Nursing process is an approach of nursing staff to patient care, based on science and many years of experience. The nursing process for pancreatitis has distinctive features due to the nature of the disease. Exacerbation of pancreatitis is accompanied by severe pain, which is why patients end up in the hospital. A qualified approach on the part of nurses and nurses is designed to provide competent care for the patient, meeting his immediate needs and the optimistic atmosphere necessary for a speedy recovery.
Responsibilities of a nurse
An inflamed pancreas is a serious disease that can even lead to death. After admission to the hospital, a seriously ill patient requires an attentive, caring attitude from the medical staff. Nursing care for pancreatitis is an integral part of successful patient treatment. After a diagnosis has been made and medications prescribed by a doctor, nursing care is needed to monitor the patient’s condition and compliance with medical orders.
First of all, the nurse provides assistance aimed at relieving acute pain and ensuring peace for the patient. Next, a nursing process map is created and gradually filled out. To do this, the nurse asks questions to the patient or his relatives about the possible cause of the disease, lifestyle, and habits of the sick person. Nursing diagnosis of the disease consists of measuring physical indicators of the patient’s condition - temperature, pressure, tests.
When the necessary information is collected, the main and potential problems are identified, based on the medical literature, a treatment plan is developed to meet the needs and recovery of the person.
Nursing staff are responsible for the timely implementation of the necessary medical measures - they put in IVs, give injections, monitor compliance with diet and rest, and help those weakened by the disease undergo examinations and procedures.
Features of the disease in acute and chronic forms
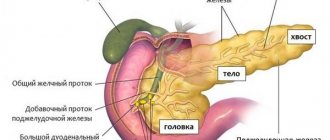
In addition to other possible causes of acute pancreatitis, 70% are due to alcohol abuse. Inflammation of the pancreas leads to spasm of the ducts, due to which the produced enzymes do not exit into the intestines, but begin to digest the pancreas itself, destroying it. This leads to severe pain and hospitalization. The greatest relief comes from applying ice to the pancreatic area, which slows down the rapid development of the process.
The patient will need bed rest and complete abstinence from food for 2-3 days. It is only allowed to drink warm boiled or mineral water, but without gas, or rosehip decoction.
After relief of the condition, the patient is recommended to diet No. 5 with less proteins, fats and carbohydrates. Food must be warm, not hot or cold, boiled, for example, steamed, or grated.
After recovery, the patient should ask the doctor about the amount of physical activity allowed.
Under unfavorable factors, exacerbations and attacks of the disease occur. Often repeating, they turn into a chronic form of pancreatitis with the same symptoms of the disease. The main difference between the chronic form is the strong destructive consequences on surrounding organs. This is associated with a wider range of treatment procedures and long-term treatment.
What is the nurse's help with inflammation of the gland of both forms?
Nursing care for pancreatitis in the first days after the patient’s admission to the hospital is focused on eliminating his serious condition, as well as providing maximum rest to the inflamed gland, and eliminating painful signs.
Let us consider in more detail what the nurse’s help is in the acute and chronic phases.
Treatment of acute pancreatitis first of all begins with primary actions aimed at saving human life. In the event of a severe attack of the disease, the patient is taken by ambulance to the hospital, where he is prescribed bed rest and given rest.
The nurse's treatment plan for acute pancreatitis includes:
- Applying ice to the area where the pancreas is located.
- When chills occur, and if necessary, wrap the person up.
- Give painkiller injections.
- Monitor fluid intake and how fast you observe for the first 3 days after a relapse.
- A conversation with the patient’s family about the need for a strict diet, as well as about giving up bad habits.
- superior pancreaticoduodenal artery - branch of the gastroduodenal artery;
- inferior pancreaticoduodenal artery - branch of the superior mesenteric artery.
B) The body and tail of the pancreas receive blood from the splenic artery.
a) formation and release into the duodenum of a transparent secretion from the puddle reaction (pH-7.5-9.0) with a volume of 1.5-2 liters;
b) composition of pancreatic secretion: water (98-99%), proteins, sodium, potassium, calcium, bicarbonates, enzymes;
c) bicarbonates - protect the mucous membrane of the duodenum from the action of acidic gastric contents, create alkaline sir in its cavity and optimal conditions for digestion;
d) the action of enzymes is aimed at once inoculating food ingredients (trypsin and chymotrypsin - break down proteins into amino acids, lipo - hydrolyzes neutral fat into fatty acids and glycerol, amylase - breaks down carbohydrates into dextrose).
a) secretion of the hormone insulin, which regulates glucose metabolism;
b) secretion of the hormone glucagon, which is an insulin antagonist (glucagon secretion is suppressed by glucose);
c) secretion of protease inhibitors.
Nurse's help with acute and chronic pancreatitis
Acute pancreatitis is a serious physical condition in which collapse is possible - a drop in blood pressure, deterioration of blood circulation, as a result of which the extremities become cold, severe weakness and fainting appear. The task of the medical staff is to eliminate the crisis, severe pain, and provide rest to the diseased organ.
The nurse gives pain-relieving injections and places a cold heating pad or ice in the pancreas area. Thanks to this, the physiological processes of the organ are suspended, inflammation is relieved, and pain is reduced. If the patient is shivering, this is not a reason to cancel the cold. They wrap him in an extra blanket and place a warm heating pad on his feet.
The patient is provided with bed rest and complete rest. He will need eight to nine hours of nightly rest each day to recover. The nurses make sure nothing bothers him and give him sleeping pills if necessary.
The nurse's duties include:
- monitor the drinking, eating and rest regime,
- monitor the intake of prescribed medications,
- give injections, IVs,
- measure temperature, pulse, blood pressure daily,
- monitor general health, timely bowel movements,
- help with mobility if necessary,
- explain to the patient the importance of following instructions,
- provide relatives with information about the need for a diet during an exacerbation of the disease and careful attention to nutrition in the future.
Acute pancreatitis is often accompanied by vomiting, so the nurse provides the patient with a container for vomit, water, wipes, and means of communication with medical staff in case of emergency.
If a person's condition does not improve or, on the contrary, worsens, surgery may be required.
The nursing process for chronic pancreatitis is similar to the nursing process for acute illness. It differs in that the chronic form is characterized by frequent relapses; the disease also negatively affects surrounding organs, which is why they are destroyed. The goal of treatment for a chronic disease is to resume the functioning of the pancreas and prevent actions that provoke an exacerbation. This approach will require significantly more time and treatment procedures.
Due to lack of knowledge about the course of the disease, the patient or his relatives may experience fear of the future or dissatisfaction with the treatment methods used. In this case, the nurse should try to explain the issues raised in a friendly and tactful manner and offer relevant medical literature for review.
Coursework acute pancreatitis nursing
- 0.1 Description
- 0.2
The patient should be protected from psychological experiences and stress; anxiety and irritating factors are completely excluded.
The pulse and frequency are constantly monitored, blood pressure is measured, preferably in both arms, body temperature in the armpit, the tolerance of food taken by a person, the frequency of physiological waste (stool) and its consistency are important. An important conversation is during which the patient learns about his disease and the prevention of exacerbation.
Bring the patient's relatives and loved ones up to date and ensure their understanding of patient care.
| Code | 392088 |
| date of creation | 2018 |
| Pages | 35 |
| Purchasing finished works is temporarily unavailable. |
The course work is intended for the “Nursing” department. PM.02 Participation in treatment, diagnostic and rehabilitation processes
MDK 02.02 Fundamentals of rehabilitation
Defense of course work for 5. .
1. Theoretical part 1.1. Definition, classification of chronic pancreatitis……….……5 1.2 Etiology, pathogenesis of chronic pancreatitis…. 6 1.3.
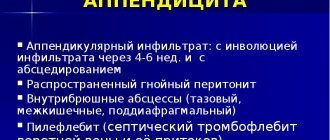
Risk factors and their influence on the development of chronic pancreatitis…………………………………………………………………………………. 7 1.4. Clinical manifestations of chronic pancreatitis………………. 8 1.5. Possible complications of chronic pancreatitis……….……….
10 1.6. Diagnosis of chronic pancreatitis……………..…………. eleven
1.7 Treatment and prevention of chronic pancreatitis………………. 12
2. Practical part 2.1. Questionnaire to identify risk factors for the disease in a patient with chronic pancreatitis……………………………………………………….…..…. 14 2.2. Care plan for a patient with chronic pancreatitis………. …. 15 2.3. Patient preparation plan for SIA.
……………………………..……..17 2.4. Reminders for patients with chronic pancreatitis………..…. …..21 2.4.1.Principles of therapeutic nutrition………………………………..…. 21 2.4.2.Regimen of physical activity……………………………..…..22 2.4.3.Rules for taking prescribed medications……….
23
2.5. Recommendations for relatives on organizing care for the patient at home………………………. …………..……………….…. 25
Review of medical educational literature on nursing care for patients with chronic pancreatitis. Analysis of the features of organizing nursing care for patients with chronic pancreatitis in the therapeutic department, recommendations for its improvement
| Heading | Medicine |
| View | abstract |
| Language | Russian |
| Date added | 13.06.2015 |
| file size | 206.9 K |
Send your good work in the knowledge base is simple. Use the form below
Students, graduate students, young scientists who use the knowledge base in their studies and work will be very grateful to you.
Posted on https://www.allbest.ru/
Federal State Budgetary Professional Educational Institution
(Federal State Budgetary Educational Institution “Medical College”)
Theme of the course work
Nursing care for patients with chronic pancreatitis
3rd year student 35gr.
Radjabova Anfisa Alievna
Head: Sharocheva M.A.
- Chapter 1. Review of medical educational literature on nursing care for patients with chronic pancreatitis
- 1.1 Organization of nursing care for patients
- 1.2 Brief characteristics of chronic pancreatitis
- 1.3 Organization of work of a nurse with patients with chronic pancreatitis
- Chapter 2. Analysis of the features of organizing nursing care for patients with chronic pancreatitis in the therapeutic department
- 2.1 Characteristics of the therapeutic department
- 2.2 The main problems in the work of nurses in the therapeutic department and ways to improve their work
- Bibliography
chronic pancreatitis nursing care
Adjacent to these two important etiological groups is the third pathology of the area of the large duodenal sphincter (papillitis, sphincteritis, diverticulitis, etc.) and the duodenum (peptic ulcer, erosion, gastroduodenitis).
The fourth smallest group combines various causes, in particular, pancreatic injuries, pancreatotoxic drugs (sulfonamides, tetracycline, chlorothiazide, furosemide, immunosuppressants, anticoagulants, indomethacin, brufen, estrogens), viral infections (hepatitis B and C virus, mumps virus, hyperlipidemia, hyperparathyroidism and others).
a) exacerbation (clinically manifested by pancreatic colic, morphologically - autolysis of acinar tissue of the pancreas)
b) incomplete remission
c) remission (absence of pain)
2. Course: mild, moderate, severe (determined by the severity of the course, the next relapse and the frequency of relapses)
The course of chronic pancreatitis can be divided into three stages
In the first (initial stage, or period, lasting up to 10 years, there is an alternation of exacerbations and remissions, the main manifestation is pain of varying intensity and localization, depending on the damage to areas of the pancreas; dyspeptic syndrome is concomitant and is the first to disappear with treatment.
Source: https://vladivostok-vrachi.ru/kursovaja-rabota-ostryj-pankreatit-sestrinskoe
Stages of monitoring a patient with pathology
The nursing process for acute pancreatitis contains several stages of observation and qualified care for the patient:
- examination, examination
- diagnostics,
- intervention planning,
- intervention,
- grade.
What is done in the first stage
The first stage is called the nursing examination. It contains the collection of information about the sick person, his life, work, habits, heredity to determine the cause of the disease. If the patient is unable to provide the necessary information, the nurse communicates with relatives. After this, she records blood pressure and heart rate, determines whether the patient has a fever, and takes blood and urine tests. All information is recorded in the nursing medical record.
The nurse monitors the patient’s intake of medications prescribed by the doctor, and sets up emergency communications if the patient suddenly feels worse.
Features of the second stage
The second stage - nursing diagnosis - is aimed at identifying the needs and problems of the patient, a potential danger to human life.
- Presence of pain, nausea or other signs of pancreatic enzyme toxicity,
- prostration,
- heartburn, flatulence,
- sleep disorders, mental state.
At the same time, the nurse monitors the regular intake of prescribed medications, compliance with the diet, and ensures communication with the medical staff in case of vomiting or deterioration of health.
Main tasks of the third stage
At the third stage, the goals and objectives of nursing care are determined. The nurse's action planning is carried out on the basis of methodological literature describing treatment regimens for pancreatitis in acute and chronic forms, as well as therapeutic actions aimed at improving the patient's health.
Among other measures to prevent exacerbation of pancreatitis, food control plays a leading role.
The work of a nurse does not replace the work of a doctor, but without it, treating patients is not possible. The nurse creates a unique atmosphere of care in a medical facility, helping patients not to lose hope and teaching the principles of a healthy lifestyle.
1