Is surgery necessary for a hiatal hernia? Not always. Surgical treatment for hiatal hernia is the only radical method of therapy. With all other methods of treatment (without surgery), the cause of the disease is not eliminated; all measures are aimed at reducing symptoms and preventing complications. Surgeons prefer a conservative treatment route. If it is possible not to have the operation, then it is postponed indefinitely.
There are strict indications for the operation:
- if conservative treatment does not produce results;
- large hernia size;
- complications of the hiatal hernia (strangulated hernia, esophageal stenosis, mucosal metaplasia, bleeding).
Is the size of the hiatal hernia determining whether to have surgery or not?
Large hernias, of course, are one of the indications for surgery for hiatal hernia. The fact is that a large hernia compresses the thoracic organs, causing the development of cardiac and pulmonary pathology. In addition, such patients often experience complications and infringement of the hiatal hernia. Conservative treatment of such patients is almost always ineffective. Strangulated hernias require surgical treatment, often urgently, but the choice of surgical method remains a subject of debate among scientists.
There are 4 degrees of hiatal hernia by volume:
- 1st degree – up to 100 cm³;
- 2nd degree – up to 300 cm³;
- 3rd degree – up to 400 cm³;
- 4th degree – over 400 cm³.
For what sizes is surgical treatment indicated?
Grade 3-4 hiatal hernias are giant hernias; for such sizes, surgical treatment is indicated. It is important that the long-term results of operations for large hernias are very unsatisfactory. Indications and contraindications for various interventions in patients with sliding and fixed hiatal hernias have not yet been clearly defined.
Literature
- Zherlov G.K., Gunter V.E., Kozlov S.V. and others. Surgical treatment of gastroesophageal reflux disease combined with duodenal ulcer // Bulletin of surgery. 2007. T. 166. No. 1. P. 51-54.
- Kasumov N.A. Reflux esophagitis: current state of the problem // Surgery. 2007. No. 4. P. 62-65.
- Maev I.V. Gastroesophageal reflux disease // Russian Medical Journal. 2002. No. 3. P. 43-46.
- Chernousov A.F., Shestakov A.L. Selective proximal vagotomy. Moscow, 2001. 158 p.
- Mainie I., Tutuian R., Agrawal A., et al. Combined multichannel intraluminal impedance-pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication // Br. J. Surg. 2006. Vol. 93. R. 1483-1487.
- Pleskow D., Rothstein R., Kozarek R., et al. Endoscopic full-thickness plication for the treatment GERD: long-term multicenter results // Surg. Endosc. 2007. –V. 21.– P. 439-444.
How is surgery performed for a hiatus hernia?
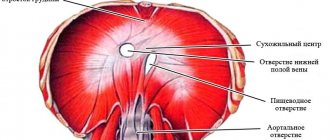
During the operation one achieves:
- restoration of the anatomically correct location of organs;
- eliminate hernial orifices;
- perform one type of fundoplication, which allows you to restore the lower esophageal sphincter (LES) and the angle of His.
The operation is carried out in two ways:
- abdominal surgery with a wide abdominal incision in the midline of the abdomen;
- laparoscopic surgery using endoscopic optics.
The operation lasts 1-2 hours. An operation to remove a hiatal hernia is performed in several stages.
The course of the operation is as follows:
- Before the operation begins, the patient must be given anesthesia. In the case of hiatal hernia, local anesthesia is preferable (spinal anesthesia and general anesthesia are possible).
- Returning organs to their anatomically correct position.
- The distended esophageal opening of the diaphragm is sutured and plastic surgery is performed.
- One type of fundoplication is performed to restore the LES and prevent reflux.
There are about four dozen different modifications of surgery for hiatal hernia. Each of them has its own advantages and disadvantages. In each individual case, the method is chosen by the attending surgeon, based on the preliminary examination data and the patient’s concomitant pathology.
Toupet operation
The basis of the operation is the formation of a symmetrical cuff from the walls of the fundus of the stomach; it wraps the esophagus 270 degrees, leaving the left vagus nerve free.
Surgery to remove a hiatal hernia using this modification results in fewer dysphagia in the early postoperative period (compared to the classic Nissen fundoplication). But it is more often complicated by relapses of GERD.
Operation using the Hill technique for hiatal hernia
The operation using the Hill technique is the most effective of the group of gastroplexy techniques. It creates a strong fixation of the lower esophagus to the para-aortic fascia. This makes it possible to keep this section of the esophagus below the diaphragm, and also creates a fulcrum for the peristaltic activity of the organ. The negative side of the technique is the difficulty of implementation and the high demands placed on the operating surgeon.
Operation according to Chernousov A.F.
Surgeries for hiatal hernias of the esophagus take place against the background of a chronic inflammatory process, which often leads to shortening of the organ. Patients operated on using the classical technique quickly experience a relapse of the disease. According to Chernousov’s method, part of the stomach is turned into a tube using gathering sutures. Next, this esophageal extension is symmetrically enveloped by the gastric wall, creating a cuff, the upper part of which is fixed to the esophagus.
Nissen method
The Nissen method is the most common in the surgical treatment of unfixed and paraesophageal hernias of the esophagus. The basis of the operation is the formation of a cuff from the walls of the fundus of the stomach, enveloping the abdominal esophagus from all sides. If the esophageal opening of the diaphragm is very large, then a prosthesis made of non-absorbable synthetic material is installed.
Treatment
An important condition for treatment is patient compliance with the general and dietary regimen. Heavy physical work, wearing tight belts and bandages that increase intra-abdominal pressure are contraindicated for them. The patient should sleep with the head of the bed elevated. A mechanically and chemically gentle diet, split meals (5–6 times a day) are indicated. The patient should take his last meal 3–4 hours before bedtime. Smoking, alcohol abuse, and coffee are contraindicated (they reduce the tone of the lower esophageal sphincter).
Surgical treatment is recommended in the following cases:
- in the absence of effect from conservative therapy in patients with severe symptoms of the disease;
- with severe reflux esophagitis, accompanied by bleeding, anemia, ulcerative esophagitis;
- with peptic stricture of the esophagus;
- with giant (subtotal and total) gastric hernia;
- when a sliding hiatal hernia is combined with other diseases of the upper digestive tract requiring surgical treatment (cholelithiasis, peptic ulcer, etc.).
According to the literature, about 10–20% of patients with this pathology undergo surgical treatment. As for the essence of surgical interventions used to eliminate sliding hernias, they are aimed primarily at restoring the closing function of the cardiac part of the stomach and closing the hernia defect. The most successful option for solving this problem is considered to be the Nissen fundoplication operation: creating a 360° cuff from the fundus of the stomach around the cardiac part of the esophagus and fixing it to the sutured legs of the diaphragm. This operation has recently been performed laparoscopically.
Endoscopic surgeries for axial hiatal hernias
Most often at present, laparoscopic methods are used in operations for axial hernia of the esophagus. The main advantages of laparoscopy are minor trauma and a short rehabilitation period.
During laparoscopy, 4 punctures are made in the abdominal wall to insert the laparoscope and instruments. Next, the abdominal organs are moved into the anatomically correct position, the distended hernial opening is sutured, and fundoplication is performed using the chosen method. During laparoscopic operations, the risk of relapse is minimal, and by prescribing additional drug therapy, negative consequences can be minimized.
With laparoscopy, as with any other operation, there may be complications:
- bleeding;
- perforation of internal organs;
- damage to the vagus nerves;
- due to irritation of the subdiaphragmatic region and peritoneum, pain in the back and left shoulder may occur.
Despite this, laparoscopy is an effective surgical method for treating hiatal hernia. With the right approach and appropriate qualifications of the surgeon, the risk is negligible.
In the most equipped surgical clinics, the endoscopic method is now used using a special Esophyx device. The device is inserted through the mouth, with its help an acute angle of His is formed, as well as a cuff at the junction of the esophagus and stomach.
Goals and objectives of surgical intervention
There are about 40 types of operations, each of which has its own disadvantages and positive aspects. The required surgical method to be performed is chosen by a specialist in each specific case. In this case, the data of preliminary examinations are taken into account, since most often the operation has to be planned.
The main objectives of surgical treatment are:
- return of organs to their normal anatomical position, i.e. elimination of the hernia;
- formation of an anti-reflux mechanism in order to prevent acidic stomach contents from entering the esophagus and the development of esophagitis;
- creation of an acute esophagogastric angle.
What are the consequences after surgery for hiatal hernia?
In some cases, complications may arise during surgery to remove a hiatal hernia, immediately after it, or after some time.
All complications are divided into:
- Intraoperative – consequences that arise during the operation. Bleeding from parenchymal organs, gastric vessels, diaphragm.
- Perforation of the esophagus, stomach.
- Damage to the trunks of the vagus nerves.
- Bleeding.
Symptoms and course
Often, a hernia does not manifest itself in any way and is defined as a “finding” when examining the stomach for other diseases. The classic version is represented by reflux esophagitis syndrome: spontaneous pain or when bending forward, pain in the lower third of the sternum or behind it, radiating upward or to the back, heartburn of varying intensity when the patient is lying down, which goes away if he sits or stands up, hiccups, belching of air. The most serious complications are strangulated hernia and bleeding from formed ulcers of the esophagus or stomach.
Early postoperative period
After surgery for a hiatal hernia, pain and swelling may persist in the operated area for several days. Edema narrows the lumen of the esophagus, which can cause transient dysphagia. Therefore, for several days the patient may feel that food is not passing well. Due to transient gastrointestinal motility disorders, intestinal problems may occur. The body's reaction to surgery may be an increase in temperature to low-grade levels; this does not require any treatment and goes away on its own.
In the postoperative period, antibiotics and painkillers are prescribed; in case of gastrointestinal motility disorders, prokinetics are prescribed.
Already on the first day the patient can get out of bed and drink fluids. The sutures are removed on the 7th day, after which the patient is discharged from the hospital.
What can you eat immediately after surgery?
Nutrition after surgery for hiatal hernia is the same as after other abdominal surgical procedures.
On the first day, you are allowed to drink a little water (up to 300 ml).
On the second day, you are allowed to eat some liquid food (mashed soup with vegetable broth, a portion of liquid porridge with water).
The operated patient is gradually transferred to diet No. 1 according to Pevzner; all foods that cause irritation and flatulence should be excluded from the diet. Food should be warm and soft. The patient should adhere to this diet for 1-2 months.
Postoperative period
As a result of laparoscopy for a hiatal hernia, 3 or 4 incisions are left on the skin in the abdominal area. Their length can range from 5 to 10 mm. From the first day, patients can get out of bed and drink. On the second day, warm liquid food is allowed.
Patients are discharged from the first to the sixth day: the specific timing is determined by the severity of the disease.
After 14-20 days, the operated patient can return to work.
A strict diet is prescribed for approximately 2 months, and a softer one lasts up to six months.
After this, there is generally no need to follow a diet or take medications.
Rehabilitation after hiatal hernia surgery
If the patient underwent laparoscopic surgery and there were no complications, then the sick leave is closed after 7 days, unless the work involves heavy physical exertion. However, the rehabilitation period does not end there.
The duration of the rehabilitation period after surgical removal of a hiatal hernia depends on the compensatory capabilities of each individual patient, as well as the traumatic nature of the intervention.
During the rehabilitation period, you should adhere to diet No. 1 according to Pevzner for at least 2 months, with its subsequent expansion under the supervision of a doctor. You need to eat at the same time, in small portions, increasing the number of meals. Food should be warm, boiled (or steamed).
Depending on the method used to perform the operation, the intensity and duration of pain may vary. Thus, during laparoscopic operations, the patient experiences virtually no pain after discharge from the hospital, whereas during abdominal operations, the pain can be prolonged and severe, knowing this, doctors prescribe painkillers.
As for physical activity and sports, they are allowed no earlier than 2.5 months after surgery, if there are no complications.
It is very important to avoid alcohol consumption and smoking.
If the operation was successful and the patient carefully followed all medical recommendations, then after 9-12 months the body will fully recover and the patient can return to normal life.
Exercises during the rehabilitation period
After surgery to remove the hiatal hernia, under the guidance of an instructor, therapeutic exercises begin on the first postoperative day in the supine position. The instructor shows how to properly inflate a balloon, do cough exercises, self-massage of the legs, arms, and abdomen. As the motor mode expands, the movements become more varied, the starting position changes, and the number of repetitions increases. The motor mode includes going up and down stairs, measured walking in the park.
The main objectives of therapeutic exercises are reduced to prevention:
- bronchopulmonary complications;
- thrombosis;
- intestinal paresis;
- contractures of the shoulder joint.
Preparing for surgery
In preparation for surgery, the patient must undergo a comprehensive examination. He is given an x-ray of the peritoneal organs , the level of acidity of gastric juice , and manometry of the esophagus . Urine and blood tests are required. A therapist, a cardiologist, and an endocrinologist are being examined. A consultation with an anesthesiologist is carried out.
Typically, reviews after hiatal hernia surgery are positive. The patient needs to familiarize himself with them, setting himself up mentally for a positive outcome. The psychological state at the time of intervention plays an important role. The patient should understand that a meager number of deaths due to surgery has been recorded. But in the absence of it, the risk of death is quite high.
Progress of laparoscopic intervention according to Nissen
So, if it is necessary to perform laparoscopic surgery , using the Nissen method, the surgeon makes four to five punctures in the anterior wall of the peritoneum. This is necessary for insertion of endoscopic instruments. Next, carbon dioxide is supplied to the abdominal cavity, expanding its walls (so that the surgeon has room to “turn around”).
The diaphragm is lowered here and sutured. The walls of the stomach are wrapped and secured around the distal (lower) portion of the esophagus. A so-called cuff is formed, which is sewn to the leg of the diaphragm.
All displaced organs are returned by the surgeon to their places (from the chest cavity to the peritoneum). When the anatomical order is established, the instruments are removed. The puncture sites are sutured. The whole procedure takes an hour and a half to two. It is performed under general anesthesia.
Nutrition after surgery for hiatal hernia
The operated person must follow a strict diet for 8 weeks. The diet after hiatal hernia surgery should correspond to table No. 1 according to Pevzner. The diet is prescribed by the gastroenterologist who supervises the patient after the operation, and only he can make changes to it. All products must be fresh and high quality, without preservatives or flavoring additives. It is very important to establish a food intake routine. You need to eat regularly, at the same time, in small portions and often.
After 8 weeks, the diet begins to expand. This process is gradual, requiring the patient’s attention to his health. If any foods cause pain or heartburn, you should avoid them. Only moderation and gradualism will enable a patient who has undergone removal of a hiatal hernia to move to a general diet without harming his health.
Diet and nutrition before and after surgery
- If you have a hiatal hernia, split meals in small portions are recommended.
- You can have dinner no later than 3 hours before bedtime.
- After eating, you should sit or move around (about an hour). Movement stimulates the evacuation of food from the stomach and reduces the manifestations of gastroesophageal reflux.
- It is not recommended to drink between meals.
- Carbonated drinks should be avoided.
- You can't overeat.
- Products that contribute to increased gas formation should be excluded from the diet: cabbage in any form, legumes, black bread, grapes, fermented milk products, milk: their consumption leads to an increase in intra-abdominal and intragastric pressure, which provokes the reflux of gastric contents into the esophagus.
- In case of exacerbation of esophagitis, the so-called “esophageal table” is prescribed. It includes: butter, soft-boiled eggs, sour cream, liquid or pureed cottage cheese, vegetable soups (mashed), porridge, meat or fish soufflé, soaked crackers, grated or baked apples.
- Do not consume: fruit juices with a sour taste, soda, alcoholic drinks.
- Spicy seasonings are prohibited.
The diet after hiatal hernia surgery is almost similar to other recommended post-operative nutrition systems.
- First day: you can drink a small amount of water (up to 300 ml).
- Second day: you are allowed to eat a small portion of liquid food - preferably low-calorie soup.
- As the body recovers, the diet is enriched with soft foods that easily move through the esophagus.
- Returning to a normal diet is allowed only with the permission of the attending physician. The main principles in this regard should be consistency and moderation.
- The temperature of the foods consumed is also important: keeping it within normal body temperature is optimal. The reason for this requirement is that after surgery, edema of the cardia often develops, making it difficult for the food mass to move at higher or lower temperatures.
Surgery for hiatal hernia: pros and cons
Surgical treatment of hiatal hernia is carried out according to strict indications, when refusal to operate threatens the life and health of the patient. In recent years, many randomized studies have been conducted to identify the frequency of complications of the hiatal hernia and relapses of the disease during abdominal and laparoscopic operations, to identify complications when using various surgical modifications, taking into account both early and long-term complications.
As a result, a clear priority of laparoscopic operations over abdominal operations was revealed. A good clinical effect of laparoscopy for removal of the hiatal hernia was noted in almost all cases. Relapses of the disease were observed only in isolated cases. Transient dysphagia (up to 1 month) is more often observed with circular fundoplication.
Patients' lives, even after successful surgery, should be free of what caused the disease. Patients should:
- eat regularly and properly,
- avoid physical and mental stress;
- get a good night's rest,
- exclude alcohol and smoking.
If your doctor recommends surgery, there is a good reason for it. In this case, you should not refuse.
What causes the problem?
A number of reasons are cited as predisposing factors to the development of a hiatal hernia. These include chronic constipation, age-related changes, bad habits, lack of exercise in life, genetics, excess weight and problems with the spine. For example, genetic predisposition, if one of the relatives had such a problem, gives a 25% risk of developing this pathology. Situations that provoke an increase in intra-abdominal pressure are also considered risk factors. This may include intestinal upset, coughing, screaming, childbirth and heavy lifting.