the first week, dressings are performed daily, and then every other day. The area of skin around the stoma and the fixation device should be well dried. Every day, rotate the plastic probe 180 degrees around its axis and move it up and down 1.0-1.5 cm so that it does not stick to the walls of the stoma.
- Make sure that the external fixation disc is at least 5 mm from the surface of the skin. If you have gained or lost weight, it becomes necessary to loosen or tighten the fixation device.
- After each meal, rinse the gastrostomy tube with 20-40 ml of water. The tube must be washed every 8 hours, even if you did not administer nutritional formula through it. Clean with a damp cloth and then dry the skin around the stoma and the retainer to avoid infection. Ask your healthcare provider which skin disinfectant you should use.
- If your gastrostomy tube falls out, contact your doctor immediately.
What food can you eat?
Food can only be taken in liquid form (the consistency of cream) and without lumps, so that the tube does not become clogged. Remember that food should contain a sufficient amount of quality protein and healthy fats (butter and vegetable oil). Daily calorie content should be approximately 2000 kcal. The daily volume is divided into equal portions of 150-200-300 ml, administered every 2-3-4 hours and is approximately 2000 ml. The temperature of the food introduced should be approximately 40-45 degrees (with the exception of specialized mixtures that are consumed at room temperature).
Main courses: blended (carefully chopped) low-fat boiled vegetables, diluted with broth, meat, poultry; liquid mashed porridge with added butter.
You can use baby meat, vegetable and fruit food, diluting them to the appropriate consistency with cream or broth. Also use milk, fermented milk products, sour cream. Boiled eggs can also be crushed and added to food. You can use compotes, fruit drinks, and juices as drinks.
In our medical institution, a probe table will be prepared for you in the kitchen. If necessary, the attending physician will prescribe nutritional support in the form of ready-made specialized mixtures, and part of the daily diet can be replaced with them. You can also use your own blender and prepare the necessary mixtures yourself from the dishes offered for the common table. When taking diluted food, you do not need additional fluid intake if you are not thirsty, especially since after each meal you need to rinse the tube with 50-60 ml of warm water.
If you have a favorite food or drink (tea, coffee), then do not deny yourself the pleasure and add it to your diet.
What to eat?
You will be given two Janet syringes (150 ml), and now they will serve as utensils.
What do you need to prepare for meals?
You will need:
- the finished mixture, its temperature should be approximately 40 degrees;
- drinking water at room temperature or slightly warmer;
- 2 syringes Janet;
- 2 containers with a volume of 200 and 500 ml (glass, mug, glass);
- spoon;
- napkin;
- blender (optional, for advanced users).
Nutrition in the postoperative period
The first day after the installation of the HS, nutrition is administered intravenously. 24–48 hours after surgery, a small amount of saline is injected with a syringe to check the patency of the stoma and the tightness of the sutures. Then the patient is injected with a glucose solution, a decoction of dried fruits without sugar, and saline solution. The total volume of liquid entering through the GS should not exceed 1 liter, the amount of 1 serving is 50–100 ml.
If there is no reflux of stomach contents into the tube and its patency is maintained, approximately 500 ml of meat broth is injected on the 3rd day. In the first 5–7 days, feeding through a gastrostomy tube is carried out only with a syringe and is performed at the lowest speed possible.
During the rehabilitation period, in the absence of inflammatory phenomena and complaints from the patient, the amount of food administered is gradually increased to 1.5 liters, and the size of one serving is increased to 180–200 ml. Mashed porridge cooked in water is added to the diet.
The structure of a modern gastrostomy tube
There are many types of gastrostomy tubes. The main components that a tube should consist of for ease of use:
- The tube itself.
- Internal fixation block (usually a small container filled with liquid through a separate portal at the outer end of the tube).
- External fixation device.
- Anti-reflux valve.
- Clamp.
- Cork.
There are types of gastrostomy for active patients - they are practically invisible on the body and do not limit normal physical activity in any way.
Gastrostomy tubes are quite expensive (the minimum price starts from 50 euros). Therefore, in the absence of a special device as a gastrostomy, it is possible to install a conventional Foley catheter, which is designed according to the same principle.
The operation to create a gastrostomy is performed for medical reasons if feeding the patient in the usual way is difficult or impossible. A gastrostomy allows you to establish a person’s nutrition, bypassing the oral cavity and esophagus.
Of course, this way of eating is very different from the usual, natural eating. And a person after a gastrostomy needs to learn new hygienic skills: special care for the stoma and the skin around it.
The first 2-3 weeks after surgery, a fistula forms. At this time, it is necessary to treat the skin around the stoma with an antiseptic solution, such as Octenisept, and use bactericidal ointment dressings with povidone-iodine.
Before processing the gastrostomy, warn the patient about the upcoming manipulations and tell them what you are going to do. Calm and encourage.
Prepare for processing:
- scissors;
- antiseptic solution Octenisept;
- sterile bactericidal dressing PoviTex;
- fixing bandage, for example Barrier or Optimel Roll;
- Niltak spray for painless removal of the previous dressing.
Sequence of manipulations:
- Remove the previous bandage using Niltac spray to dissolve the adhesive layer.
- Treat the skin around the gastrostomy opening with Octenisept antiseptic solution.
- Carefully, holding the external fixation disk of the gastrostomy tube, rotate the tube 360 degrees. This is necessary for the correct formation of the fistula passage.
- Open the package of PoviTex bactericidal dressing. Without removing the protective layer, cut a piece of bandage measuring 5x5 cm and make a cut on it to the middle (in the form of panties).
- Remove the protective layer and apply a PoviTex dressing to the skin under the external fixation disk of the gastrostomy tube.
- Secure the bandage with a wide Optimel Roll plaster or Barrier postoperative bandage, making a similar incision on it.
IMPORTANT!:
- Do not apply a bandage over the retainer to avoid irritation and the formation of bedsores.
- Do not use alcohol solutions to treat gastrostomy tubes.
- At each treatment, inspect the skin around the gastrostomy tube. If signs of inflammation appear, consult a doctor.
- Don't take a bath for three weeks after your gastrostomy.
- Remember to wash your hands before eating/feeding.
- Nutrition is administered through a gastrostomy tube in liquid form. Fractionally, in small portions. Or using a special dispenser (as prescribed by a doctor).
- After feeding and after taking medications, rinse the gastrostomy tube with a small amount of warm boiled water.
- Make sure the skin around your stoma is clean and dry after every meal. If necessary, cleanse the skin with Tamu-Tamu hydrophilic oil and water.
- Do not leave the skin around the stoma wet to avoid maceration. Dry it with a soft cloth.
- Treat the skin under the fixative with Octenisept antiseptic solution or another alcohol-free antiseptic at least once a day.
- To protect your skin from moisture and pollution, use Silesse spray film.
- If skin irritation occurs, consult a doctor. To heal the skin, you can use Children's Tamu-Tamu cream containing zinc and Tamanu oil.