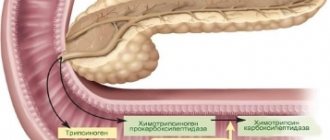
A pathological disorder of the functionality of the pancreas of an inflammatory nature can have both an edematous form of development and a necrotic one. The most popular is acute edematous pancreatitis. Pancreatic edema is a rather dangerous sign, with a high risk of developing an abscess, and in which the ducts are filled with an impressive amount of epithelial exfoliated cellular structures and leukocytes. Remember: swelling of the pancreas creates all the conditions for all breakdown products to enter the blood plasma and contribute to intoxication of the entire body.
Causes
In 90% of cases, this pathology develops against the background of alcohol abuse. Ethyl alcohol has a toxic effect on the organ, enhancing the production of enzymes. The latter begin to digest the gland, which causes tissue swelling. Other common causes of pancreatitis are:
- hyperparathyroidism (excessive production of parathyroid hormone by the parathyroid glands);
- cholelithiasis;
- cholecystitis;
- irrational use of medications (tetracyclines, estrogens, systemic corticosteroids, thiazide diuretics);
- operations;
- injuries (bruises);
- mumps (viral infection of the salivary glands);
- enterovirus infection;
- infection of the body with mycobacteria and campylobacteria;
- developmental anomalies;
- cystic fibrosis (damage to the exocrine glands);
- hepatitis (liver damage);
- combined infectious inflammation of the stomach and small intestine;
- circulatory disorders;
- high levels of calcium in the blood;
- errors in nutrition (violation of the regime, excess of spicy, fatty and fried foods in the menu, overeating);
- smoking.
Pancreatitis may be a consequence of toxic substances.
Edema and diseases of the pancreas
As a rule, swelling of the pancreas is the result of improper activity of the digestive enzymes that it produces. Impaired functioning most often causes a primary disease. The most common are:
- cholelithiasis (occurs very quickly);
- alcohol abuse (long process).
Acute pancreatitis can be caused by other diseases:
- diabetes;
- damage to the pancreas due to injury or surgery;
- infectious diseases;
- blocked ducts;
- malignant tumors.
Symptoms
If a person has developed an edematous form of inflammation of the pancreas, then the following signs are possible:
- Pain. Intense and constant. It is felt in the hypochondrium on the left, right, or encircles. Lasts several hours or days. Does not disappear when using antacids. Radiates to the shoulder, back and shoulder blade on the left. Dull or cutting.
- Increased body temperature. It is a response to the penetration of microbes. The temperature rises to +38…+39ºC. Indicates that the body is intoxicated.
- Chills.
- Lack of appetite. The reason is insufficient supply of enzymes to the duodenum and, as a result, difficulty in digesting food.
- Vomit. It can be indomitable. Vomit contains bile. Does not bring relief to a sick person.
- Frequent heartbeat. Pulse exceeds 80 beats/min.
- Skin that is cold and damp to the touch.
- Jaundice color of the skin and sclera of the eyes.
- Reduced blood pressure. Severe hypotension indicates fluid loss and shock.
- Frequent, loose stools. Occurs as a result of stagnation of enzymes in the organ.
- Bluish spots in the face, neck or navel.
- Muscle tension on the left side.
- Feeling of abdominal distension.
- Bloating.
- Belching.
- Hiccups.
- Dry mouth.
- Dyspnea. It results from loss of electrolytes through repeated vomiting.
- Weakness.
- Headache.
With pancreatitis, not all of the listed symptoms may be present.
Diagnostics
If you have pain, you need to go to the hospital. Will help in making a diagnosis:
- collection of anamnesis of illness and life;
- physical examination (tapping, palpation and auscultation);
- visual inspection;
- Ultrasound;
- radiography;
- computed tomography or magnetic resonance imaging;
- diagnostic laparoscopy (examination of the abdominal organs).
Ultrasound in the acute form of pancreatitis reveals an enlargement of the gland or its individual parts (tail, head, body), heterogeneity of structure, uneven contours, accumulation of fluid in the abdominal cavity and around the pancreas.
Analyzes
If you suspect acute pancreatitis you will need:
- general and biochemical blood tests;
- general and biochemical urine tests;
- stool examination;
- ionogram.
With pancreatitis, leukocytes, amylase, lipase, C-reactive protein, glucose, urea increase in the blood, and ESR also increases. During an acute inflammatory process, the following decreases: total protein, hematocrit, albumin, globulins, concentration of magnesium, calcium and potassium. In acute pancreatitis, the amylase content in the urine increases.
Differential diagnosis is carried out with other pathologies of the digestive organs (cholecystitis, peptic ulcers, colitis, Crohn's disease, appendicitis), as well as diseases of the genital organs.
Treatment
Treatment for acute pancreatitis is complex. It begins after consultation with a gastroenterologist. Therapy is aimed at relieving edema, normalizing the outflow of pancreatic juice and bile, eliminating symptoms and preventing complications (pancreatic necrosis, abscesses, cysts).
Basic principles of drug therapy
For acute pancreatitis, the following medications are used:
- Antispasmodics (No-shpa, Drotaverine). These drugs eliminate pain by relaxing the muscles of the organ wall.
- Anesthetics (Novocaine). They are used during blockades in the presence of severe pain.
- Proton pump inhibitors (Omez, Pariet). They block the substance responsible for the formation of hydrochloric acid.
- Antacids (Gaviscon, Phosphalugel).
- Saline and protein solutions.
- Antibiotics. Prescribed by injection or in tablet form. The drugs of choice are cephalosporins, carbapenems, fluoroquinolones and penicillins.
- Analgesics (Tramadol, Analgin-Ultra).
- Proteinase deactivators (Aprotex).
- Diuretics (Lasix).
- Plasma replacement and perfusion solutions (Reopoliglyukin);
- Antipyretics (Panadol, Efferalgan). Indicated for fever above 38ºC.
When gallstones are detected, medications are used to dissolve them. After pain relief, enzymes (Pangrol, Festal, Creon) are often prescribed.
They are contraindicated in the acute stage of the disease. In case of acidosis (pH shift to the acidic side), treatment with alkaline solutions is possible.
We recommend reading: What is hemorrhagic pancreatitis?
Traditional medicine methods
Traditional medicine cannot replace hospital treatment. Their inept use can cause harm and cause complications. They are used with the permission of a gastroenterologist. For acute pancreatitis, the following can be used:
- infusion based on yarrow, immortelle, calendula, chamomile, string, St. John's wort and sage;
- decoction of barberry bark;
- decoction of golden mustache;
- propolis;
- cranberries mashed with honey;
- beans;
- oatmeal jelly;
- fresh potato juice;
- sauerkraut brine.
Traditional medicine cannot replace hospital treatment.
You can prepare an infusion based on elecampane, mint and string. To do this, you need to take 1 tsp of dried herbs. and pour the mixture with 400 ml of boiling water. The infusion takes 3-4 minutes to prepare. This product should be taken 1/3 cup 2 times a day before meals after preliminary filtration.
Consuming compote for pancreatitis has a beneficial effect on the pancreas.
Surgical
After hospitalization of a person with acute pancreatitis, the doctor may raise the question of surgical intervention. The most frequently performed types of operations are:
- removal of stones;
- drainage (removal of fluid);
- resection (partial removal of an organ);
- cystogastrostomy (anastomosis).
With the edematous form of pancreatitis, radical treatment is rarely required. It is indicated in case of development of purulent complications or concomitant cholelithiasis. Endoscopic operations are most often performed. Their feature is low trauma and the ability to visualize the organ on the screen through a tube with a camera. All operations are performed within the walls of the hospital.
Diet
In the first 2-3 days after the onset of an attack of pancreatitis, table No. 0 is prescribed. This means that the patient needs to fast. In this condition, you can drink water without gases, rosehip decoction and jelly. The amount of fluid consumed should be 2-2.5 liters per day. On days 3-5 from the onset of pancreatitis, diet No. 5 is prescribed.
It is allowed to eat liquid porridges (with the exception of wheat), low-fat soups, dried bread, fermented milk products, weak tea, low-fat fish, mashed potatoes, cereals, baked and boiled vegetables, sweet fruits and steam omelettes.
In the first 2-3 days after the onset of an attack of pancreatitis, table No. 0 is prescribed. This means that the patient needs to fast.
Therapeutic nutrition for pancreatitis involves excluding from the diet fatty foods, sweets with rich cream, baked goods, coffee, chocolate, sparkling water, pickles, raw vegetables, alcohol and mushrooms.
How to prevent
It is better to prevent diseases than to treat them. This applies to edematous pancreatitis and complications of the disease. The first condition for preventing edematous pancreatitis is proper nutrition. You will have to pay special attention to your health, monitor your diet and eating habits. Minimal consumption or complete refusal of unhealthy fatty, fried foods, elimination of bad habits will help maintain a healthy pancreas and body.
Carbohydrate foods, chocolates, and sweets will not be beneficial. Fast food combined with carbonated drinks, which are popular among young people today, causes great harm to the body. Pay attention to the medications you are taking. Strict use as prescribed by a doctor who knows about other diseases will prevent medications from triggering the development of the disease.
Regular examination will not be superfluous for people with already diagnosed diseases of the digestive system. Timely examination and detection is half the success. Diseases in the gastrointestinal tract often give rise to inflammatory processes in the pancreas. Proper treatment will reduce the likelihood of edematous pancreatitis.
source
Complications
If acute pancreatitis is not treated in a timely manner, the following consequences are possible:
- pancreatic necrosis;
- sepsis (blood infection by bacteria and their toxins);
- shock;
- renal and liver failure;
- aseptic or purulent lesion of the abdominal wall;
- inflammation of the pleura;
- respiratory failure;
- shock lung;
- collapsed lung;
- multiple organ failure;
- encephalopathy (brain damage due to chronic lack of oxygen);
- depression;
- psychosis;
- thrombosis of large vessels;
- suppuration with the formation of abscesses;
- formation of cysts;
- bleeding;
- diabetes;
- jaundice;
- anemia (decreased levels of red blood cells and hemoglobin);
- drop in blood pressure;
- formation of fistulas between the pancreas and the stomach or intestines;
- tumors.
Complications of pancreatitis can be early (in the first days of the disease) and late (develop after 1-2 weeks or later).
Development of oncology
A serious complication of acute pancreatitis is the formation of a benign or malignant tumor. This happens when gland cells degenerate. This pathology develops slowly in people who do not follow treatment recommendations.
A serious complication of acute pancreatitis is the formation of a benign or malignant tumor. This pathology develops slowly in people who do not follow treatment recommendations.
Necrosis
Edematous pancreatitis can be complicated by necrosis (death) of pancreatic tissue. Pancreatic necrosis develops. The mortality rate for this pathology reaches 30-80%. Most often, tissue necrosis is preceded by the consumption of large amounts of alcohol. Pancreatic necrosis can be fatty (with increased activity of the lipase enzyme), hemorrhagic (with impaired microcirculation) and mixed.
Tissue necrosis in pancreatitis is characterized by severe pain, uncontrollable vomiting not associated with food consumption, increased sensitivity of the skin in the projection of the organ, signs of vascular and respiratory disorders. Pancreatic necrosis often leads to abscess, phlegmon (spread purulent melting of tissue) and fibrosis (overgrowth of connective tissue) of the gland.
Massive cell death causes enzymatic deficiency.
Cyst
Pseudocysts in pancreatitis are formed due to incomplete resorption of necrotic tissue. As a result, a capsule and connective tissue are formed, inside which pus or other secretion is located. Cysts form in the body, head or tail of the pancreas. Cysts up to 5 cm in size may not cause symptoms.
Formations localized in the area of the ducts of the organ are prone to spontaneous resorption. Large cysts are manifested by severe pain, which soon decreases. There is a typical period when a person experiences an imaginary improvement in well-being after acute pancreatitis.
Large cysts can compress surrounding tissue and rupture. In the latter case, the pain syndrome intensifies. When the ureters are compressed, dysuria in the form of urinary retention or pain is possible. Sometimes cysts develop intestinal obstruction.
Acute edematous pancreatitis
Acute edematous pancreatitis is familiar to a considerable number of people.
Pathology occurs as a result of the inflammatory process. Patients themselves contribute to its occurrence. By eating improperly and abusing alcohol, people create favorable conditions for the development of the disease. Often the cause is problems in the duodenum. Gastritis provokes the disease. With proper treatment, the disease is curable. A frivolous attitude towards lifestyle and nutrition becomes the cause of pancreatic necrosis, during which the pancreas becomes inflamed, enlarges, and edema appears. Edematous pancreatitis is a mild form of inflammation. The structure of the gland has a lobular appearance; foci of necrosis and exudate may occur in the abdominal cavity.
- Fried or fatty foods;
- A sharp transition from lean foods to fatty foods;
- Failure to comply with the gradual transition to the usual regimen after dietary nutrition;
- Toxic drugs;
- Change of basic food products (to spicy unusual foods);
- Alcohol consumption;
- Ingestion of toxic substances into the body.
Doctors say that edematous pancreatitis often occurs due to problems in the digestive system, due to improper food intake, a sudden diet break, or alcohol consumption. Some patients mistakenly talk about the relationship between microbes and the appearance of edema, but the cause of the inflammatory process and swelling is spasm and disturbances in digestive secretion.
Pancreatic enzymes are very aggressive and long-term exposure causes destructive processes in the body. It is necessary to identify swelling in time and begin treatment, avoiding necrosis. Edematous pancreatitis also affects other areas responsible for the endocrine system. For this reason, the secretion of enzymes decreases, and impaired synthesizing processes of glucagon and insulin lead to diabetes mellitus.