What is bowel cancer?
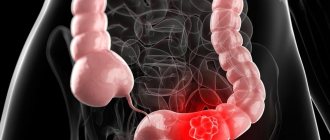
Colon cancer is a malignant degeneration of the glandular epithelium, mainly of the colon or rectum. The first stages are characterized by sluggish symptoms, distracting from the primary pathology and reminiscent of a gastrointestinal disorder. The leading radical treatment method is surgical excision of the affected tissue.
Epidemiology
In official medicine, intestinal cancer is referred to as “colorectal cancer.” This is a collective name consisting of two roots: “colon” and “rectum”. It is in the corresponding parts of the intestine that the maximum number of primary malignant tumors is detected.
Colon (lat. colon) is a colon with four consecutive sections:
- ascending, which is located vertically on the right side of the human body;
- descending - vertically on the left side;
- transverse - connects the ascending and descending sections, located in the upper part of the abdominal cavity, just below the stomach and liver;
- sigmoid - forms a peculiar short bend in the form of a letter (Σ), is located at the bottom on the left side and connects the descending and rectum.
Rectum (lat. rectum) is the rectum (located in the pelvis).
In the cecum and appendix (third section of the large intestine) and small section (duodenum, jejunum, ileum), malignant neoplasms are much less common. The average incidence of cancer detection outside the large intestine is 0.4-1.0% of all cases of intestinal oncology.
Important epidemiological features of colon cancer:
- occupies a leading position in the structure of oncological diseases, inferior to: in men – stomach cancer and lung cancer, in women – breast cancer;
- the most common morphological form of this cancer is adenocarcinoma (malignant degeneration of benign intestinal polyps consisting of glandular tissue);
- the probability of developing adenocarcinoma in the intestine is 98-99%, the incidence of sarcoma and other types of tumors does not exceed 1-2%;
- the most common location of the tumor: in the rectum (about 50%), in the sigmoid colon (up to 40%), in the descending and ascending colon (about 7%), in the transverse colon (about 3%);
- Women are more often (up to 55%) diagnosed with cancer of the colon, and men (up to 60%) are diagnosed with cancer of the rectum;
- The disease occurs at any age, a sharp rise in incidence is observed after 40 years, the peak occurs in the period from 60 to 75 years.
In Russia, about 40 thousand cases of colorectal cancer are diagnosed annually with a mortality rate of up to 30 thousand. High mortality is associated with the health status of older people, who almost always have comorbidities.
The paradox is that colorectal cancer is not a pathology with difficult to detect symptoms. This disease can be detected by modern instrumental and laboratory methods even at the earliest stages, but it is characterized by a significant number of diagnostic errors associated with the multiplicity of clinical manifestations of the disease.
In this regard, it is very important:
- qualifications and oncology alertness of doctors performing the initial appointment at the district clinic;
- attentiveness of patients (especially older and older people) suffering from gastrointestinal disorders and those at risk of colorectal cancer.
Diagnosis of any disease, and especially in the early stages, is always a dialogue between the doctor and the patient. Very often, information from a patient who correctly describes the signs of a disease is crucial.
However, patient alertness is not the main link in timely diagnosis of cancer for the following reasons:
- A doctor conducting an appointment at a clinic may not pay attention to signs of oncology in a stream of patients. Its symptoms are varied, perhaps erased, especially since increased fatigue, weight loss, diarrhea, blood in the stool, discomfort or pain in the abdomen, rapid heartbeat (the main signs of the first stages) resemble many diseases, and are effectively, albeit temporarily, eliminated medicines.
- It is sometimes psychologically difficult for a local therapist to replace a previously made diagnosis associated with a banal chronic digestive disorder with a frightening one - cancer, and promptly refer the patient to a specialist for a highly sensitive examination;
- Only the patient knows about his own predisposing risk factors for oncology in the form of similar diseases in blood relatives, the characteristics of his personal lifestyle, the nature of his work, nutrition, and the presence of some individual delicate symptoms.
The knowledge gained within the framework of this educational article will help the average person understand the causes of the disease to the extent sufficient to draw the attention of the clinic doctor to this problem during the initial appointment.
Cancer is not always a death sentence! This is a situation where it is better to make a mistake in guessing a formidable diagnosis than to mistakenly make a banal diagnosis. For timely detection of pathology, a prepared patient is needed who does not become depressed just from the suspicion of oncology in his body.
Prevention of relapse after colorectal cancer treatment
After treatment for colon cancer, recurrence is possible. In addition, patients who go into remission have an increased risk of stomach, bile duct, uterine, kidney, and ureteral cancers.
There are some measures that can help reduce the risk of relapse:
- Follow your doctor's recommendations. Show up for appointments on time and get tested. This will help to detect a relapse in time and increase the chances of its successful treatment. Typically, periodic examinations include colonoscopy, computed tomography, and blood tests for tumor markers.
- Stop smoking.
- Maintain a healthy weight.
- Stay physically active.
- Eat a healthy diet. Limit your meat consumption and give preference to plant-based products.
- Avoid alcohol.
| More information about treatment at the European Clinic: | |
| Oncologist-gastroenterologist | 5100 rub. |
| Chemotherapy appointment | 6900 rub. |
| Emergency oncology care | from 11000 rub. |
| Palliative care in Moscow | from 40200 per day |
| Radiologist consultation | 10500 rub. |
Book a consultation 24 hours a day
+7+7+78
Symptoms of bowel cancer
Diagnosing cancer based only on clinical symptoms is futile due to the numerous manifestations of the disease. The following description of symptoms is given to show the variety of manifestations of pathology, and to confirm the importance of competent medical diagnosis using modern methods.
Colorectal cancer has no characteristic (pathognomonic) symptoms. There are several groups of symptoms of intestinal cancer that characterize various pathological processes within the patient’s body.
Toxic-anemic symptoms
The initial stages of intestinal cancer are accompanied by a violation of the integrity of the mucous membranes of the intestinal walls.
As a result, the gates of infection open, the contents of the intestines enter the blood, causing intoxication, which manifests itself:
- increased fatigue, weakness, headache, nausea, and other signs of intoxication;
- elevated body temperature, joint pain (a consequence of toxicosis);
- loss of blood from small vessels of the intestinal wall, anemia, pallor of the mucous membranes, decreased hemoglobin levels, thickening of the blood, changes in its other indicators and, as a result, changes in the rhythm of the heart and breathing.
The disease can be confused with a variety of intoxications caused, for example, by inflammatory diseases of the heart, joints or upper respiratory tract.
Enterocolitic inflammation of the large intestine: symptoms
This inflammation is formed mainly with extensive damage to the mucous membranes, when toxins begin to enter the blood from the surface of the damaged membranes, and in addition to intoxication, intestinal dysfunction occurs.
Pathology manifests itself:
- increased body temperature, reminiscent of an infectious fever;
- constipation and more often - diarrhea;
- increased gas formation as a result of rotting intestinal contents, bloating and rumbling;
- involvement in the pathogenesis of intestinal sphincters that regulate peristalsis. The process is accompanied by periodic pain in the abdomen (left or right), especially after eating;
- mucus, visible blood and pus in the stool.
In the absence of oncological alertness, the doctor may confuse these symptoms with dysentery, inflammatory processes in the large intestine.
Dyspeptic bowel disorder: symptoms
This disorder is detected when a large number of pain receptors are involved in the pathogenesis and irritation as a result of ulceration of the walls of the mucous membranes, as well as in the initial stages of metastasis to the liver.
Symptoms appear as:
- severe abdominal pain;
- unpleasant belching is a sign of damage to the sphincters and liver;
- nausea and vomiting – toxemia;
- diarrhea or constipation - impaired intestinal motility;
- elevated body temperature.
Dyspeptic intestinal disorder resembles an inflammatory process in the appendix (this is part of the large intestine), as well as in organs adjacent to or functionally associated with the large intestine (pancreas, stomach, small intestine, gall bladder).
Obstructive blockage of the intestinal lumen: symptoms
Blockage is detected when the tumor metastasizes and the formation of inflammatory adhesions around it.
The pathology usually manifests itself as signs of partial blockage of the lumen of the colon in the form of:
- prolonged constipation that is not eliminated by enemas and laxatives;
- heaviness in the stomach;
- increased pain after eating.
Signs of blockage resemble diverticulosis (formation of pockets filled with feces in the intestinal walls), adhesive disease, spastic pain in the intestines, the presence of fecal stones (calculi) in the lumen of the rectum.
When the small intestine is involved in carcinogenesis, symptoms of acute and complete intestinal obstruction, intussusception (protrusion of the walls), and volvulus are formed. These phenomena are manifested by severe pain, uncontrollable vomiting, sometimes immediately after eating, and the rapid development of cancer symptoms.
Pseudo-inflammatory (resembling general inflammation) symptoms
They develop in the later stages of oncology with metastases to the lungs, ovaries, and other organs; very often the symptoms are combined with a palpable tumor.
The following signs of the disease are detected:
- heat;
- severe, constant pain in the abdomen, sometimes of unclear localization;
- purulent and bloody discharge from the anus during bowel movements;
- constipation, inability to defecate without an enema, difficulty evacuating intestinal gases;
- symptoms associated with organs affected by metastases, for example, cough when the lungs are involved, dyspepsia when the liver is involved, discharge from the genital organs when they are involved in carcinogenesis.
Warning signs
Depending on the location of the tumor, certain symptoms of bowel cancer may appear. It is advisable to divide them into 3 groups.
- Symptoms of small intestine cancer.
- Symptoms of colon cancer.
- Nonspecific symptoms of an oncological process in the body.
Small bowel cancer
Oncological diseases rarely affect the upper intestines. However, it is there that they are diagnosed later due to the mildness of symptoms. Early clinical signs are only present when the tumor is located in the area of the papilla of Vater - the area where the bile and pancreatic ducts flow into the duodenum. Tissue growth can block the flow of digestive secretions. In this regard, there are:
- icteric staining of the skin and visible mucous membranes;
- skin itching;
- pain in the right hypochondrium;
- pain in the epigastric region (along the midline of the abdomen at the level of the ribs joining the sternum), encircling the left side;
- a picture characteristic of chronic cholecystitis and pancreatitis.
Colon cancer
Tumor damage to the lower intestine manifests itself the earlier, the closer the tumor is located to the anus. Complaints, as a rule, are well formulated by patients and bring them to the doctor quite early.
- Unstable stool is an alternation of diarrhea and constipation, which usually indicates a partial blockage of the intestinal lumen.
- “Ribbon-shaped” stool is observed if the tumor is located in the rectum and prevents the passage of stool.
- Blood usually appears on the surface of already formed stool in the form of stripes or streaks.
- At later stages, mucus and pus appear in the stool (already when the tumor disintegrates).
- Tenesmus is a painful urge to defecate associated with irritation of the rectum by excess tissue or pathological discharge (blood, mucus and pus). At the same time, there is no feces ready to be excreted from the body.
- Gas and fecal incontinence occurs when cancer destroys the anal sphincter and it loses its ability to hold intestinal contents.
- If a growing tumor completely blocks the intestinal lumen, a picture of obstruction develops. In this case, the patient is urgently hospitalized in a surgical hospital for surgical treatment. Often this is the first and only manifestation of cancer.
- When the tumor grows through all layers of the intestinal wall and involves the abdominal cavity, a picture of peritonitis or ascites (fluid accumulation in the abdomen) is possible.
- A rectal tumor in women can spread to the tissues of the vagina and bladder. Then patients experience difficulties in sexual activity and urination. In the stage of decay, fistulas form between these organs. In this case, gases and feces may be released from the vagina, and urine from the anus.
The first signs of bowel cancer
It is advisable to identify the first signs of intestinal cancer using instrumental methods of visual examination of the walls of the large intestine, by probing or by radiation methods, without penetrating into the body.
The basis for prescribing instrumental or laboratory tests are:
- at-risk groups;
- age over 40 years, but there are cases of the disease at a younger age;
- the presence of some signs indicating damage to the gastrointestinal tract against the background of any other symptoms, for example, a combination of disorders of the heart and excretory functions against the background of intestinal dysfunction.
A very important role during this period is played by the competent oncological alertness of the general practitioner, because in 70-90% of cases people turn to the general practitioner in the early stages of the disease, often for reasons that have no apparent relation to cancer.
The doctor usually thinks about the possible layering of oncology when the following subjective sensations appear or intensify in the patient (at least three at a time), including:
- general weakness;
- fast fatiguability;
- pain in a certain anatomical area of the abdomen (see intestinal anatomy above);
- progressive weight loss;
- slight but persistent increase in body temperature;
- blood or mucus in stool;
- dark (black) stool;
- pallor of the mucous membranes and skin;
- lack of relief after effective therapeutic procedures.
Naturally, these signs are not an accurate indication of cancer; one should always take into account the patient’s suspiciousness, individual pain sensitivity threshold, and other clinically important parameters for diagnosis. When the doctor confirms the patient’s complaints, the diagnosis is clarified on the basis of clinical, instrumental and laboratory studies.
It is inappropriate to list the primary macro- and microscopic changes in the intestinal walls that diagnosticians detect during examinations in this article, since such knowledge is purely professional.
Symptoms of intestinal tumors
Intestinal tumors manifest themselves with different symptoms, correlating with the localization of the pathology, the size of the growth, and histological structure.
Symptoms in the thin section
Tumors of the small intestine do not show themselves for a long time. Tumor-like pathologies of the small intestine at an early stage are discovered accidentally during a preventive examination.
The first signs of a benign tumor of the thin section:
- pain in the center of the abdomen or on the left;
- belching, increased gas formation;
- poor appetite;
- unstable stool - diarrhea gives way to constipation.
As the growth enlarges, the manifestations become brighter and more saturated. The growth protrudes into the intestinal lumen and blocks it. Characteristic symptoms of intestinal obstruction occur - abdominal pain, nausea, vomiting, stool and gas retention. Polyps of the small intestine reveal themselves by abundant secretion of mucous secretion.
Symptoms of a malignant tumor of the small part:
- intestines hurt unbearably;
- body temperature rises;
- nausea, vomiting, heartburn, belching in the early stages of the disease;
- diarrhea interspersed with stool retention;
- intestinal obstruction;
- rupture of the intestinal wall in the terminal phase.
Symptoms of small intestinal neoplasms with a long course and large size of the growth are manifested by loss of appetite, emaciation, weakness, and fatigue. Signs of tumor-like growths of the small intestine in women are hidden behind symptoms of inflammation of the ovaries and uterus, which are also characterized by cramping abdominal pain in women. Hot flashes caused by neuroendocrine formations are similar to those of the menopausal period.
Symptoms in the thick section
Neoplasms of the large intestine announce themselves with the first symptoms:
- discomfort in the lower abdomen;
- blood and mucus in stool;
- there is a frequent alternation of loose stools with dense feces;
- intestinal blockage;
- bleeding after cancer disintegrates;
- anemia, hypovitaminosis, metabolic disorders.
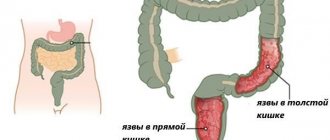
The location of the cancerous growth can indirectly be determined by the type of bloody discharge:
- tumor of the rectum and the adjacent area of the sigmoid - scarlet blood, without mucus;
- localization of pathology in the descending part of the colon - dark blood mixed with feces and mucus;
- the presence of a malignant growth in the ascending, transverse part of the colon and cecum does not manifest itself in any way. Hidden bleeding is expressed by anemia, fatigue, pallor of the skin and mucous membranes.
People with bowel cancer look exhausted and tired. Their liver becomes enlarged, and an accumulation of exudate appears in the abdominal cavity - ascites (dropsy). Against the background of a thin body, the stomach is swollen, the skin is very stretched, with protruding blood vessels.
Causes of bowel cancer
Colorectal cancer is common among people with a predominant diet of animal proteins and fats, leading a sedentary lifestyle - these are residents of Europe and North America (regardless of race).
In African countries, with a diet of predominantly plant proteins and carbohydrates with a high content of plant fiber in food, as well as a high level of physical labor, the incidence rate is 10-20 times lower than in developed countries. But Africans living in Europe or America for a long time make up a significant group of patients with colon cancer.
This gives reason to believe that it is the excess of meat in the diet against the background of a deficiency of plant fiber necessary for peristalsis and bowel movements during bowel movements, and a sedentary lifestyle that are the main causes of colorectal cancer. The theory of racial resistance to cancer is untenable.
The three most likely pathways leading to intestinal cancer (although the true causes of the occurrence and development of carcinogenesis are not fully known):
I. group of reasons
In some cases, precancerous stages occur without clinical manifestations in the form of dysplasia (changes at the cellular level). A person feels completely healthy for a long time; periodic disorders are mistaken for minor disorders that can be eliminated with minimal effort. Cancer in this case is a surprise for both the patient and the doctor.
II. group of reasons
Another part of precancerous conditions is disguised as chronic pathologies. There is certainly a proven fatal link between some diseases of the gastrointestinal tract and colorectal cancer.
Here are some of the most significant diseases that are most likely to precede cancer:
- Polyposis of the large intestine (the probability of malignant degeneration (malignancy) is up to 100%), sometimes associated with genetic disorders in close relatives. Not all are precursors to cancer; the most dangerous polyposis are:
diffuse familial, has the following clinical signs - frequent bowel movements, more than five times a day, bloody stools, pain or discomfort in the abdomen of varying intensity;
- villous, has the following signs - copious mucus discharge during bowel movements (up to 1.5 liters per day), other symptoms (see diffuse polyposis);
- Turcot syndrome is a rare hereditary disease that combines a brain tumor and colon polyposis, see the symptoms of polyposis above;
- Peutz-Jeghers-Touraine syndrome is a combination of pigment spots on the face and polyps in the large intestine in relatives.
- nonspecific ulcerative colitis - diarrhea, frequency of bowel movements up to 20 times a day, blood or pus in the stool caused by ulcers on the intestinal walls, pain in the lower abdomen, bloating of intestinal loops (protrusion of the lower abdomen);
- diabetes mellitus type 2 (non-insulin dependent) – increased thirst, large volume of urine with normal frequency of urination, itching, dry skin, obesity, weakness, prolonged healing of skin and muscle damage.
III. group of reasons
Diseases that do not precede cancer, but often overlap with this disease and confuse the clinical picture.
This is relevant if the doctor supervises the patient for a long time, for example, regarding:
- hemorrhoids;
- diverticula (pockets in the intestinal walls);
- chronic intestinal obstruction;
- anal fissures or fistulas;
- other diseases of the lower gastrointestinal tract.
Each disease has its own typical clinical picture with the same or common symptom for all listed diseases - difficult, painful defecation.
Stages of bowel cancer
The division of cancer pathogenesis into different stages is accepted throughout the world. There are different approaches to this issue, but the entire medical community recognizes the feasibility of division. This classification method greatly simplifies the description of carcinogenesis and standardizes its understanding. In our country, it is generally accepted to distinguish four main stages of cancer and several possible variants within each stage.
For the diagnosis of intestinal cancer, the following classifications have been proposed, including those used abroad:
- S. Dukes et al., a total of six stages, uses the principle of determining the depth of tumor germination and the presence of metastases in the lymph nodes;
- TNM (Latin equivalents of the first letters denoting “tumor”, “lymph node”, “metastasis”) is an international classification widely used by Russian doctors. There are 4 stages of cancer in total, one stage of precancer. The abbreviation of the classification contains its principle.
There are other classifications. We will focus on the TNM classification, as the most common in our country, and describe the characteristic features of each stage.
When there is no reason to consider changes indicating signs of cancer as established, this condition has a symbol - (Tx). If there are signs indicating precancerous symptoms, then the designation (Tis) is used. To describe the involvement of regional lymph nodes in carcinogenesis, the designation N is used. If, during the examination of the patient, no convincing evidence of damage to the nodes is obtained, then the results are designated by the letters (Nx), and if it is clearly established that the nodes are not damaged, then this is designated (N0). The letter M (metastasis) is not used in the description of precancer.
Stage 1 colon cancer
In medical histories, examination reports and other official medical documents, it is indicated by a combination of letters and numbers (T1 N0 M0). This is the initial stage, clinically it is manifested by general symptoms of intoxication. Upon instrumental examination, it is visualized as a small, mobile, dense formation or ulcer (T1). Changes are found in the mucous membrane or submucosal layer. Lymph nodes are not affected (N0). There are no metastases (M0).
Colon cancer stage 2
There are two possible options for describing this stage in medical documents with the results of instrumental studies: (T2 N1 M0) or (T3 N0 M0). These options differ in the size of the tumor. Namely, the size of the tumor is described from a third to half the diameter of the intestine (T2 and T3). In one variant there are signs of damage to the nearest lymph nodes (N1), and in the second there is no damage (N0). Distant metastases are always absent (M0).
Colon cancer stage 3
This form of colorectal cancer is distinguished by a variety of morphological and cytological forms of carcinogenesis.
There are seven possible description options, including milder manifestations, designated:
- (T4 N0 M0) – the tumor occupies more than 50% of the intestinal diameter, the lymph nodes are not affected, there are no metastases;
- (T1 N1 M0) – a small mobile tumor, the nearest lymph nodes are affected, without distant metastases in the liver;
- (T2 N1 M0) – tumor up to 30% in diameter, nearby lymph nodes are affected, no metastases;
- (T3 N0 M0) – tumor up to 50% of the intestinal diameter, no damage to the lymph nodes, no metastases.
Relatively more severe forms of the third stage are designated:
- (T4 N1 M0) – a massive tumor surrounding the intestine, adhesions form with neighboring organs and tissues, the nearest 3-4 lymph nodes are affected, there are no distant metastases;
- (T1-4 N2 M0) – the size of the tumor does not matter, more than four intestinal lymph nodes are affected (N2), there are no metastases.
- (T1-4 N3 M0) – the size of the tumor does not matter, the lymph nodes along large blood vessels are affected (N3), that is, there is a massive spread of cancer cells throughout the body, there are no distant metastases yet.
Colon cancer stage 4
This is the last, most dangerous stage of the disease, characterized by distant metastases in the body. In medical documents it may be designated (T1-4, N1-3 M1). The size of the tumor and damage to regional lymph nodes are not of fundamental importance. However, distant metastases are always present, usually in the liver (M1).
Metastases in the intestine
A feature of colorectal cancer is distant metastases to the liver; much less often they are found in the lungs, brain, genitals and omentum. The growth of malignant cells into vital organs greatly reduces the likelihood of successful treatment of patients.
Intestinal metastases in adenocarcinoma are found in 50% of cases, in colloid cancer in 70%, and in anaplastic types of cancer in about 82%. When comparing the frequency, squamous cell forms of cancer metastasize more often, but they can be found much less frequently than glandular cancers.
Disease prognosis
In Russia there is no system for early cancer prediction. The reason is the chronic lack of funding for useful activities. Therefore, there are no highly sensitive methods for detecting cancer available for mass use.
Occult blood tests, which are widely used in our clinics, give many false results, and DNA diagnostics are still limited in their availability for mass research.
Modern prognosis mainly depends on the literacy and oncological alertness of the doctor, who knows how to find a connection between diseases of the gastrointestinal tract and precursors of cancer. The prognosis is based on the doctor’s subjective feelings and the results of a visual examination of the patient, so up to 20% of Russian patients have a primary diagnosis of intestinal cancer with distant metastases.
Ways to improve objective forecasting methods are based on the introduction of highly effective instrumental and laboratory techniques into mass medical practice.
In the presence of an already formed tumor, the most promising methods for objectively predicting the rate of development of metastases are the determination of specific protein markers, including the Oncotype Dx colon test and others.
How long do you live with bowel cancer?
The question contains a fatal meaning of the mortal danger of cancer. But let's be optimistic, because in the early and sometimes in the later stages of the disease, doctors achieve amazing success in the radical treatment of this form of oncology.
The answer to the question posed about life expectancy can be divided into two parts:
- the first concerns the quality and duration of life after diagnosis;
- the second is the frequency of examinations in order to detect oncology at the earliest possible stages.
Information on the five-year survival rate of patients with intestinal cancer, often used in scientific research to show trends and patterns of the disease, is incorrect in the context of a popular article, because the body of each individual person has a different safety margin, depending on:
- age;
- concomitant pathologies;
- bad habits;
- living conditions;
- stress and so on.
Of the above, only age cannot be adjusted. Proper treatment of concomitant pathologies, giving up bad habits, selecting a diet, eliminating stress significantly increases the likelihood of not getting sick, and the patient’s chances of recovery and a significant prolongation of life with the help of surgeons and doctors of other specialties increase.
A quality life is possible even with significant excision (resection) of part of the intestine and the application of a colostomy (an opening for excreting feces outside, bypassing the anus). The presence of a colostomy, with normal care, is not a significant factor reducing the quality of life.
On the other hand, the earlier cancer is detected, the greater the chance of successful treatment. Following this logic, it can be assumed that extremely frequent examinations provide a chance for early detection of the disease and prolongation of life. Fortunately, this is not entirely true.
Early confirmation of the diagnosis is possible with examinations at intervals of one year. After all, from the first mutations to the onset of clinical stages, on average, two to three years pass.
To significantly increase the length and quality of life, screening studies should be carried out annually after the age of forty.
When the disease is detected in late stages, proper patient care and maintaining good hygienic condition of the colostomy play an important role in prolonging life.
If intestinal cancer was detected at stage 1, and the tumor has not yet spread anywhere (which happens extremely rarely, with a happy coincidence), then the chance of success reaches 99%.
If the cancer is at stage 2, when the tumor begins to grow on the intestinal walls, then the chance of cure is 85%.
At stage 3, when the tumor affects the nearest lymph nodes, the chance of cure drops to 65%.
In the later stages of bowel cancer, when distant lymph nodes are affected, the chance of cure is about 35%.
How long a person will live after recovery depends on the severity of the disease, as well as on other factors listed above.
On the subject: Selenium reduces the risk of cancer by 2 times, what foods contain it?
Treatment
The most effective method of combating colon cancer is still surgical treatment.
Chemotherapy does not produce significant results. It is used only to prevent tumor growth and spread of metastases. Can be prescribed before and after surgery.
Radiation therapy is used to eliminate any remaining abnormal cells after radical surgery. And also for the prevention of relapse of the malignant process and the spread of metastases.
Treatment should be comprehensive, that is, combine various methods.
Surgical therapy
In the early stages of intestinal cancer (I, II), surgery is quite effective (in 90% of cases). In case of tumor metastasis, in addition to radical treatment, chemotherapy and radiotherapy are used.
Basic methods of colon cancer surgery:
- Resection (removal) of part of the intestine for small tumors (stage I or II)
The operation is performed under general anesthesia by laparoscopy. Small incisions (from 0.5 to 1.5 cm) are made on the anterior wall of the abdomen with a scalpel. Through them, surgical instruments and an endoscope, at the end of which there is a video camera and a light source, are inserted into the abdominal cavity. The image is displayed on the monitor screen. The surgeon isolates the affected part of the intestine and performs resection. The tumor is completely eliminated without contact with it (prevention of relapse). Then an anastomosis (connection) is formed. The resulting stumps of the two intestinal tubes are stitched with a surgical stapler.
This method is less traumatic and has a low risk of infectious complications. Patients recover within a week.
- Resection of the affected intestine
Used for large tumors (III, IV). The operation is performed by laparotomy. A longitudinal incision is made on the anterior abdominal wall and secured with clamps. The surgical field is inspected to determine the resection area. The affected intestine is isolated and fixed with clamps. Excision is performed within healthy tissue (to prevent contact with the tumor and reduce the risk of relapse).
Total resection is carried out for malignant tumors of impressive size. In this case, the small or large intestine is completely removed, then an anastomosis is performed. The remaining stumps can be of different diameters, and difficulties arise when restoring the organ.
Be sure to read:
Histological examination of intestinal tissue: preparation and implementation
Possible complications: infection and bleeding (during and after surgery), adhesions at the anastomotic sites, pain due to limited peristalsis, hernia (protrusion of the intestine), digestive upset (flatulence, constipation or diarrhea) and disruption of bowel and bladder emptying ( encopresis and enuresis).
- Bowel resection with colostomy
An artificial opening for excreting feces is formed above the site of organ damage. Colostomy can be temporary (to unload the intestines after surgery and effective recovery). The sutures heal faster (within one month). Then the colostomy is eliminated, and the patient regains physiological bowel movements. In rare cases, the artificial hole remains for the rest of your life. With a permanent colostomy, patients need to learn how to use special colostomy bags. The anus is sutured.
Complications of this method of surgery: the formation of an abscess due to infection of the abdominal wall with feces, necrosis of the excreted intestine, narrowing of the outlet (with insufficient fixation), prolapse of intestinal loops into the wound with weak mobilization, prolapse of the intestine due to active peristalsis and increased intra-abdominal pressure.
Chemotherapy
Toxic drugs are prescribed to reduce tumor growth and the risk of metastasis.
Used before and after surgery, as well as as palliative care for cancer patients with inoperable tumors at the last stage. The following chemical compounds are used: “5-fluorouracil”, “Capecitabine”, “Oxaliplatin” and others. All drugs block the division of atypical cells, worsening their metabolism. Chemotherapy is accompanied by side effects:
- severe weakness;
- headache;
- dyspeptic disorders (nausea and vomiting);
- alopecia (hair loss).
Leucovorin is a physiological agent based on folic acid that reduces the side effects of chemotherapy on healthy organs and tissues. Prescribed along with toxic drugs.
Radiation therapy
Treatment of intestinal cancer using ionizing radiation (neutron, x-ray, gamma). Radiotherapy prevents cancer cells from recovering, dividing and growing further. Radiation exposure is contraindicated in severe cardiac pathology, diseases of the lungs, liver and kidneys in the period of exacerbation, in acute infections and blood diseases. Not for use in pregnant women and children under 16 years of age.
Types of radiation therapy:
- Application of radionuclides. The drugs are administered inside the body using special solutions that must be drunk; either intravenously, into the abdominal cavity or directly into the tumor itself.
- Remote technique. The cancerous tumor is irradiated through healthy tissue. Suitable for tumors located in hard-to-reach places.
- Contact radiotherapy. Closed sources of radiation (needles, wire, capsules, balls, etc.) are introduced into the tumor. Implantation of foreign objects can be temporary or permanent.
Radiotherapy is accompanied by side effects due to damage to healthy organs and tissues. Local and general reactions are distinguished. Local damage affects the skin (dermatitis, erythema, atrophy and ulcers), mucous membranes (redness and swelling, erosions and ulcers, atrophy, fistula formation) and organs (ulcers, fibrosis, necrosis). General symptoms are associated with the adverse effects of radiation on the body (inflammation of the intestines, metabolic disorders, persistent changes in blood composition, dysfunction of the digestive system). With repeated use of radiotherapy, chronic radiation sickness and cancer of other organs develop.
Diagnosis of bowel cancer
The choice of diagnostic regimen is determined by the doctor. The minimum includes screening studies, primarily a fecal occult blood test, which is a very simple and publicly available method used in the most primitive laboratories.
- Patients at risk should have a stool test once a year to exclude hidden bleeding; this method allows you to identify a tumor or polyp with a diameter of 2 cm or more;
- If the test for occult blood is positive, fibrosigmoscopy or rectomanoscopy with video recording or contrast examination of the colon is prescribed.
A real breakthrough in the diagnosis of intestinal cancer occurred after the widespread introduction into medical practice of radiation diagnostic methods, for example, contrast radiography or more modern methods:
- computed tomography and its modifications (CT, MSCT);
- ultrasound diagnostics through the abdominal wall and using sensors inserted into the intestines (ultrasound, TRUS, others);
- magnetic resonance imaging and its modifications (MRI)
- positron emission tomography (PET-CT).
A promising method is the laboratory determination of DNA markers for colon cancer. After all, this form of the disease is one of the few that can be identified long before the onset of the clinical stage, and thereby save life without painful treatment procedures.
Causes of colon cancer
The causes of colon cancer, like any other oncology, are not known for certain, but there are risk factors for its development:
- A diet high in animal fats, carcinogens,
- Heredity,
- Inflammatory bowel diseases (Crohn's disease, ulcerative colitis),
- Smoking,
- Alcohol.
A cancerous tumor can arise from the degeneration of a polyp (benign neoplasm) or appear on its own. It develops slowly and may not manifest itself in any way in the early stages.
The most common clinical manifestations of colon cancer are blood in the stool or black stool (if the lesion is located further from the rectum) and intestinal obstruction (if the lesion is closer to the rectum). However, these symptoms occur in later stages, when the tumor has penetrated deep into the intestinal wall or has grown to a large size, closing part of the intestinal lumen. Treatment at such stages is no longer effective, so screening plays an important role in the early diagnosis of colon cancer.
Screening is a mass examination that allows you to identify a group of people who require more thorough diagnosis. Stool occult blood testing and colonoscopy are used to screen for colon cancer.
Bowel cancer treatment
Modern methods of treating colorectal cancer are based on radical surgical removal of the tumor, surrounding tissue and metastases. Radiation and chemotherapy methods are used as auxiliary methods. In the medical literature there is information about a significant extension of the life of patients operated on stages 3-4 of intestinal cancer. Some sources indicate a three-year survival rate of 50%, and a five-year survival rate of 30% of surgical patients. The use of combined methods allows us to hope for better patient survival results.
Chemotherapy for bowel cancer
The main limiting factor for the widespread use of chemotherapy for this form of cancer is the resistance of the main forms of intestinal tumors to cytostatic drugs.
Chemotherapy is used systemically, before or after surgery. In some cases, local administration into the blood vessels feeding metastases is indicated. The main drug used for chemotherapy is 5-fluorouracil. In addition to it, other cytostatics are used - capecitabine, oxaliplastin, irinotecan and others. To enhance their action, immunocorrectors (interferogens, stimulators of humoral and cellular immunity) are prescribed.
Surgery to remove a tumor in the intestine
It is generally accepted that this is the only radical treatment for bowel cancer. There are various techniques, including:
- traditional methods of resection of the affected segment of the intestine and surrounding vessels;
- operations through miniature incisions of the abdominal wall;
- removal of the tumor with a package of lymph nodes and metastases using a high-frequency knife.
The technique and method of surgical intervention are chosen by the attending physician based on the recommendations of the consultation. It has been proven that the quality of the operation and the likelihood of tumor recurrence directly depend on the training of the surgical team and the equipment of the specialized clinic.
See also: Other treatments
Treatment of colon cancer
Treatment of colon cancer is complex and includes:
- Surgical removal
- Drug treatment (chemotherapy, targeted therapy, immunotherapy)
- Radiological treatment
Surgical treatment involves resection of the part of the colon affected by the tumor and the creation of an anastomosis or removal of the stoma to the surface of the body, as well as the removal of lymph nodes into which tumor cells can spread.
Chemotherapy can be given before surgery or both before and after. Its goal is to reduce the risk of cancer cells spreading and destroy existing metastases. The decision on additional drug therapy is made individually for each patient.
Treatment methods at the Federal Scientific Center
- Laparocentesis, thoracentesis, drainage and stenting of the bile ducts for obstructive jaundice
- Conducting palliative/symptomatic therapy
- Chemoembolization of liver tumors
- Effective pain relief using modern techniques