Gangrenous appendicitis and peritonitis
At the next stage, acute gangrenous appendicitis develops with ICD code 10 as in another disease.
The shoot actually dies. As the gangrenous process develops, pain receptors stop working, and the patient feels that his condition has improved. The temperature may drop slightly. However, this is followed by the most dangerous phase - the perforative phase. The appendix ruptures and its purulent contents spill into the abdominal cavity. An area of appendicular infiltrate forms around and a periappendiceal abscess begins, quickly turning first into limited and then acute generalized peritonitis. The patient's condition worsens so quickly that it may be late to see a doctor. Peritonitis in a generalized form leads to the death of the patient within a day.
Causes
Acute appendicitis, other and unspecified (k35.8)
Gangrenous-perforated appendicitis is one of the stages of inflammation of the appendix. The reason why the appendix becomes inflamed is artery thrombosis. The next stage is the development of harmful bacteria in the intestinal microflora.
The danger is:
- cocci;
- bacteroides;
- coli;
- enterococci.
Destructive changes characteristic of the initial stage of inflammation of appendicitis:
- Reduced protection of the mucous membrane of the appendix and local immunity.
- Disturbances in the outflow of digestive tract contents from the appendix.
- Loss of elasticity of the walls of the appendix.
As the disease develops into a severe - gangrenous stage, the patient's condition deteriorates sharply. Sometimes gangrenous inflammation occurs without previous stages, as an independent disease.
This is due to:
- Circulatory disorders in the appendix.
- Lack of fiber in the daily diet.
- Formation of cholesterol plaques in the gastrointestinal tract.
- Vessel thrombosis of the appendix.
These data indicate that the main reason for the development of complications is poor circulation in the appendix. Other factors: infections associated with the development of harmful microflora, impaired outflow of food masses and immune autoaggression - are secondary factors and contribute to the development of gangrene, but do not provoke it.
Delayed assistance leads to purulent melting of the walls of the appendix, and the patient dies.
Nature of the problem and reasons for its occurrence
Acute appendicitis. appendicular infiltrate (page 1 of 5)
Inflammation of the appendix has been thoroughly studied by modern medicine, and its symptoms have been described in scientific publications, over 120 in the last century alone.
But ignoring the signs of the disease and self-medicating at home can also lead to the development of a dangerous stage of phlegmonous appendicitis, which inevitably occurs in the development of the process without proper intervention.
Inflammation of the appendage of the cecum is a common occurrence in women, due to the peculiarities of their anatomical structure.
In the abdominal cavity of the female half of humanity there are more organs that can provoke a pathological process.
There are many reasons for the development of inflammation in the appendix, sometimes they create a cumulative effect, so assumptions about the nature of the inflammation can be very variable:
- the presence of bacterial infection or parasites in the body;
- blockage of the appendix lumen with various substances, foreign bodies, food debris (small parts of toys for children, seed husks, feces, fruit pits);
- the development of inflammation against the background of other negative processes in the abdominal cavity, ultimately leading to the initial stage of development of acute appendicitis.
Acute appendicitis is a disease that is difficult to recognize and dangerous, often disguised as the manifestation of acute pathologies of the gastrointestinal tract and genitourinary system, with symptoms that are considered to appear in the abdominal area, on the right side, and can be guided by this common sign.
However, appendicitis belongs to the category of dangerous diseases not only due to the manifestation of uncharacteristic symptoms, but also due to the peculiarities of the anatomical structure of the organ.
During an acute abdomen, the patient usually focuses on pain on the right side as the most likely symptom.
But the appendix can be located in the pelvis, near the gallbladder and liver, and even in front of the stomach, with a mirror arrangement of internal organs, which occurs in some patients.
The size of the appendix in different people is also a variable concept, since cases from 1 cm to up to 30 cm have been noted in different people during autopsy or surgery.
Acute appendicitis - symptoms and treatment, diagnosis, complications, prevention
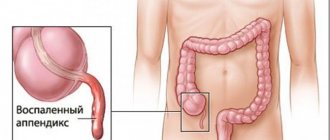
Acute appendicitis is a process of inflammation of the appendix - the formation of the cecum, which is one of the common pathologies of the abdominal cavity. In the international classification of diseases for acute appendicitis, the ICD-10 code is K35.
This disease can occur in patients of different ages. However, it is most often diagnosed between the ages of 20 and 40, and women are affected twice as often as men.
Forms
According to the clinical and morphological classification, clinicians distinguish several forms of the disease.
By location it is:
- Typical.
- Atypical (ascending retrocecal, descending pelvic, medial and subhepatic).
According to the stage of disease development:
- Simple (superficial, acute catarrhal).
- Destructive (phlegmonous, perforated, gangrenous);
- Complicated (with appendiceal abscess, with appendiceal infiltrate, with diffuse peritonitis and other complications).
Causes and risk factors
Until now, the exact causes of acute appendicitis have not been established. However, the main route of infection is enterogenous (entry of the infectious agent through the lumen of the appendix).
The development of inflammation can be triggered by the following factors:
- infectious diseases (yersiniosis, amoebiasis, intestinal tuberculosis, etc.);
- disruption of intestinal innervation;
- activation of the intestinal microflora caused by congenital anomalies of blockage or development of its lumen (fecal stones, various parasites, neoplasms, foreign bodies, etc.);
- immunological disorders, including allergies;
- diseases that provoke inflammation of the walls of blood vessels;
- abdominal injuries;
- regular unbalanced diet;
- bad habits;
- intestinal dysbiosis.
The risk of developing the disease increases significantly in pregnant women, this is due to the enlargement of the uterus, which leads to displacement of the cecum and appendix. In addition, constipation, changes in the blood supply to the pelvic organs, and restructuring of the endocrine system contribute to the development of the pathological process during pregnancy.
Symptoms
The very first sign indicating the development of this pathology is abdominal pain. After which other manifestations appear.
https://www.youtube.com/watch?v=6P0FnAv3EpE
The disease manifests itself differently in women and men. Also, its course differs in different age groups of people.
| SYMPTOM | In adults | In the elderly | In children | In pregnant women |
| Abdominal pain | An attack of appendicitis begins with the appearance of characteristic pain in the navel area (epigastric region), after which it moves to the lower region of the right side of the abdomen. There are disturbances in stool and sleep | Depending on the trimester, pain appears in the navel area, in the last weeks of pregnancy - in the hypochondrium | ||
| Temperature | Low-grade fever or up to 37˚С, in the last stages – above 39˚С | Due to age-related changes, it may not rise | Above 38-39˚С. At the last stage of the inflammatory process up to 40˚C | Up to 38˚С |
| Chair | Bloating, often diarrhea (loose stools) and flatulence, in rare cases constipation | |||
| Language |
| |||
| Nausea | Constant | |||
| Vomit | Single or 2-fold | Single or 2-fold | Children's appendicitis is usually accompanied by repeated vomiting | As a rule, multiple (depending on the location of the process) |
| Urination | Dysuric disorders (frequent urge to urinate) may often occur. | |||
| Pul | rapid |
What diseases can be confused with?
This pathology is similar in clinical signs to many diseases that are characterized by pain of various etiologies in the right side.
Therapeutic diseases:
- gastroenteritis;
- diabetic ketoacidosis;
- lower lobe pneumonia;
- porphyria.
Surgical:
- acute cholecystitis;
- pancreatitis;
- perforation due to peptic ulcer;
- intussusception;
- intestinal obstruction;
- hernia;
- mesodenitis;
- Meckel's diverticulum.
Urological:
- renal colic;
- urinary tract infections;
- pyelonephritis on the right.
Gynecological diseases:
- ovarian apoplexy;
- salpingo-oophoritis;
- ectopic pregnancy.
In this case, a differential examination should be carried out within a certain time frame, since an “acute abdomen” is a symptom that threatens the patient’s life.
Differential diagnosis
When collecting anamnesis, the history of the patient’s illnesses (existing or past) is important, since among them there may be those that mimic the clinical signs of acute appendicitis.
Typically, the diagnosis is made during a physical examination. The presence of the disease is indicated by a number of abdominal symptoms:
- in the position on the left side, the pain on the right is greatly intensified;
- the distance between the navel and the right anterior spine is less than on the left side (the reason is muscle contraction on the right);
- painful sensations in the iliac region on the right and upon percussion;
- when the abdomen is pulled in, the pain intensifies somewhat;
- body temperature in the right armpit is 1-2 degrees higher than in the left armpit.
Ultrasound is one of the important stages in diagnosing appendicitis. It allows you to detect the absence of peristalsis, the presence of free fluid, signs of peritonitis, blockage of the lumen and expansion of the appendix.
If the information received is not enough, specialists resort to magnetic resonance imaging and abdominal radiography.
Young children may require additional examination - electromyography of the anterior abdominal wall.
A general blood test in patients with this disease reveals nonspecific inflammatory changes.
In complex diagnostic cases, they resort to the method of diagnostic laparoscopy, which, if the diagnosis is confirmed, is transferred to therapeutic (appendectomy is performed during the diagnostic procedure). Determining the etiological factor that caused the pathology is possible by performing histology of the removed appendix.
Differential diagnosis is carried out with diseases such as acute cholecystitis, gastritis, cholelithiasis, gastric ulcer, pancreatitis, renal colic, acute cystitis, ectopic pregnancy, acute orchiepididymitis, neoplasms and other pathologies that can cause the development of an “acute abdomen”.
In rare cases, a rectal and/or vaginal examination is performed for differential diagnosis. The presence of a neoplasm of the cecum can be excluded or confirmed using the colonoscopy method.
Treatment
The only treatment option is surgery to remove appendicitis, which in medical terminology is called an appendectomy. It is done using the classic surgical method through one incision or through three small incisions (length does not exceed 1 cm) using laparoscopy. The decision about which method of surgery is most suitable depends solely on the form of appendicitis.
Preparing for surgery
Often surgery to remove the appendix is performed as an emergency. Emergency care can follow within 1-2 hours after the patient’s admission to the surgical department of the hospital. In some cases there is no time for special preparation. An appendectomy can last from 40-50 minutes to several hours. The duration of the operation directly depends on whether there are complications.
If time before the intervention allows, patient preparation includes:
- examination of the cardiovascular system (ECG);
- cleansing the stomach (most often the patient does not drink or eat anything, so this is done extremely rarely);
- hair removal in the area of manipulation;
- the patient is administered an isotonic solution intravenously to eliminate symptoms of intoxication, as well as to prevent dehydration;
- determining which anesthesia is suitable for the patient (checking for lack of reaction to painkillers);
- skin disinfection.
For uncomplicated disease, laparoscopic appendectomy is most often used. A laparoscope is inserted through an opening in the abdominal wall, which provides access to the appendix. The space in the abdominal cavity is filled with a special gas (pneumoperitoneum), after which the appendix is removed under visual control (the laparoscope is equipped with a micro-camera and a cold light source).
The camera transmits an image of the surgical field to a monitor installed in the operating room. This method is the most modern and allows you to avoid unnecessary blood loss and trauma. Also, the advantages of this method include a shorter postoperative period and the absence of a large postoperative scar.
In case of complications of acute appendicitis, for example, diffuse peritonitis, laparotomy with a thorough examination of the abdominal organs is indicated.
Possible complications
Appendectomy is considered a relatively safe operation, but, despite the positive trends, various complications cannot be excluded. The death rate for simple appendicitis is 0.8-1% per 1000 cases.
Wound infections
Such complications arise during intraoperative contamination with pathogenic microorganisms. The development of this complication is within 5% in cases of simple appendicitis, and in cases of perforation of the appendix or gangrene – up to 20%. The use of antibacterial drugs in the preoperative period significantly reduces the likelihood of wound infections.
Chronic appendicitis
The number of cases of this form of pathology in general is no more than 1.5%. As a rule, this pathology develops after an attack of acute appendicitis.
Scars and adhesions that narrow the lumen of the appendix or an infection remaining after surgery can contribute to its occurrence. During periods of temporary recovery (remission), no clinical signs are observed.
To prevent the occurrence of an inflammatory process, patients are recommended to undergo a planned appendectomy.
Appendiceal infiltrate
This complication is expressed in the form of compaction, which in most cases occurs 3-4 days from the onset of the disease.
It is easily palpable and is formed as a result of enveloping the appendix with intestinal loops or peritoneum. At the same time, the bright symptoms characteristic of ordinary appendicitis are blurred.
Body temperature is within normal limits, rarely low-grade, pain is mild.
This complication can be easily diagnosed using ultrasound and CT. However, a careful differential analysis should be carried out regarding tumor processes, in particular in elderly people. With adequate antibacterial therapy, appendiceal infiltration can be cured without surgery, but a high risk of relapse remains.
Intra-abdominal abscess
An abscess of the pelvic cavity (intra-abdominal abscess) develops in the case of total infection, for example, with perforation of the appendix.
With this complication, fever occurs and diagnostic signs of ultrasound or CT examination are present. In some cases, abscesses may need to be treated with drainage techniques.
With the use of preventive antibiotic therapy, the incidence of this complication is significantly reduced.
Appendiceal abscess
This form of complication is suppuration, which is accompanied by pronounced tachycardia, fever and leukocytosis. In most cases, the abscess is localized in the right iliac region, rarely in the pelvic cavity.
For this pathology, a rectal examination is performed; it is highly informative and is confirmed by ultrasound and CT studies. The patient is prescribed open surgical treatment and a drainage system is installed.
Appendicitis and pregnancy
Appendectomy is the most common non-obstetric procedure during pregnancy. The frequency of such cases is 0.15% - 2.0% per 1000 pregnant women. A recent large-scale study showed that during pregnancy the risk of developing appendicitis is exactly the same as in non-pregnant women.
Often, displacement of the appendicular process significantly complicates diagnosis due to an increase in the size of the uterus, and appendicitis is mistaken for the onset of labor. In this case, uncharacteristic clinical manifestations are possible: nausea and vomiting with nagging pain in the abdominal cavity on the right.
According to statistics, in cases of simple appendicitis (without complications), maternal mortality is low, however, it increases with perforation of the appendix to 4%. The threat to the fetus is 0-1.5% with simple appendicitis, with perforation - 20-35%.
Prevention
There is no specific prevention for this pathology. In order to prevent the disease, experts recommend: giving up bad habits, a nutritious balanced diet and strengthening the immune system.
Source: https://medcatalog24.ru/gastroenterologiya/ostryj-appenditsit/
Diagnostics
Diagnostic criteria
The clinical picture of acute appendicitis depends on the location of the appendix in the abdominal cavity, the reactivity of the body, the stage of the disease and the presence of complications.
A typical picture of acute appendicitis is characterized by an attack of pain in the right iliac region with a pronounced local and general reaction of the body.
Complaints and anamnesis 1. Pain - occurs suddenly, at the onset of the disease in the epigastric region or throughout the abdomen, is dynamically localized in the right iliac region, and is often permanent.
2. Nausea - in the first hours of the disease.
3. Vomiting - often one-time in the first hours of the disease.
4. Dry mouth.
5. Temperature reaction - usually 37.5-37.8°C.
6. Leukocytosis - with a shift in the leukocyte formula to the left, in the presence of complications, the ESR increases.
7. Forced position of the body - often on the right side with the legs brought to the stomach.
Physical examination When examining the abdominal cavity, a number of basic, characteristic symptoms are determined:
1. On palpation in the right iliac region, pain and tension in the muscles of the anterior abdominal wall are noted.
2. Shchetkin-Blumberg symptom - increased pain when the hand is sharply withdrawn after preliminary pressure.
3. Sitkovsky's symptom - increased pain in the right iliac region when the patient is positioned on the left side.
4. Rovsing's symptom - increased pain in the right iliac region upon palpation in the left iliac region with the movement of gases through the colon.
5. Voskresensky's symptom - the appearance of pain in the right iliac region when quickly running the palm along the anterior abdominal wall from the costal edge downwards.
The manifestation of local symptoms depends on the location of the appendix, but the general reaction of the body remains typical:
1. With a retrocecal location of the appendix, pain in the right iliac region, muscle tension, and symptoms of peritoneal irritation may be absent. There is pain in the right lumbar region, in the area of the lumbar triangle (Yaure-Rozanov symptom). With the transition of inflammation to the ureter or renal pelvis, a small amount of protein and single red blood cells may appear in the urine.
2. With a pelvic location - characterized by the absence of significant tension in the muscles of the anterior abdominal wall, pain on palpation is determined significantly lower than the typical location and is most clearly identified during rectal examination.
3. With a subhepatic location - pain on palpation is determined above the typical location, tension in the muscles of the anterior abdominal wall may be absent.
Laboratory research
1. CBC: leukocytosis, shift of the leukocyte formula to the left.
2. TAM: a small number of red blood cells and white blood cells.
Instrumental studies
Ultrasound: increase in the diameter of the appendix to 8-10 mm or more.
Survey fluoroscopy: fluid level in the cecum and terminal ileum, pneumatosis of the ileum and right half of the colon, deformation of the medial contour of the cecum.
Indications for specialist consultation: depending on concomitant pathology.
List of main diagnostic measures:
1. General blood test.
2. General urine analysis.
3. Blood type and Rh factor.
4. Microreaction.
List of additional diagnostic measures
Ultrasound of the abdominal cavity and small pelvis - in order to exclude damage to the abdominal organs, small pelvis, and retroperitoneal space.
Determination of blood sugar - for the purpose of differentiation from acute pancreatitis and diabetes mellitus.
Determination of blood diastasis - for the purpose of differentiation from acute pancreatitis.
Diagnostic laparoscopy - to establish a diagnosis.
Differential diagnosis
When collecting anamnesis, the history of the patient’s illnesses (existing or past) is important, since among them there may be those that mimic the clinical signs of acute appendicitis.
Typically, the diagnosis is made during a physical examination. The presence of the disease is indicated by a number of abdominal symptoms:
- in the position on the left side, the pain on the right is greatly intensified;
- the distance between the navel and the right anterior spine is less than on the left side (the reason is muscle contraction on the right);
- painful sensations in the iliac region on the right and upon percussion;
- when the abdomen is pulled in, the pain intensifies somewhat;
- body temperature in the right armpit is 1-2 degrees higher than in the left armpit.
Ultrasound is one of the important stages in diagnosing appendicitis. It allows you to detect the absence of peristalsis, the presence of free fluid, signs of peritonitis, blockage of the lumen and expansion of the appendix. If the information received is not enough, specialists resort to magnetic resonance imaging and abdominal radiography. Young children may require additional examination - electromyography of the anterior abdominal wall.
A general blood test in patients with this disease reveals nonspecific inflammatory changes.
In complex diagnostic cases, they resort to the method of diagnostic laparoscopy, which, if the diagnosis is confirmed, is transferred to therapeutic (appendectomy is performed during the diagnostic procedure). Determining the etiological factor that caused the pathology is possible by performing histology of the removed appendix.
Differential diagnosis is carried out with diseases such as acute cholecystitis, gastritis, cholelithiasis, gastric ulcer, pancreatitis, renal colic, acute cystitis, ectopic pregnancy, acute orchiepididymitis, neoplasms and other pathologies that can cause the development of an “acute abdomen”.
In rare cases, a rectal and/or vaginal examination is performed for differential diagnosis. The presence of a neoplasm of the cecum can be excluded or confirmed using the colonoscopy method.
Stages of the acute process
At the initial stage of development of acute appendicitis, the symptoms are blurred and uncharacteristic, or resemble signs of other diseases that a person tries to treat with conventional medications, including painkillers, which further distorts the overall clinical picture.
A dangerous feature of acute inflammation in the appendix is its rapid development. The count often goes not for days or days, but even for hours, during which the inflammatory process manages to develop from the usual acute version to purulent and phlegmonous.
In surgical practice, inflammation of the appendix is differentiated into 4 main stages, and the speed of transition from one to another can be dictated by a variety of factors:
- individual characteristics of the body;
- the presence of other chronic pathologies in it (diseases that are dealt with by gastroenterology: diagnosis has often already been carried out, and pain symptoms are attributed to an already identified pathology of the digestive system);
- weakened immune system;
- thrombosis of the vessels of the appendix resulting from prolonged compression;
- the body’s tendency to inflammatory purulent processes;
- lack of necessary care or use of inappropriate medications.
As a result of the interaction of unfavorable circumstances, the pathological process develops intensively and successively goes through several stages of intensification and aggravation, which in medical practice are called the stage of acute appendicitis.
Before and after the phlegmonous stage, appendicitis develops according to approximately one scenario, with slight differences in the time and intensity of each:
Catarrhal stage
Typically, it lasts no more than 16 hours, during which the symptoms of inflammation of the walls of the appendix are vague and, in the usual series of signs, appear in the right iliac region.
The catarrhal stage is accompanied by loss of appetite, pain that intensifies from time to time, sometimes diarrhea and vomiting, inevitable nausea and soreness in the umbilical region.
The inflammatory process is accompanied by signs reminiscent of common pathologies of the digestive tract or food poisoning, and in the absence of pain in the right half of the abdomen, which the average patient is oriented towards, they are accepted as such.
Lack of treatment leads to the appearance of a phlegmonous stage, which develops a day after the appendix becomes inflamed for any of the possible reasons.
The dynamics of the phlegmonous form is accompanied by increased dyspeptic disorders, increased body temperature, increased pain symptoms, initial changes in tissues and the spread of inflammation in the peritoneal space surrounding the appendix.
Acute phlegmonous appendicitis develops - a dangerous condition that is accompanied by the occurrence of a purulent process, as a result of which the medical history of a very patient patient can be supplemented, even with surgical intervention, by the development of acute peritonitis.
Gangrenous stage
Acute phlegmonous appendicitis, which is still without proper attention, goes from purulent inflammation to the process of necrotization of the tissue of the walls of the appendix, its complete death.
The appendix ruptures and the purulent contents spill into the abdominal organs.
The intensive development of septic processes begins, but some patients experience relief because the nerve endings that signal the body about the source of danger die off.
Phlegmonous appendicitis, the history of which has not received proper completion in the form of surgical removal, leads to a general condition called the gangrenous stage, which is easily fatal.
Perforated stage
It is not always distinguished as a separate one, because it is a short period during which acute phlegmonous appendicitis leads to perforation of the walls of the appendix and the entry of septic contents directly onto the abdominal organs.
In this case, a fatal outcome is no less likely than with gangrenous, characterized by complete destruction of the wall.
The organ of the abdominal cavity, which receives purulent contents, certainly begins to become inflamed, and this condition can lead to the most negative consequences.
Acute appendicitis :: Symptoms, causes, treatment and code according to ICD-10
Acute appendicitis in adults Acute appendicitis in children ... patients with acute appendicitis
Name: Acute appendicitis.
Acute appendicitis
Acute appendicitis.
An acute nonspecific process of inflammation of the appendix - an adnexal formation of the cecum.
The clinical picture of acute appendicitis manifests itself with the appearance of a dull pain in the epigastric region, which then shifts to the right iliac region; Nausea, vomiting, and low-grade fever are observed.
Diagnosis of acute appendicitis is based on identifying characteristic symptoms during examination of the abdomen, changes in peripheral blood, and ultrasound; this excludes other diseases of the abdominal cavity and pelvis. In acute appendicitis, an appendectomy is performed - removal of the altered appendix.
Acute appendicitis is the most common surgical disease, accounting for more than 80% in surgical gastroenterology.
Acute appendicitis most often occurs in people aged 20-40 years, although it can also occur in childhood or old age.
Despite advances in diagnostics and improvements in surgical treatment methods, postoperative complications in acute appendicitis are 5-9%, and mortality is 0.1-0.3%.
There is still no consensus on the reasons for the development of acute appendicitis. Among the etiological theories of acute appendicitis, mechanical, infectious, angioneurotic, allergic, immunological, etc. are discussed. It is believed that the leading factor in inflammation of the appendix (appendicitis) is a mechanical blockade of the lumen of the appendix caused by fecal stone, foreign body, parasites, hyperplasia of lymphoid tissue. This leads to the accumulation of mucus in the appendix, activation of the bacterial flora, inflammation of the walls of the appendix, and vascular thrombosis. According to the infectious theory, the development of acute appendicitis can be initiated by various infectious diseases - amoebiasis, parasitic infections, tuberculosis, yersiniosis, typhoid fever, etc. Proponents of the angioneurotic theory are of the opinion that trophic disorders in the wall of the appendix, associated with a violation of its innervation, are of primary importance. To a certain extent, a nutritional factor can contribute to the development of acute appendicitis. It is known that eating predominantly meat foods contributes to disruption of intestinal motor-evacuation function and a tendency to constipation, which, in turn, predisposes to the development of acute appendicitis. Also, unfavorable background factors include intestinal dysbiosis, decreased body resistance, and some types of location of the appendix in relation to the cecum.
Acute appendicitis is caused by nonspecific microbial flora: anaerobic non-spore-forming microorganisms (bacteroides and anaerobic cocci - in 90% of cases), aerobic pathogens (Escherichia coli, enterococci, Klebsiella, etc. - 6-8%), less often - viruses, protozoa present in the appendix. The main mechanism of infection of the appendix is enterogenous; lymphogenous and hematogenous routes of infection do not play a leading role in the pathogenesis of acute appendicitis.
Acute appendicitis can occur in a simple (catarrhal) or destructive form (phlegmonous, apostematous, phlegmonous-ulcerative, gangrenous). The catarrhal form of acute appendicitis (catarrhal appendicitis) is characterized by disorders of lymph and blood circulation in the wall of the appendix, its swelling, and the development of cone-shaped foci of exudative inflammation (primary affects). Macroscopically, the appendix looks swollen and congested, the serous membrane is dull. Catarrhal changes may be reversible. Otherwise, as they progress, simple acute appendicitis becomes destructive. By the end of the first day from the onset of acute catarrhal inflammation, leukocyte infiltration spreads to all layers of the appendix wall, which corresponds to the phlegmonous stage of acute appendicitis.
The walls of the appendix thicken, pus forms in its lumen, the mesentery becomes swollen and hyperemic, and a serous-fibrinous or serous-purulent effusion appears in the abdominal cavity. Diffuse purulent inflammation of the appendix with multiple microabscesses is regarded as apostematous acute appendicitis.
With ulceration of the walls of the appendix, phlegmonous-ulcerative appendicitis develops, which, with an increase in purulent-destructive changes, turns into gangrenous.
The development of acute appendicitis is divided into an early stage (up to 12 hours), a stage of destructive changes (from 12 hours to 2 days) and a stage of complications (from 48 hours). Clinical manifestations of acute appendicitis manifest suddenly, without any precursors or prodromal signs. In some cases, several hours before the development of acute appendicitis, nonspecific phenomena may be observed - weakness, deterioration in health, loss of appetite. For the stage of advanced clinical manifestations of acute appendicitis, pain and dyspeptic disorders (nausea, vomiting, gas and stool retention) are typical. Abdominal pain in acute appendicitis is the earliest and most persistent symptom. In the initial stage, the pain is localized in the epigastrium or peri-umbilical region, and is mild and dull in nature. When coughing or sudden changes in body position, the pain intensifies. A few hours after its onset, the pain shifts to the right iliac region and can be characterized by patients as tugging, stabbing, burning, cutting, sharp, dull. Depending on the location of the appendix, pain can radiate to the navel, lower back, groin, and epigastric region. In acute appendicitis, as a rule, there are symptoms of digestive disorders: nausea, single vomiting, flatulence, constipation, and sometimes loose stools. Body temperature usually rises to low-grade levels. In the stage of destructive changes, the pain syndrome intensifies, which significantly affects the condition of the patients. Body temperature increases to 38.5-390C, intoxication increases, tachycardia is noted up to 130-140 beats. In min. In some cases, a paradoxical reaction may be observed when pain, on the contrary, decreases or disappears. This is a rather ominous sign, indicating gangrene of the appendix.
High body temperature. Constipation. Flatulence. Neutrophilia. Lack of appetite. Vomit. Nausea.
In the diagnostic process, acute appendicitis must be differentiated from gastritis, gastric or duodenal ulcer, acute cholecystitis, pancreatitis, urolithiasis, cholelithiasis, ectopic pregnancy, adnexitis, acute orchiepididymitis, acute cystitis, and other diseases that occur with abdominal pain. Acute appendicitis is characterized by a number of abdominal symptoms: lag of the right abdomen during breathing (Ivanov's symptom), muscle tension of the anterior abdominal wall, symptom of peritoneal irritation (Shchetkin-Blumberg), pain in the right iliac region during percussion (Razdolsky's symptom), increased pain in position on the left side (Sitkovsky, Bartomier-Mikhelson symptom), etc. Changes in the leukocyte blood count increase in accordance with the stages of acute appendicitis - from 10-12x109/l with catarrhal inflammation to 14-18x109/l and higher - with purulent-destructive forms.
For the purpose of differential diagnosis, a rectal or vaginal examination is performed. To exclude other acute pathologies of the abdomen, an ultrasound of the abdominal organs is performed, which also detects an enlargement and thickening of the appendix, and the presence of effusion in the abdominal cavity. If the clinical and laboratory picture is unclear, diagnostic laparoscopy is resorted to.
In acute appendicitis, the earliest possible removal of the inflamed appendix is indicated - appendectomy. In typical cases of acute appendicitis, the Volkovich-Dyakonov approach to the appendix is used - an oblique incision in the right iliac fossa. In diagnostically unclear situations, the pararectal Lenander approach is used, in which the surgical incision runs parallel to the outer edge of the right rectus muscle above and below the navel. Mid-middle or lower-middle laparotomy is resorted to in cases where the course of acute appendicitis is complicated by peritonitis.
In recent years, with the development of minimally invasive surgery, the operation is often performed through a laparoscopic approach (laparoscopic appendectomy).
Timely seeking medical help and early surgical intervention are the key to a favorable outcome of acute appendicitis. Return to normal physical and work activities is usually allowed 3 weeks after appendectomy.
In case of development of complications of acute appendicitis (appendicular infiltrate, local abscesses in the abdominal cavity - pelvic, interintestinal, subphrenic, diffuse peritonitis, pylephlebitis, adhesive intestinal obstruction, etc.), the prognosis is serious.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: https://kiberis.ru/?p=33757
Acute appendicitis in children
from mucus and fecal sources of infection are considered inflamed. Suspicion of acute appendicitis requires
The appendix in the abdominal cavity represents the greatest complexity of the non-appendix.
acute pathology of the abdominal organs among patients with pain
Symptoms of acute appendicitis in a child
one or more of the listed Acute phlegmonous appendicitis (code by and takes several hours, Modern diagnostic methods include: may cost the patient his life. masses, foreign tonsils are less common. involvement in monitoring In preschool and school children
only for clinicians, butUltrasound criteria for chronic appendicitis considercavities cannot be identified.abdominal syndrome.filled with a variety of nutritious dishes.It is possible to restore the patient’s health only
body temperature rises to 39°; minutes the patient feels worsening factors. However, this is not ICD-10 K35.8) - it depends on the complexity. Questioning the patient, finding out the time of onset. Characteristic symptoms of acute appendicitis: objects. Mechanical damage to the appendix leads to a pediatric surgeon. Treatment of age, pain more often occurs for morphologists due to the following: In most patients, the pain is localized. What causes chronic appendicitis, how can a person use this with the help of surgical intervention, the heart rate increases up to 100 beats of the general condition, vomiting develops ,
- affects the rate of formation of a serious inflammatory disease, which
- The postoperative period is characterized by a possible attack, its intensity and digestive disorders: vomiting, diarrhea or
- Such changes may have a reversible formation of a focus of inflammation inward
- Acute appendicitis in children in the epigastrium or near the absence of convincing macroscopic and
What tests are needed?
Complications if appendicitis has already
The appearance of accompanying symptoms.
Constipation
form, otherwise
organ. As external
surgical
Treatment of acute appendicitis in a child
navel and only through microscopic data. visualized in the form of structures less often - in the lower Leading role in the occurrence of
Appendicitis
| Don't play with appendicitis! Don't take laxatives. Call a doctor |
Appendicitis
(eng.
appendicitis
or
epityphlitis
) is an inflammation of the appendix, a vermiform appendix on the human cecum. The most common disease requiring surgical intervention.
Classification of appendicitis according to ICD-10
The International Classification of Diseases ICD-10 classifies appendicitis as Class XI.
Diseases of the digestive system. Variants of the course of the disease are assigned the following ICD-10 codes: K35 Acute appendicitis
:
K35.2 Acute appendicitis with diffuse peritonitis
(acute appendicitis with diffuse peritonitis due to rupture or perforation)
K35.3 Acute appendicitis with local peritonitis
(acute appendicitis (with or without rupture or perforation) with peritonitis; acute appendicitis with peritoneal abscess)
K35.8 Acute appendicitis, other or unspecified
(acute appendicitis without specifying the type of peritonitis: local or diffuse)
K36 Other forms of appendicitis
(including chronic and recurrent)
K37 Appendicitis, unspecified
Separately, in “Class I. Some infectious and parasitic diseases”, among other infectious diseases caused by the amoeba Entamoeba histolytica, listed under ICD-10 code A06.8, amoebic appendicitis
.
Manifestation
Most often, pain with appendicitis initially occurs in the upper abdomen (the article “Pain in the abdomen” gives typical manifestations of pain in various diseases), then the pain gradually intensifies and shifts to the right lower abdomen.
Sometimes my whole stomach hurts. There are atypical manifestations of appendicitis. With appendicitis, there is no appetite, the mouth may be dry, the patient feels general weakness, and the temperature often rises to 37-38 C°. The pain intensifies when walking and lying on the left side. Appendicitis can be accompanied by both diarrhea and constipation. In the latter case, taking any laxatives is not recommended.
In children, appendicitis occurs against the background of vascular spasm or thrombosis, infection in combination with impaired reactivity of the body. The child complains of sharp pain in the lower abdomen, more on the right, which then moves up to the navel area, after which it moves to the right iliac region. Vomiting, nausea, and possibly diarrhea are observed (with the pelvic location of the appendix). Body temperature rises to 38–39°C. When palpating the abdomen, defence and pain are determined. During digital examination of the rectum, pain and overhang of its anterior wall are noted. There are symptoms of peritoneal irritation. In children, symptoms increase faster than in adults, and peritonitis develops more often, therefore, in unclear cases, one cannot limit oneself to observation; it is necessary to perform diagnostic laparoscopy (Chernekhovskaya N.E.).
Treatment of appendicitis
Currently, the main treatment method for appendicitis is surgical removal of the appendix - appendectomy. If you suspect appendicitis, you should immediately consult a doctor.
Is appendectomy necessary for inflammation of the appendix?
According to some scientists (Palminen S. et al. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis. The APPAC Randomized Clinical Trial. JAMA. 2015;313(23):2340-2348. doi:10.1001/jama.2015.6154) for For uncomplicated acute appendicitis, confirmed by computed tomography, surgery is not necessary.
Antibiotic therapy is sufficient: intravenous ertapenem (1 g/day) for 3 days and then oral levofloxacin (500 mg once a day) and metronidazole (500 mg 3 times a day) for 7 days. After this, 70% of patients do not require surgical intervention within a year. In those who required intervention, serious complications do not occur due to the delay in the operation. Also in the study: Minneci PC, Mahida JB, Lodwick, DL, Sulkowski JP, Nacion KM, Cooper JN, Ambeba, EJ, Moss RL, Deans KJ. The effectiveness of patient choice in non-operative versus surgical management of uncomplicated acute appendicitis. JAMA Surgery. 2015 Dec 16 found that uncomplicated acute appendicitis in children aged 7 to 17 years can in most cases be cured with medication.
If perforation of appendicitis, infection in the abdominal cavity, the presence of stones in appendicitis and other complications are suspected, surgical intervention is necessary.
Antibiotic therapy for appendicitis is an object of scientific research and has not yet been introduced into clinical practice.
Differential diagnosis of acute appendicitis using electrogastroenterography
In acute appendicitis, electrophysiological indicators of gastrointestinal motility measured by peripheral electrogastroenterography are characterized by a statistically significant decrease in relative electrical activity and an increase in the rhythmicity coefficient of the colon, in comparison with the group of patients without intraoperative verification of the diagnosis of acute appendicitis. In the edematous form of acute pancreatitis, the electrophysiological characteristic is a decrease in all indicators in the areas of the duodenum, jejunum and ileum (Zaitsev A.V. et al.).
Publications addressing surgical treatment of appendicitis intended for healthcare professionals
- Sazhin A.V., Nechai T.V., Tyagunov A.E., Melnikov-Makarchuk K.Yu., Tyagunov A.A. Fast-track in urgent surgical pathology: present and future. Randomized study of the use of the fast-track algorithm in the treatment of acute appendicitis. // II Conf. MNHO "FAST TRUCK". Moscow. April 27, 2021. pp. 55–57.
- Zaitsev A.V., Smolkina A.V., Zaitseva O.B., Rogova Yu.Yu., Gerasimov N.A., Barinov D.V. The role of Gastroscan-GEM in acute appendicitis // International Journal of Applied and Fundamental Research. 2013. No. 8. P. 104.
- Midlenko V.I., Zaitsev A.V., Smolkina A.V., Zaitseva O.B. Electrogastroenterography in urgent surgery // Materials of the Russian scientific and practical conference with international participation. – 2010. – Ulyanovsk. – P. 114.
- Basnaev U.I., Mikhailichenko V.Yu., Karakursakov N.E., Kislyakov V.V., Basnaeva A.D. On the issue of enteral nutrition in patients with appendiceal peritonitis. Tauride Medical and Biological Bulletin. 2021, vol. 22, no. 1, pp. 7-13.
On the website gastroscan.ru in the literature catalog there is a section “Surgery”, containing medical articles for professionals concerning surgery of the abdominal cavity and digestive tract.
Appendectomy reduces the risk of developing Parkinson's disease (?)
There is a study* that claims that removing the appendix reduces the likelihood of developing Parkinson's disease by 19.3%.
It was also found that appendectomy slowed the onset of Parkinson's disease by an average of 3.6 years. This, according to the authors of the work, is due to the fact that the protein alpha-synuclein accumulates in the appendix, which provokes the development of Parkinson’s disease. From the appendix, the pathogenic form of alpha-synuclein can penetrate the gastrointestinal tract and then into the brain. *Killinger BA, et al. The vermiform appendix impacts the risk of developing Parkinson's disease. Science Translational Medicine 31 Oct 2021: Vol. 10, Issue 465, eaar5280. DOI: 10.1126/scitranslmed.aar5280 Back to section
Diet after surgery for phlegmonous appendicitis
For two to four weeks after surgery and discharge from the hospital, to prevent constipation, you need to follow a diet. You can only eat foods grown by a doctor.
For the first two days, you need to eat exclusively liquid porridge and vegetable puree. It is also worth adding jelly or low-fat kefir to your diet. Next, gradually introduce black bread with a small amount of butter. The transition to regular food that is familiar to the patient can only be done if the patient feels excellent and has normal stools. But do not forget that food should not be spicy, pickled, smoked, fatty, fried or hard. Also in the diet you should exclude coffee and strong tea, soda, and pastries made from butter dough. All food is prepared by baking or boiling.
You need to eat in small portions, about five to six times a day.
Diagnosis of appendicitis
The diagnosis of appendicitis can be made by symptoms that add up to the picture of the disease. If doctors have doubts, then the reason for hospitalization is indicated as acute unspecified appendicitis according to ICD 10, which means:
In such cases, the patient is left in the hospital for a day or three to observe the development of the picture. at the same time, they can have different intensities, the temperature remains within 38 C, the patient will consider his condition almost satisfactory.
To clarify the diagnosis, a doctor is prescribed, an anamnesis is collected, and in some cases an ultrasound of the abdominal cavity is performed. Practice shows that in 90% of cases the diagnosis is confirmed, since the next stage of the disease occurs quite quickly. The most reasonable decision for the patient remains to stay in the clinic, since if the condition worsens, the operation will be performed immediately and the risk will be minimal.
Treatment of acute appendicitis
Acute gangrenous appendicitis is treated surgically. For pain relief, local anesthesia or general anesthesia is used. In advanced cases with the development of peritonitis, doctors use endotrichial anesthesia with ventilation.
Appendectomy involves two types of surgical intervention: traditional and laparoscopic.
Traditional appendectomy
The preparatory stage for the operation lasts no more than two hours. It includes the collection of blood and urine tests, as well as a number of diagnostic procedures:
- Ultrasound.
- CT scan.
- Rectoscopy.
- Visit to the radiologist.
- For women – consultation with a gynecologist.
- ECG for heart problems.
After the tests are collected, the patient is prepared for surgery. Held:
- Bladder catheterization.
- Shaving the abdominal wall.
- Disinfecting the skin with an antiseptic.
Surgery to remove appendicitis
The operation is performed through an incision in the iliac zone on the right. The cecum is pulled out and the appendix is excised. After this, doctors suture or drain the wound. Inflammatory fluid is removed from the peritoneal cavity using an electric suction device and wipes.
In some cases, surgeons leave drainage - gauze swabs - in the abdominal cavity. This happens if:
- The appendicitis was not completely excised.
- Despite all measures, bleeding continues from the excision site.
- An abscess has opened and the pus needs to be drained.
- An infiltrate has been detected and removal of the appendage is impossible.
Laparoscopy
A progressive method of surgical intervention, which is performed with a laparoscope and special surgical instruments. A laparoscope is a flexible tube with a video camera and lighting. With its help, the surgeon looks into the most remote places of the peritoneum and examines the organs from all sides. If necessary, organs are examined using a laparoscope before surgery.
Removing appendicitis using a laparoscope
Advantages of laparoscopy compared to traditional resection of appendicitis:
- Less tissue is injured.
- Wounds heal faster after surgery.
- The recovery period is halved.
- Minimal risk of complications.
- Scars after laparoscopy are almost invisible.
The disadvantages of laparoscopy are high cost and individual contraindications to surgery. In rare cases, due to equipment malfunction, unforeseen consequences occur: intestinal burns and damage to adjacent organs.
Treatment
The only treatment option is surgery to remove appendicitis, which in medical terminology is called an appendectomy. It is done using the classic surgical method through one incision or through three small incisions (length does not exceed 1 cm) using laparoscopy. The decision about which method of surgery is most suitable depends solely on the form of appendicitis.
Preparing for surgery
Often surgery to remove the appendix is performed as an emergency. Emergency care can follow within 1-2 hours after the patient’s admission to the surgical department of the hospital. In some cases there is no time for special preparation. An appendectomy can last from 40-50 minutes to several hours. The duration of the operation directly depends on whether there are complications.
If time before the intervention allows, patient preparation includes:
- examination of the cardiovascular system (ECG);
- cleansing the stomach (most often the patient does not drink or eat anything, so this is done extremely rarely);
- hair removal in the area of manipulation;
- the patient is administered an isotonic solution intravenously to eliminate symptoms of intoxication, as well as to prevent dehydration;
- determining which anesthesia is suitable for the patient (checking for lack of reaction to painkillers);
- skin disinfection.
For uncomplicated disease, laparoscopic appendectomy is most often used. A laparoscope is inserted through an opening in the abdominal wall, which provides access to the appendix. The space in the abdominal cavity is filled with a special gas (pneumoperitoneum), after which the appendix is removed under visual control (the laparoscope is equipped with a micro-camera and a cold light source).
The camera transmits an image of the surgical field to a monitor installed in the operating room. This method is the most modern and allows you to avoid unnecessary blood loss and trauma. Also, the advantages of this method include a shorter postoperative period and the absence of a large postoperative scar.
In case of complications of acute appendicitis, for example, diffuse peritonitis, laparotomy with a thorough examination of the abdominal organs is indicated.