Nutrition is a process necessary to ensure the vital functions of the human body. The stomach plays one of the main roles in this process. The functions of the stomach include the accumulation of food mass, its partial processing and further movement into the intestines, where the absorption of nutrients occurs. All these processes occur in the gastrointestinal tract.
Stomach: structure and functions
It is a muscular hollow organ of the digestive system, which is located between the esophagus and the duodenum.
Next, we will find out what function the stomach performs and analyze its structure.
It consists of the following conventional sections:
- Cardial (entrance) part. Its projection is located at the level of the 7th rib on the left.
- The arch or bottom, the projection of which is located on the left at the level of the 5th rib, more precisely, its cartilage.
- Body of the stomach.
- Pyloric or pyloric region. At the exit from the stomach is the pyloric sphincter, which separates the stomach from the duodenum. The projection of the pylorus is located anteriorly opposite the 8th rib to the right of the midline and posteriorly between the 12th thoracic and 1st lumbar vertebrae.
The shape of this organ resembles a hook. This is especially noticeable on x-rays. The stomach has a lesser curvature, which faces the liver, and a greater one, facing the spleen.
The wall of the organ consists of four layers, one of which is outer, it is the serous membrane. The other three layers are internal:
- Muscular.
- Submucosal.
- Slimy.
Due to the hard muscular layer and the submucosal layer lying on it, the mucosa has numerous folds. In the area of the body and fundus of the stomach, these folds have an oblique, longitudinal and transverse direction, and in the area of the lesser curvature - only longitudinal. Due to this structure, the surface of the gastric mucosa increases significantly. This makes the bolus of food easier to digest.
Structure of the stomach
The stomach is located in the upper abdomen, and is slightly displaced to the left hypochondrium. In the medical literature, the upper part of the abdomen, located under the lower edge of the sternum and ribs, is called the epigastric region, or epigastrium .
The shape of the stomach is not constant and depends on its filling, body position, the condition of surrounding organs and the constitution of the person.
The stomach is a hollow muscular organ, the maximum volume of which is individual for each person and is 1.5-2.5 liters.
The stomach has two sphincters (ring muscles) that regulate the entry of food from the esophagus and its exit after processing into the duodenum. These are the esophageal and pyloric sphincter (or pylorus).
The stomach is conventionally divided into 4 sections: Cardiac section, fundus or fornix, body and pyloric section.
Structure of the stomach:
Motor function
Further digestion of food occurs in the stomach. The motor function of the stomach is the accumulation of food mass, its mechanical processing and further movement into the intestine.
During meals and in the first minutes after this, the stomach is relaxed, which promotes the accumulation of food in it and ensures the release of secretions. Next, contractile movements begin, which are provided by the muscle layer. In this case, the food mass is mixed with gastric juice.
The muscles of the organ are characterized by the following types of movements:
- Peristaltic (wavy).
- Systolic - occur in the pyloric region.
- Tonic - help reduce the size of the stomach cavity (its bottom and body).
After eating, peristaltic waves are weak at first. By the end of the first hour after a meal, they intensify, which promotes the movement of the food bolus towards the exit from the stomach. The pressure in the pyloric region of the stomach increases. The pyloric sphincter opens and part of the food mass enters the duodenum. The remaining majority of this mass is returned to the pyloric region. The evacuation function of the stomach is inseparable from the motor function. They ensure grinding and homogenization of the food mass and thereby contribute to better absorption of nutrients in the intestines.
Types of gastric glands
Pyloric
The structure of the gastric glands.
These centers are located at the junction of the stomach and the small intestine. The structure of glandular cells is branched with a large number of terminal tubules and wide lumens. The pyloric glands have endocrine and mucous secretors. Both components play a specific role: the endocrine centers do not secrete gastric juice, but control the functioning of the gastrointestinal tract and other organs, and the accessory centers form mucus, which dilutes the digestive juice in order to partially neutralize the acid.
Cardiac
They are located at the entrance to the organ. Their structure is formed from endocrine tubes with epithelial ones. The task of the cardiac glands is the secretion of mucoid mucus with chlorides and bicarbonates, which is necessary to ensure the sliding of the food bolus. These mucous accessory secretors are also located at the bottom of the esophagus. They soften food as much as possible in preparation for digestion.
Own
They are numerous and cover the entire body of the stomach, lining the bottom of the stomach. Fundic bodies are also called the own glands of the stomach. The tasks of these structures include the production of all components of gastric juice, in particular pepsin, the main digestive enzyme. The fundic structure includes mucous, parietal, main, and endocrine components.
With prolonged chronic inflammation, the stomach's own glands degenerate into cancerous ones.
Secretory function. Stomach glands
The secretory function of the stomach is to chemically process the bolus of food using the secretion produced. An adult produces from one to one and a half liters of gastric juice per day. It contains hydrochloric acid and a number of enzymes: pepsin, lipase and chymosin.
Glands are located on the entire surface of the mucosa. They are exocrine glands that produce gastric juice. The functions of the stomach are directly related to this secretion. Glands are divided into several types:
- Cardiac. They are located in the cardia area near the entrance to this organ. These glands produce a mucoid mucus-like secretion. It performs a protective function and serves to protect the stomach from self-digestion.
- Main or fundic glands. They are located in the area of the fundus and body of the stomach. They produce gastric juice containing pepsin. Due to the juice produced, the food mass is digested.
- Intermediate glands. Located in the narrow intermediate zone of the stomach between the body and the pylorus. These glands produce a viscous mucoid secretion, which has an alkaline reaction and protects the stomach from the aggressive effects of gastric juice. It also contains hydrochloric acid.
- Pyloric glands. Located in the gateway area. The secretion they produce also plays a protective role against the acidic environment of gastric juice.
The secretory function of the stomach is provided by three types of cells: cardiac, fundic, or main, and pyloric.
The mechanism of digestion in the stomach.
The digestive functions of the stomach are deposition, mechanical and chemical processing of food and gradual portioned evacuation of stomach contents into the intestine . Food, being in the stomach for several hours, swells, liquefies, many of its components dissolve and undergo hydrolysis by enzymes of saliva and gastric juice.
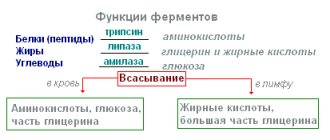
Salivary carbohydrases act on food carbohydrates located in the central part of the food contents of the stomach, where gastric juice , stopping the action of carbohydrases. Enzymes of gastric juice act on proteins in food contents in the area of direct contact with the gastric mucosa and at a short distance from it, where gastric juice has diffused.
Secretory function of the stomach.
Gastric juice (2-2.5 liters per day) contains many inorganic substances: water, chlorides, sulfates, phosphates, sodium bicarbonates, potassium, calcium, magnesium, ammonia . The osmotic pressure of gastric juice is higher than that of blood plasma.
The parietal cells produce hydrochloric acid of the same concentration (160 mmol/l), but the acidity of the secreted juice varies. The faster the secretion of hydrochloric acid, the less it is neutralized and the higher the acidity of gastric juice.
Hydrochloric acid of gastric juice causes denaturation and swelling of proteins and thereby promotes their subsequent breakdown by pepsins , activates pepsinogens, creates an acidic environment necessary for the breakdown of food proteins by pepsins; participates in the antibacterial effect of gastric juice and regulation of the activity of the digestive tract (depending on the pH of its contents, its activity is enhanced or inhibited by nervous mechanisms and gastrointestinal hormones).
The organic components of gastric juice are represented by nitrogen-containing substances: urea, uric and lactic acids, polypeptides . The protein content reaches 3 g/l, mucoproteins - up to 0.8 g/l, mucoproteases - up to 7 g/l. Organic substances of gastric juice are products of the secretory activity of the gastric glands and metabolism in the gastric mucosa , and are also transported through it from the blood.
Among proteins, enzymes . The main cells of the gastric glands synthesize several pepsinogens , which are usually divided into two groups. Pepsinogens of the first group are localized in the fundus of the stomach , the second group - in the antrum and the beginning of the duodenum . When pepsinogens are activated by the cleavage of a polypeptide from them, several pepsins are formed. Actually, pepsins are called enzymes of the protease class , which hydrolyze proteins at a maximum speed at pH 1.5-2.0. The protease, called gastricsin, has an optimal pH of 3.2-3.5 for protein hydrolysis. These enzymes have different effects on different types of proteins.
Pepsins are endopeptidases , and the main products of their hydrolytic action on proteins are polypeptides (about 10% of bonds are broken to release amino acids). The ability of pepsins to hydrolyze proteins in a wide pH range is of great importance for gastric proteolysis, which occurs at different pH levels depending on the volume and acidity of gastric juice, buffer properties and the amount of food taken, and the diffusion of acidic juice deep into the gastric contents. Protein hydrolysis occurs in close proximity to the mucous membrane. The passing peristaltic wave “removes” the mucosal layer, moves it to the antrum of the stomach, as a result of which the former deeper layer of food content, on the proteins of which pepsins acted in a slightly acidic reaction, adjoins the mucous membrane. These proteins undergo hydrolysis by pepsins in a more acidic environment.
An important component of gastric juice are mucoids, produced by mucocytes of the surface epithelium , neck of the fundic and pyloric glands. Gastromucoprotein (internal Castle factor) also belongs to mucoids . A layer of mucus 1-1.5 mm thick protects the gastric mucosa and is called the gastric mucosal protective barrier . Mucus - a mucoid secretion - is represented mainly by two types of substances - glycoproteins and proteoglycans.
The glands in the pyloric part of the stomach secrete a small amount of slightly alkaline juice with a high content of mucus. The alkaline pyloric secretion partially neutralizes the acidic contents of the stomach, evacuated into the duodenum.
is of great protective importance , the destruction of which can be one of the reasons for damage to the mucous membrane of the stomach and even deeper structures of its wall. This barrier is damaged by high concentrations of hydrochloric acid in the stomach contents, aliphatic acids (acetic, hydrochloric, butyric, propionic) even in small concentrations, detergents (bile acids, salicylic and sulfosalicylic acids in the acidic environment of the stomach), phospholipases, and alcohol. Prolonged contact of these substances (at their relatively high concentrations) disrupts the mucosal barrier and can lead to damage to the gastric mucosa.
The destruction of the mucous barrier and stimulation of the secretion of hydrochloric acid is facilitated by the activity of microorganisms Helicobacter pylori . In an acidic environment and in conditions of a damaged mucous barrier, it is possible to digest elements of the mucous membrane with pepsin (peptic ulcer-forming factor). This is also facilitated by a decrease in the secretion of bicarbonates and blood microcirculation in the gastric mucosa.
Excretory function
It lies in the fact that some substances enter the stomach cavity from the lymph and blood through its wall, namely:
- Amino acids.
- Squirrels.
- Uric acid.
- Urea.
- Electrolytes.
If the concentration of these substances in the blood increases, then their entry into the stomach increases.
The excretory function of the stomach is especially important during fasting. Protein in the blood cannot be used by the body's cells. They are only able to assimilate the final product of protein breakdown - amino acids. Getting from the blood into the stomach, the protein undergoes further processing there under the action of enzymes and breaks down into amino acids, which are subsequently utilized by the body’s tissues and its vital organs.
Protective function
This function is provided by the secretion produced by the organ. Invaded pathogenic microorganisms die from the action of gastric juice, or more precisely, from the hydrochloric acid contained in its composition.
In addition, the stomach is designed in such a way that if poor-quality food gets into it, it is able to ensure its return and prevent dangerous substances from entering the intestines. Thus, this process will prevent poisoning.
Endocrine function
This function is carried out by endocrine cells of the stomach, which are located in its mucous layer. These cells produce more than 10 hormones that can regulate the functioning of the stomach and digestive system itself, as well as the entire body as a whole. These hormones include:
- Gastrin is produced by G cells of the stomach itself. It regulates the acidity of gastric juice, being responsible for the synthesis of hydrochloric acid, and also affects motor function.
- Gastron - inhibits the production of hydrochloric acid.
- Somatostatin - inhibits the synthesis of insulin and glucagon.
- Bombesin - this hormone is synthesized both by the stomach itself and the proximal small intestine. Under its influence, the release of gastrin is activated. It also affects the contractions of the gallbladder and the enzymatic function of the pancreas.
- Bulbogastron - inhibits the secretory and motor function of the stomach itself.
- Duocrinin - stimulates the secretion of the duodenum.
- Vasoactive intestinal peptide (VIP). This hormone is synthesized in all parts of the gastrointestinal tract. It inhibits the synthesis of pepsin and hydrochloric acid and relaxes the smooth muscles of the gallbladder.
We found out that the stomach plays an important role in the process of digestion and ensuring the vital functions of the body. Its structure and functions were also indicated.
HCO3, which, entering the lumen of the duodenum, neutralizes H+. A decrease in H+ concentration inhibits the synthesis and release of secretin. The main site of action of secretin is the cells of the excretory ducts of the pancreas. If the pH of the duodenal contents becomes above 4.5, then stimulation of pancreatic secretion by secretin is not observed. In the stomach, secretin stimulates the secretion of pepsin and the function of the pyloric sphincter, inhibits gastrin secretion caused by acids, stops gastrin secretion under the influence of food and inhibits gastric motility. In the endocrine apparatus of the pancreas, it stimulates the secretion of insulin and inhibits the release of glucagon. In the liver, secretin activates bile production and gallbladder contraction caused by cholecystokinin. In the duodenal glands (Brunner's glands), it stimulates the secretion of water and bicarbonates. It inhibits small intestinal motility and the resorption of water and Na+. Secretin is excreted from the body mainly by the kidneys.
In clinical practice, determination of secretin in the blood is necessary for diagnosing Werner-Morrison syndrome. Its level can be significantly increased in patients suffering from duodenal ulcer. To carry out differential diagnosis between these diseases, a secretin test is sometimes used. Administration of secretin to a patient with Werner-Morrison syndrome causes an increase in the gastrin content in the blood, while the level of gastrin in the blood of healthy people and patients with peptic ulcer disease decreases.
Vasoactive intestinal polypeptide in plasma
Plasma levels of vasoactive intestinal polypeptide are normal
-
20
-
53 pg/ml.
Vasoactive intestinal polypeptide (VIP) belongs to the group of intestinal hormones. It consists of 28 amino acid residues and is chemically similar to glucagon. VIP is found in cells along the entire length of the small intestine. It is characterized by a pronounced vasodilator and hypotensive effect. In the digestive system, VIP inhibits HC1 secretion caused by gastrin or histamine; inhibits the secretion of pepsin and promotes relaxation of the stomach muscles. It also stimulates the secretion of water and electrolytes in the pancreas and the formation of bile. Its concentration in the cerebrospinal fluid is 10 times higher than in plasma. Determination of VIP content in plasma is important for the diagnosis of pancreatic cholera syndrome (Werner-Morrison syndrome; WDHA syndrome: watery diarrhea, hypoglycemia, achlorhydria). Werner-Morrison syndrome is characterized by life-threatening diarrhea of up to 10 liters per day, with all associated electrolyte disturbances. The development of this clinical picture is due to hypersecretion of VIP and histidine-isoleucine peptide by gastroenteropancreatic endocrine tumors or ganglioneuroblastoma. Most often, Werner-Morrison syndrome is caused by tumors localized in the pancreas and producing large amounts of VIP (tens of times higher than normal). About 25% of such tumors are located outside the pancreas and have the morphological features of ganglioneuroblastoma [Gitel E.P., Fadeev V.V., 1996]. An increase in plasma VIP levels can be detected in Crohn's disease, but the degree of increase is much lower (VIP increases approximately 2 times).
Serum serotonin
The normal serum serotonin content in adults is 0.22-2.05 µmol/l (40-80 µg/l).
Serotonin (oxytryptamine) is a biogenic amine found mainly in platelets. Up to 10 mg of serotonin constantly circulates in the body. From 80 to 95 %
its total amount in the body is synthesized and stored in the enterochromaffin cells of the gastrointestinal tract. Serotonin is formed from tryptophan as a result of decarboxylation. In the enterochromaffin cells of the gastrointestinal tract, most of the serotonin is adsorbed by platelets and enters the bloodstream. This amine is localized in large quantities in a number of parts of the brain, there is a lot of it in mast cells of the skin, and it is found in many internal organs, including various endocrine glands. Serotonin, formed by the listed sources, affects the endocrine systems in various ways:
474
Functional disorders
Gastrointestinal diseases are usually associated with a violation of any of its structures. Stomach dysfunction is observed quite often. We can talk about such pathologies only if the patient’s examination does not reveal any organic lesions of this organ.
Disorders of the secretory or motor function of the stomach can occur with pain and dyspepsia. But with proper treatment, these changes are often reversible.