Malabsorption syndrome (MAS) is a symptom complex that occurs as a result of impaired absorption of nutrients, vitamins and microelements in the small intestine. Clinically manifested by diarrhea, weight loss, and signs of multivitamin deficiency.
Malabsorption syndrome is accompanied by more than 70 different diseases and syndromes.
Classification
According to etiology
- Primary (caused by congenital defects in the structure of the intestinal wall and enzymopathies).
- Secondary (develops against the background of various gastrointestinal diseases, with neuroendocrine disorders, while taking certain medications): Enterogenous (due to organic and functional intestinal disorders);
- Pancreatogenic (cancer, pancreatitis);
- Gastrogenic (atrophic gastritis, condition after gastrectomy, stomach cancer, gastrinoma);
- Hepatogenic (liver cirrhosis, cholestasis syndrome).
By the nature of the lesion
- Partial (selective) malabsorption (absorption of individual nutrients is impaired).
- Total malabsorption (absorption of all food components is impaired).
By severity
| Severity | Manifestations in adults | Manifestations in children |
| I (light) |
|
|
| II (medium-heavy) |
|
|
| III (severe) |
|
|
Malabsorption syndrome: clinical diagnosis and treatment
A.A. Sheptulin Department and clinic of propaedeutics of internal diseases, gastroenterology and hepatology (head of the department and director of the clinic - academician of the Russian Academy of Medical Sciences V.T. Ivashkin) MM A named after. I.M.Sechenova
Malabsorption syndrome is understood as a complex of disorders resulting from impaired absorption of nutrients. vitamins and microelements in the intestine. Currently, in a broad sense, this term also includes the syndrome of impaired digestion, since various disorders of food digestion processes that develop with this syndrome lead secondarily to disruption of absorption processes [1].
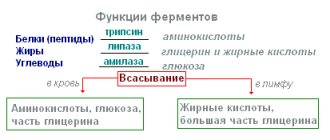
Etiology and pathogenesis Malabsorption syndrome can occur in many diseases: post-gastroresection syndrome, exocrine pancreatic insufficiency (in patients with chronic pancreatitis, cystic fibrosis and pancreatic cancer), diseases of the liver, biliary tract (most often in cases where they are accompanied by impaired bile secretion), with short bowel syndrome (after resection of the small intestine performed due to thrombosis and embolism of the mesepterial arteries, traumatic intestinal injuries, complicated forms of Crohn's disease), iptestinal fermentopathies (for example, lactase deficiency) [2]. A common cause of malabsorption syndrome is damage to the small intestine that develops in celiac disease. tropical sprue, Unplea disease, eosipophilic gastroenteritis, systemic mastocytosis, amyloidosis, immunodeficiency syndromes, lymphomas of the small intestine and radiation exposure. As part of the malabsorption syndrome, the so-called exudative enteropathy syndrome is often distinguished, which can occur with infectious and parasitic diseases of the intestine (for example, amebiasis, tuberculosis), lymphangiectasia of the intestine, and Mepetrier's disease. Zollipger-Ellison syndrome and other diseases. Disturbances in the absorption processes in the intestine are often observed with bacterial overgrowth syndrome, which can develop when passage through the small intestine is slowed down (after gastric resection according to Billroth I and intestinal resection with side-to-side or end-to-side anastomosis, the occurrence of postoperative adhesions in the intestine, interintestinal fistulas, the formation of intestinal strictures in patients with Crohn's disease, tumors of the intestine and mesepterial lymph nodes), due to retrograde reflux of the contents of the large intestine into the small intestine after resection of the ileocecal valve, with achlorhydria. The pathogenesis of diarrhea, which is the main factor leading to the development of malabsorption syndrome and its main clinical sign, may include various mechanisms [3]. Thus, the occurrence of diarrhea in disaccharidase deficiency is based on the accumulation of osmotically active particles (undigested carbohydrates) in the intestinal lumen. Impaired digestion and absorption of fats due to exocrine pancreatic insufficiency leads to the development of steatorrhea. In this case, undigested fats are hydroxylated in the lumen of the colon by bacteria, as a result of which the secretory activity of colopocytes is stimulated. In postgastroresection syndrome, diarrhea is caused by too rapid entry of osmotically active food components into the upper parts of the small intestine, as a result of which the processes of digestion and absorption are disrupted and steatorrhea develops. An additional pathogenetic factor in such cases may be bacterial overgrowth syndrome, which develops as a result of decreased secretion of hydrochloric acid. The occurrence of diarrhea in exudative enteropathy is explained by the release of high molecular weight plasma proteins into the intestinal lumen and their subsequent breakdown by intestinal microflora into osmotically active particles that bind water. Several links include the pathogenesis of diarrhea in short bowel syndrome. First, extensive resection of the small intestine causes malabsorption of carbohydrates and an increase in chyme osmolarity; in this case, fat absorption disorders lead to steatorrhea. Resection of the intestine also promotes hypersecretion of hydrochloric acid, as a result of which pancreatic enzymes are inactivated. Secondly, resection of the ileum causes a decrease in the absorption of bile acids and their increased entry into the lumen of the colon. A decrease in the epterohepatic circulation of bile acids aggravates steatorrhea, and the entry of free bile acids into the colon inhibits sodium absorption and stimulates chloride secretion, which also increases diarrhea. Finally, elimination of the occlusive mechanism of the ileocecal valve during ileal resection contributes to the occurrence of bacterial overgrowth syndrome. The pathogenesis of diarrhea in celiac disease is associated with a decrease in the total absorption surface of the small intestinal mucosa, resulting from lymphoplasmacytic infiltration of its lamina propria with subsequent villous atrophy and proliferation of crypt cells. Structural changes in the mucous membrane of the small intestine cause the occurrence of diarrhea and disturbances in absorption processes in diseases such as Unpl's disease, eotic gastroenteritis, systemic mastocytosis, intestinal amyloidosis, variable immunodeficiency syndrome, B- and T-cell lpmoma. radiation damage to the intestines.
Clinic Diarrhea in malabsorption syndrome is usually characterized by an increase in the volume of ciyvia (polyfecal matter), stool has a pasty or watery consistency, often acquires an unpleasant odor and, in the presence of steatorrhea, is poorly washed off the walls of the toilet. If the synthesis of bile acids is disrupted or their entry into the intestines is difficult (cholestasis), the stool becomes acholic and acquires an oily sheen. With lactase deficiency, diarrhea appears after consuming milk and dairy products and is accompanied by rumbling and cramping pain in the abdomen. Pain in the upper abdomen, radiating to the lumbar region or becoming encircling, accompanies diarrhea in the presence of chronic pancreatitis. From the editor
Clinical manifestations of malabsorption syndrome.
A common symptom encountered with malabsorption syndrome is weight loss due to insufficient intake of essential nutrients into the body. In children and adolescents (particularly those suffering from celiac disease), malabsorption syndrome leads to growth retardation and infantilism. A decrease in protein levels, especially pronounced in exudative enteropathy, causes the occurrence of edema. Poor absorption of iron and vitamin B12 causes the development of anemia. Patients with malabsorption syndrome often complain of general weakness, fatigue, and decreased performance. Many patients have clinical signs of deficiency of various vitamins (see figure): B1 (paresthesia), B2 (glossitis and ashular stomatitis), D (bone pain, tetany), K (increased bleeding), A (follicular hyperkeratosis, twilight disorders vision), nicotinic acid (pellagra), etc. With a long and severe course of malabsorption syndrome, cachexia progresses, symptoms of polyglandular insufficiency (adrenal glands, gonads), muscle atrophy, and mental disorders are added. Other clinical symptoms may also appear due to the characteristics of the disease that led to the occurrence of malabsorption syndrome. Thus, with Whipple's disease, joint pain, enlarged lymph nodes, damage to the lungs (bronchitis, pleurisy), heart (endocarditis, pericarditis) and central nervous system are noted. With systemic mastocytosis, headaches, tachycardia, and skin changes such as urticaria pigmentosa are observed. In immunodeficiency syndromes, a high incidence of infectious diseases of the upper respiratory tract is determined. With Zollinger-Ellison syndrome, persistent and often recurrent ulcers of the stomach and duodenum are noted. Intestinal lymphomas occur with fever, changes in the fingers in the form of drumsticks, hepato- and splenomegaly. In case of radiation damage to the intestine, manifestations of malabsorption syndrome are often combined with clinical signs of radiation proctitis (frequent stools in small portions, tenesmus, admixture of scarlet blood in the stool - hematochezia). Diagnosis and differential diagnosis Laboratory tests in patients with malabsorption syndrome often reveal a decrease in the content of albumin, cholesterol, iron, calcium, magnesium, vitamin A, and folic acid in the blood. Stool examination plays an important role in the diagnosis of malabsorption syndrome. First of all, the total mass of feces excreted by the patient during the day is determined. To do this, it is necessary to measure the daily amount of feces, collecting it (preferably in special plastic containers) for at least 3 days. Malabsorption syndrome is characterized by a significant mass of feces (usually more than 500 g per day), which decreases against the background of fasting (an important sign that allows us to exclude the secretory nature of diarrhea). In this case, attention is paid to the detection of muscle fibers (creatorrhoea), neutral fat (steatorrhea) and starch (amilorrhea) during microscopic examination of feces and the daily loss of fat in feces is determined. In a healthy person, 95% of fats are digested and absorbed, even with a very high content in the diet (150 g per day), so that normally no more than 7 g of fats are excreted in feces per day. Significant loss of fats in feces (more than 14 g per day) indicates severe exocrine pancreatic insufficiency. If there are digestion and absorption disorders in the small intestine, the pH of the stool may change. Thus, when the digestion of carbohydrates is impaired (for example, with disaccharidase deficiency), due to the activation of fermentation processes, the pH values shift to the acidic side (<6.0). The absorption function of the small intestine is assessed using the D-xylose test. The patient takes 25 g of D-xylose, after which he collects urine for 5 hours. At a normal level of absorption in the small intestine, the amount of D-xylose released during this time should be at least 5 g. The 75Se-homotaurocholic acid test detects a decrease in the absorption of bile acids in the terminal ileum and helps in the diagnosis of so-called hologenic diarrhea. Increased loss of protein through the intestines (in Whipple's disease, malignant lymphoma, radiation enteropathy) is detected when using a test with 51cr-albumin. The Schilling test is used to assess vitamin B12 absorption. Normally, after taking labeled vitamin B12, its excretion in urine during the day is at least 10%. Indicators of daily excretion of vitamin B12 in urine below 5% indicate a violation of its absorption in the small intestine. Accurate data on the processes of absorption in the small intestine can be obtained using its perfusion study. In this case, a probe is inserted into the jejunum, through which perfusion is carried out with solutions with known concentrations of Na, SG and other substances. Calculations carried out after repeated measurements of the concentration of these electrolytes in the distal parts of the small intestine allow us to draw a conclusion about the nature of the absorption processes. If malabsorption syndrome is suspected, an x-ray examination of the small intestine is performed, revealing its typical signs (fragmentation of a barium sulfate suspension column, thickening and coarsening of the folds of the mucous membrane), and sometimes helping to recognize the diseases that caused its development (blind loops of the small intestine, interintestinal anastomoses, multiple diverticula, small intestinal lymphoma, intestinal pseudo-obstruction syndrome in systemic scleroderma, signs of nodular lymphoid hyperplasia in common variable immunodeficiency syndrome, etc.). Endoscopic examination of the small intestine with a biopsy from its proximal parts and subsequent histological and histochemical examination makes it possible to diagnose diseases such as Whipple's disease, small intestinal lymphoma, eosinophilic gastroenteritis, celiac disease, tropical sprue, systemic mastocytosis, amyloidosis. The H2 breath test performed with lactulose or glucose is currently used to diagnose bacterial overgrowth syndrome. The principle of the method is based on the fact that bacteria can ferment lactulose. As a result, H2 is released, the concentration of which can then be measured in the exhaled air. Normally, lactulose is broken down only in the colon. The early appearance of H2 in exhaled air indicates bacterial breakdown of the substrate in the small intestine. The diagnosis of bacterial overgrowth syndrome is also confirmed by culture of duodenal aspirate and subsequent detection of an increased content of microortnisms in it (106/ml). To diagnose the underlying disease that caused the development of malabsorption syndrome, additional research methods are used. Thus, if exocrine pancreatic insufficiency is suspected, in addition to determining the daily loss of fat in feces, a secretin-pancreozymin test, the Lund test, is performed. pancrysolauryl test and p-aminobasic acid test (NBT-PABA-tsst), evaluate the content of chnmotrypsin and elastase-1 in the stool. Characteristic signs of pancreatitis are detected by ultrasound examination of the abdominal organs and endoscopic retrograde cholangiopancreatography. To recognize lactase deficiency, an additional lactose load test is performed. The patient takes a dose of 50 g of lactose, after which the glucose level is determined. The occurrence of dyspeptic disorders, as well as the absence of an increase in blood glucose after a lactose load, confirms the diagnosis of lactase deficiency. A specific diagnostic test for detecting celiac disease is an increase in the titer of antibodies to gliadin. If systemic mastocytosis is suspected, the level of gnstamamine in the blood and the secretion of its metabolites in the urine are determined. The diagnosis of variable unclassified immunodeficiency is confirmed when a pronounced decrease in the level of immunoglobulins of all classes is detected. Identification of the specific disease that caused the malabsorption syndrome allows for more differentiated therapy.
Treatment The treatment of malabsorption syndrome is based on two basic principles: influencing the course of the underlying disease that contributed to the development of this syndrome (I), and correcting disturbances in the processes of impaired absorption in the intestine (I) [1].
The implementation of the first principle plays, in particular, an important role in the treatment of patients with celiac disease. Eliminating products made from wheat and rye flour, semolina and barley and replacing them with iodukgs made from rice and corn can significantly improve the condition of patients and even achieve their complete recovery. The exclusion of milk and a number of dairy products helps to stop diarrhea in patients with lactase deficiency. Long-term antibiotic therapy leads to the cessation of diarrhea in patients with Whipple's disease. Timely surgical treatment, carried out when detecting interstitial fistulas and large diverticula, which caused the development of bacterial overgrowth syndrome, eliminates intestinal absorption disorders in such patients. The second principle of treatment includes compliance with certain dietary recommendations, prescription of replacement therapy, as well as drugs that normalize impaired intestinal functions [4, 5]. Patients with malabsorption syndrome are advised to eat a high protein diet (up to 1,130 g per day). On the contrary, the fat content in the diet of patients (especially in the presence of steatorrhea) should be reduced by approximately 50% compared to normal. Instead, medium-chain triglycerides are recommended, which are more easily digested by pancreatic lipase and absorbed without the formation of micelles. In patients with low levels of protein in the blood, a good effect can be obtained by prescribing them special mixtures for enteral nutrition (portagen, nzocal, etc.), containing all the necessary nutrients. including vitamins and microelements. For more complete absorption, these mixtures are best administered dropwise into the stomach through a tube. In severe cases, patients are transferred to parenteral nutrition with the introduction of 20-40", glucose solutions, 10-20% fat emulsions, 5-10'% L-amino acid mixtures, electrolyte solutions containing potassium, sodium, magnesium, calcium and phosphorus salts , as well as microelements. Replacement therapy with vitamins A, D, E, K, B12, folic acid and iron supplements is carried out. In cases where malabsorption syndrome occurs with severe steatorrhea and digestion, enzyme preparations are prescribed to improve cavity digestion. When choosing specific drugs, you should pay attention not only to the need for a high lipase content in their composition, but also to their release form. Currently, enzyme preparations are recommended in which the lyophilized extract of pancreatin (obtained mainly from the pancreas of the pancreas) is enclosed in special microspheres (pellets). resistant to gastric juice. The latter, in turn, must be in a capsule coated with gelatin. These capsules quickly dissolve in the gastric contents. after which the microspheres. mixing with chyme and not being exposed to gastric juice, they enter the lumen of the duodenum. where at pH 5.5 the drug is released from the microsphere. The daily dose of drugs (in terms of lipase content) should be 000-150,000 units. If patients with malapsorption syndrome experience accelerated transit of contents through the intestines. Drugs that weaken intestinal motility may be used. Loieramide is usually prescribed at a dose of 2 mg per dose. The total daily dose of the drug is determined by the frequency of stools. For patients in whom malabsorption syndrome occurs against the background of initially weakened intestinal motility and intestinal stasis (with diabetic entropathy, systemic scleroderma, amyloidosis), the use of lopsramnd is contraindicated. In severe cases, synthetic analogues of somatostatip octrsotpd are used to relieve diarrhea. which inhibits intestinal motility, improves absorption and inhibits intestinal secretion. Octreotide is prescribed at a dose of 100-250 mcg 1 time per day. For symptomatic purposes, astringents and enveloping agents (smecta, attapulgt, etc.) can be used. Literature 1.Kiley SA. Marsh L AY. Maldigestion and malahsorhtiou//Sleisenger &• Fordtran'sgastrointestinal and lirer disease (lid. l-eldman M. el al). 6tbed., 1998;2: 1501-22. 2. Ivashkin BJ-1., SheptulinAA. (.'ipd/yum diarrhea. L/., 2000; 1.15. 3- Kare/pers DM. Ma'1absorbi111Ya//Papyufpzi<). Chogia of the digestive organs (edited by D.M.Hendersoia).M.-SG1o. 1997: 121-64-4-Belousova EA., Zlatkina AR. Absorption syndrome (pathophysiology, poultry, treatment). A manual for practitioners. M, 1998; 28. 5. Loginov AS Parfenov AL. Intestinal diseases. M., 2000: 632. (Visited 227 times, 1 visits today)
Causes
Malabsorption syndrome develops due to:
- impaired absorption of one or more nutrients by the mucous membrane of the small intestine;
- disturbances in the breakdown of proteins, fats and carbohydrates due to insufficiency of digestive enzymes.
The first group of reasons include:
- malabsorption of certain amino acids (Hartnap disease, Lowe's syndrome, cystinuria);
- impaired absorption of monosaccharides (glucose, galactose, fructose), fatty acids (abetalipoproteinemia);
- disturbances in the absorption of vitamins (folic acid, vitamin B12);
- disorders of mineral absorption (familial hypophosphatemic rickets, primary hypomagnesemia);
- damage to the mucous membrane of the small intestine (infectious and non-infectious enteritis, enterocolitis, Crohn's disease, tuberculosis, intestinal amyloidosis, diverticulosis, Whipple's disease);
- some other diseases and conditions with malabsorption (systemic pathology, tumors, post-resection syndromes, blood diseases).
Be sure to read: What is traveler's diarrhea, how does it manifest and how is it treated?
The second group of reasons includes:
- congenital enzymopathies (celiac disease, enterokinase deficiency, disaccharidases deficiency - lactase, isomaltase, sucrase);
- diseases of the pancreas (tumors, pancreatitis);
- liver diseases (cirrhosis, chronic hepatitis);
- stomach diseases (cancer, atrophic gastritis);
- diseases of the small intestine (Crohn's disease, Whipple's disease, resection of the small intestine, amyloidosis);
- taking certain medications (cytostatics, antibiotics, laxatives, glucocorticosteroids).
Treatment of malabsorption
Malabsorption syndrome is a disorder that requires an integrated approach.
The main principles of treatment are the following:
- elimination of the underlying pathology against which this condition arose;
- diet;
- taking enzyme agents to improve digestion;
- restoration of normal intestinal microflora;
- normalization of motor function, elimination of diarrhea;
- restoration of the intestinal mucosa;
- elimination of metabolic disorders, lack of vitamins and microelements.
Drugs
The main types of medicines used to treat diseases of this group are listed in the table below.
| Drug name | Dosage per day | Duration of treatment |
| Restoring deficiency of vitamins and microelements | ||
| Vitamin B 12 (cyanocobalamin solution) | 30-100 mcg | 10-15 days |
| Nicotinamide (nicotinic acid), intramuscular | 0.5-3 ml | 5-10 days |
| Ferrum Lek for iron deficiency anemia | The first days - 2 ml intramuscularly, then long-term use of 1-3 tablets for adults and children over 12 years old, children 1-12 years old - 5-10 ml of syrup, younger children - 2.5-5 ml of syrup. | 3-5 months |
| Folic acid | Adults – 5 mg, children – 1 mg | 20-30 days |
| Calcium gluconate | 1-3 g 2-3 times | 2-3 months or more with monthly monitoring of calcium levels in the blood. |
| Antimicrobials | ||
| Rifaximin (Alpha Normix) | For adults and children over 12 years of age – 400 mg every 8-12 hours. | 7 days |
| Metronidazole | Adults and children over 12 years of age – 250 mg 2 times. Children under 12 years of age – 5-16.7 mg per 1 kg of body weight 3 times. | Determined individually, on average 10 days. |
| Antisecretory and antidiarrheal agents | ||
| Octreotide (Sandostatin), subcutaneous | Adults – 50-500 mcg 2 times, children – 1-10 mcg per 1 kg of weight. | 5 days |
| Loperamide (Imodium, Lopedium) | Adults – 1 tablet after each episode of diarrhea, but not more than 6 tablets. Children over 5 years old – 2 mg 2 times. | 3-5 days |
| Pancreatic enzymes | ||
| Creon | Adults – 150 thousand units. Children – 50-100 thousand units. | Up to several months |
| Mezim forte | Adults – 2-4 tablets with each meal. Children – 500-1000 units. per 1 kg of weight with each meal. | |
Diet therapy
The basic principles of nutrition for this syndrome are as follows:
- therapeutic nutrition – table No. 4 according to Pevzner;
- increased protein content (up to 150 g per day);
- limiting carbohydrates to 250 g per day;
- reduction in the amount of fat by 50%;
- consumption of specialized products with combinations of nutrients (Nutricomp, Nutrigen, Nutrinidrink, for children - “Maloezhka” and others);
- small meals, at least 5-6 times a day;
- consumption of foods rich in tannin (for diarrhea), as well as viscous consistency (mucoid soups, porridges, jelly).
ethnoscience
In folk medicine, the following recipes are used for nutrient malabsorption and diarrhea:
- Pour 250 ml of clean water into a small saucepan, add 1 tbsp. l. oak bark and place on the stove over medium heat, stirring occasionally. After boiling, turn off the heat, cool, strain through cheesecloth. Drink 1 glass 3 times a day until diarrhea completely stops.
- 1 tsp. crushed pomegranate peels pour 1 tbsp. boiling water, keep in a water bath for 15 minutes. Then leave for 30 minutes, drink 1 tsp. 3 times a day.
- 5 tbsp. l. dried blueberries, pour 1 liter of boiling water, leave for 2 hours, then strain. You can drink it in any quantity like tea.
- Boil 0.5 l in a saucepan, add 2 tsp. rice, cook for 1 hour. Then remove from heat and strain. Drink half a glass every hour.
Surgical intervention
Surgical treatment is indicated in the following cases:
- Crohn's disease;
- ulcerative colitis in a complicated form;
- malignant tumors;
- diverticulosis;
- liver pathologies;
- lymphangiectasia.
Features of treatment for children
In children, this disorder is almost always accompanied by severe pain. Therefore, their treatment requires the use of anticholinergic drugs (Riabal, Drotaverine, No-Shpa).
For newborns with various forms of malabsorption, special baby food (milk formula and cereal) has been developed.
Pancreatic enzyme preparations are recommended to be taken in the form of microgranules (for newborns) or gelatin capsules (for older children). Their dosage is selected individually, depending on the degree of lipase deficiency. If there is no effect from their use (which may be due to increased stomach acidity), it is necessary to prescribe medications that inhibit hydrochloric acid.
Symptoms
Clinical manifestations of malabsorption syndrome can be divided into local and general.
Local symptoms
Diarrhea with polyfecal matter
The frequency of stools is 4-20 times a day.
The volume of feces increases to 300 g/day) or more. The consistency of the stool is pasty or liquid, the color is light yellow or greenish, there are pathological inclusions in the form of undigested pieces of food, muscle fibers, and often the stool has a strong unpleasant odor. If the digestion of fats is impaired, the stool becomes sticky, shiny, difficult to wash off, and sometimes droplets of fat are visible in it (steatorrhea).
When fermentation processes are activated, feces become foamy, and the reaction shifts to the acidic side.
Patients often note a very violent urge to defecate, occurring immediately after eating, and the process of defecation itself may be accompanied by severe weakness, hypotension, and palpitations.
Abdominal pain
Pain is usually localized in the right iliac or periumbilical regions. The nature of the pain can be paroxysmal or constant.
Intestinal discomfort (flatulence, rumbling, flatulence)
Symptoms increase in the afternoon and disappear after passing gas and defecation. With flatulence, patients note a noticeable increase in abdominal volume, difficulty breathing, palpitations, pain in the heart area.
General symptoms
Common symptoms are caused by metabolic disorders and include
Weight loss (in children – growth retardation and infantilism)
Rapid weight loss is caused by impaired absorption of proteins and fats. Loss of body weight is accompanied by weakness and fatigue. Due to impaired protein absorption, muscle strength decreases sharply and muscle atrophy occurs. Significant protein deficiency causes the development of edema.
In children, malabsorption is manifested by severe retardation in growth, physical and sexual development.
General anemic and sideropenic syndromes
- iron deficiency microcytic anemia (due to iron deficiency);
- macrocytic anemia (due to vitamin B12 deficiency);
- dry skin, hair;
- perversion of taste and smell;
- difficulty swallowing due to atrophy of the esophageal mucosa;
- changes in nails (brittleness, lack of shine, spoon-shaped deformation of the nail plate);
- fragility and hair loss;
- atrophic gastritis.
Mineral metabolism disorder
- hypocalcemia - cramps in the limbs and trunk, bone pain, pathological fractures.
- metabolic disorders of potassium, sodium, chlorine, magnesium, phosphorus, etc. (weakness, decreased muscle tone, nausea, vomiting, heart rhythm disturbances, decreased blood pressure).
Hypovitaminosis
- vitamin A deficiency – impaired twilight vision, dry skin;
- deficiency of vitamin B12 and B9—macrocytic anemia, atrophic gastritis, damage to the nervous system;
- vitamin C deficiency - skin hemorrhages, bleeding gums, frequent nosebleeds, general weakness;
- vitamin B1 deficiency - peripheral polyneuropathy (decreased sensitivity in the distal extremities, paresthesia, numbness of the legs);
- vitamin PP deficiency - pigmentation of exposed skin, dermatitis, atrophy of the tongue papillae, taste disturbance;
- deficiency of vitamin B2 – “stubs” in the corners of the mouth, glossitis;
- vitamin K deficiency - hypoprothrombinemia, increased bleeding.
Be sure to read:
Intestinal colic in a child: symptoms and treatment (first aid, medications, nutrition)
Endocrine disorders
Occurs against the background of severe malabsorption syndrome:
- adrenal insufficiency – severe weakness, pigmentation of the skin and mucous membranes, hypotension.
- dysfunction of the gonads - decreased potency, testicular atrophy in men; hypo- or amenorrhea in women.
- hypothyroidism (if iodine absorption is impaired) - facial pastiness, chilliness, bradycardia, constipation, drowsiness, memory loss, hair loss, dry skin.
Clinical manifestations and symptoms of malabsorption syndrome
The following are typical nonspecific symptoms (that is, those that are also observed in other diseases):
- weight loss (especially with celiac disease);
- general weakness;
- increased fatigue;
- bloating, flatulence;
- abdominal pain (sometimes radiating to the lower back or shingles);
- diarrhea;
- dry skin, hair loss;
- feeling of fullness in the stomach;
- impotence;
- menstrual irregularities.
In adults
Specific symptoms in adults are:
- swelling of the legs and feet;
- ascites (dropsy);
- changes in the skin, tongue, mucous membranes;
- stomatitis, seizures in the corners of the lips, inflammation of the tongue;
- pigment spots on the skin, peeling nails, thin and falling hair.
Malabsorption syndrome is a disease accompanied by hypovitaminosis.
If there is a deficiency of vitamins and microelements, the following signs are observed:
- vitamin A – weakening of visual acuity at dusk;
- vitamin B12 – symptoms of megaloblastic anemia (yellowish skin color, bright red, varnished tongue; nervous disorders);
- vitamins B1 and E – burning sensation, tingling, crawling, numbness, cramps, pain in the legs;
- calcium – numbness, cramps, pain in muscles and bones, increased fragility of the latter;
- copper, zinc, iron – skin rash, fever.
In children
In young children, the disease may manifest itself as a deterioration of the condition (diarrhea, abdominal pain, flatulence) due to dietary changes (introduction of complementary foods, new foods):
- lactase deficiency – after consuming dairy products (especially whole milk);
- sucrase deficiency – sweetened foods, juices;
- glucose-galactose deficiency - after milk, sugar-containing products;
- celiac disease - after the introduction of semolina, oatmeal (possible delay in the onset of symptoms for 1-2 months);
- enteropathic dermatitis - a sharp reduction in body weight gain, greasy and liquid feces, hair loss after breastfeeding;
- secondary forms of the disease – persistence of diarrhea after infectious and inflammatory pathologies.
- irritable bowel syndrome – alternating constipation and diarrhea after stressful situations;
- pancreatic enzyme deficiency - after fatty foods.
Diagnostic algorithm for SM
Malabsorption syndrome can be assumed in patients with chronic diarrhea, anemia, and rapid weight loss. If such symptoms occur, you should consult a physician/pediatrician or gastroenterologist.
Mandatory examination methods
- General blood analysis. Signs of microcytic or megaloblastic anemia.
- Blood chemistry. Changes in levels of total protein, albumin, glucose, triglycerides, cholesterol, calcium, zinc, magnesium, etc.)
- Scatological research. Straw-yellow or greenish color of stool, pH less than 5.5, appearance - foamy, shiny, smell - sour, putrid, steatorrhea, creatorrhoea, amilorrhea.
- D-xylose test to assess the absorption capacity of the small intestine. In case of malabsorption syndrome, the amount of D-xylose excreted in the urine is less than 5 g.
- Endoscopic research methods (FGDS, colonoscopy, intestinoscopy) with tissue biopsy from the proximal small intestine, terminal ileum. Allows diagnosis of Crohn's disease, celiac disease, eosinophilic gastroenteritis, Whipple's disease.
- X-ray examination of the small intestine using a suspension of barium sulfate. Characteristic radiological signs of malabsorption are expansion of the jejunum and a decrease in its tone, the “cast” symptom - straightening and smoothing of the walls of the jejunum, slowing down the passage of barium sulfate through the small intestine, shortening and flattening of the folds of the mucous membrane of the small intestine with an increase in the distance between them. In addition, fluoroscopy of the intestine makes it possible to identify diseases that caused the development of this syndrome (interintestinal anastomoses, diverticulosis, lymphoma).
Additional research methods
They are carried out depending on the suspected disease that caused the malabsorption syndrome:
- determination of blood levels of vitamin B12, folic acid, iron, ferritin, Schilling test;
- determination of the level of thyroid hormones, cortisol, sex hormones;
- ERCP (for diagnosing diseases of the pancreas and biliary tract);
- Ultrasound of the abdominal organs;
- , MRI (for diagnosing tumor and inflammatory processes in the abdominal cavity);
- immunological studies for the diagnosis of celiac disease, IBD;
- serological tests for the diagnosis of infectious and parasitic enteritis.
Malabsorption - diagnosis
To diagnose malabsorption syndrome, your doctor will ask about your symptoms. He may order various diagnostic tests to rule out or confirm the diagnosis.
Tests include:
Blood analysis
The doctor will ask for a complete blood count as well as electrolyte levels. Checking your blood protein levels will help you understand if and to what extent a person is malnourished.
Stool analysis
A stool test can help determine if there is fat in your stool. High fat levels may mean that fat is not being absorbed in the intestines.
Breath tests
Breath tests will check for the presence of hydrogen gas in people with lactose intolerance. Excess hydrogen is produced in the intestines if lactose is not absorbed.
Visualization
Sometimes your doctor may check the functions and structures of your digestive organs. Your doctor may also recommend an esophagogastroduodenoscopy or colonoscopy to examine the intestinal lining and take tissue biopsies to diagnose certain conditions.
Treatment
Adequate treatment of malabsorption syndrome is possible only after identifying the cause of impaired absorption. At the same time, treatment of the underlying disease significantly improves the processes of digestion and absorption in the intestine.
Be sure to read:
Intestinal infection: symptoms and treatment methods (diet, medications)
Treatment of malabsorption syndrome involves:
- prescribing an appropriate diet;
- correction of protein metabolism disorders;
- correction of electrolyte disturbances;
- vitamin replacement therapy;
- symptomatic treatment.
Diet
General nutritional provisions
Considering that the main manifestation of diseases occurring with malabsorption syndrome is diarrhea, nutrition should be aimed at reducing intestinal motor activity:
- chemical and mechanical sparing of the gastrointestinal mucosa;
- exclusion of products that enhance the processes of fermentation and putrefaction in the intestines;
- exclusion of foods rich in essential oils (radish, onion, garlic, radish, sorrel, mushrooms);
- use of products rich in tannin.
Recommended: dried bread, unpalatable dry biscuits, slimy soups with low-fat meat and fish broth, dishes made from lean meats, steamed or boiled, porridges (except pearl barley and porridge) with the addition of a small amount of milk, pureed vegetables and casseroles, fruit jelly, jellies, compotes, tea, cranberry, blueberry, apple juices, cottage cheese, fermented milk products.
The diet is modified depending on the underlying disease and the severity of the inflammatory process. Patients with severe malabsorption syndrome are advised to eat a high protein diet and limit fat intake.
Enteral nutrition
In case of significant digestive disorders, special depolymerized enteral mixtures are used as a supplement to the diet or as the main diet.
In more severe cases, synthetic mixtures are used, which are completely absorbed in the proximal small intestine. They consist of free amino acids, oligopeptides, polyunsaturated fatty acids, glucose polymers, vitamin and mineral complexes.
Parenteral nutrition
Parenteral nutrition is used to treat severe malabsorption syndrome. Intravenous infusions of glucose solution, mixtures of amino acids, and fat emulsions are performed.
Drug treatment
- replacement therapy with vitamins and minerals (cyanocobalamin, nicotinamide, calcium gluconate, Ferrum Lek);
- antibacterial therapy (used to treat infectious enteritis, Crohn's disease, etc.);
- hormonal therapy (used to treat celiac disease, systemic diseases);
- choleretic drugs and enzymes are used for pathologies of the liver and pancreas;
- antidiarrheal drugs (sandostatin, loperamide);
- antispasmodics – for pain syndrome (duspatalin, spasmomen).
In continuation of the topic, be sure to read:
- Causes of bloating and increased gas formation, treatment methods
- Rectal cancer: symptoms, stages, treatment and prognosis for life
- Rectal fissure: causes, symptoms and treatment of pathology
- More about hemorrhoids: causes, symptoms and treatment methods
- Details about bowel cancer: stages, symptoms, treatment and prognosis
- Sigmoiditis (inflammation of the sigmoid colon): symptoms and treatment methods
- Intestinal disorder and methods of its treatment: diet and medications
- Intestinal dyskinesia: types, causes, symptoms and treatment methods
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Dumping syndrome: definition, causes and treatment of pathology
Diet for malabsorption syndrome
In the stage of severe dyspeptic disorders with a predominance of diarrheal type, a gentle diet with a low fat content or fasting for 2 days is indicated. Avoid dairy products, spicy, fried, fatty foods.
Then:
The diet begins to include boiled dishes, soups, cereals without milk, and vegetables in small quantities. Fruits are not recommended. After stable normalization of stool, a high-protein diet with a balanced diet and replenishment of indigestible elements is prescribed.
Optimal high-protein dishes are chicken breast, veal, legumes. If the diet does not achieve the required amount of protein and its concentration in the blood decreases noticeably, then transfusion of pure amino acids is indicated.
If this is not enough, then they resort to the procedure of blood plasma transfusion. These manipulations can only be performed in a hospital under the supervision of the attending physician.
Depending on the form, vitamins, saline solutions, and those containing micro- and macroelements must be administered intravenously or intramuscularly. Among the saline solutions used are saline solution in different percentages, Trisol, Chlosol, Ringer's solution.
To maintain potassium, sodium and calcium, their chlorides are used. These drugs are prescribed under the control of a biochemical blood test and heart rhythm.