Benign pancreatic tumor is a rare disease. Doctors from different countries have described only about 200 cases. The prevalence is 1–3 cases per 1 million population. According to statistics from pathologists, the disease occurs once in 3500–5000 autopsies.
The tumor is usually detected incidentally during examination for other suspected diagnoses. The tumor makes itself felt only if it grows with stretching of the pancreatic capsule or compression of surrounding organs.
The pathology was assigned a statistical code according to ICD-10 D13.6. A separate code is D13.7 for benign islet cell tumors.
What is the difference between a benign tumor and a malignant one?
A number of histological and clinical signs indicate the benign nature of the process in the pancreatic gland. Differences from cancer are included in the table.
| Feature name | Benign tumor | Malignant tumor |
| The result of a cytological examination of the material obtained during biopsy | Consists of cells “native” to the gland. | The cell type is changed, similar to other tissues. |
| History of the disease | Eliminates precancerous pathology and heredity. | It turns out that the patient has chronic diseases of the stomach, intestines, viral hepatitis, cirrhosis of the liver, chronic pancreatitis, and similar cases are possible in the family. |
| Manifestations | There are often no symptoms. | The growth of the formation is manifested by severe pain, indigestion, and dyspepsia. |
| Signs of intoxication | None. | Patients have: weakness, nausea, vomiting, loss of appetite, weight loss, pale skin, fever. |
| Tumor marker level | Normal. | Protein complexes CA 19-9, CEA are increased. |
| Growth dynamics | Absent or insignificant. | There is a rapid increase. |
| Blood supply | Does not have an abundant network of arteries. | Growth requires increased nutrition, so additional vessels grow. |
| Tendency to metastasize | Absent. | It quickly spreads to neighboring tissues, the nearest lymph nodes, and gives distant metastases to the lungs, liver and other organs. |
Why does pancreatic tumor occur?
Scientists cannot say exactly why the disease occurs, but a number of main indirect reasons are called:
- Smoking. More than half of the patients suffering from the tumor are smokers with many years of experience. Substances in tobacco smoke provoke the occurrence of malignant neoplasms. The situation is aggravated by the fact that regular smoking of cigarettes disrupts the proper blood supply to the organ.
- Chronic pancreatitis. A constant, low-grade inflammatory process promotes the modification of healthy cells into cancerous tumors.
- Diabetes. In people suffering from diabetes for many years, glucose levels are constantly higher than normal, which greatly increases the likelihood of cancer.
- Hereditary predisposition. If one of the family members suffered from a similar disease, immediate relatives need to closely monitor their health and undergo a timely examination.
- Excess body weight. Excess fats and carbohydrates create excessive stress on the organ and provoke the formation of additional fat cells in the tissues, which are prone to transform into malignant tumors.
- Poor nutrition. There is a hypothesis that if the basis of the diet consists of fatty meat dishes, then the risk of tumors in the pancreas increases. Alcohol, caffeine, and lack of fresh vegetables and fruits have a negative impact.
- Chronic diseases of the liver and gastrointestinal tract. Gastric ulcers are especially dangerous in this regard: the intestines cannot fully neutralize all the toxic substances accumulated in the body.
- Infectious diseases.
- Poisoning with toxic substances.
- Lack of adequate physical activity.
- Advanced age of the patient.
- Living in unfavorable environmental conditions, especially in areas with high background radiation.
Causes of benign neoplasms
Specific causes of the pathology have not been identified. Scientists have identified risk factors. When examining people with a predisposition, the risk of developing a neoplasm is much higher. The group includes:
- patients who smoke and abuse alcohol,
- persons suffering from chronic pancreatitis, long-term inflammatory process in the gastroduodenal zone,
- people living in areas contaminated with toxic emissions, radiation,
- members of families where there were cases of tumor pathology of various organs.
Malnutrition is considered a risk factor:
- alternating periods of hunger and overeating,
- lack of a regular eating schedule,
- passion for fatty meat dishes, fast food,
- neglect of vegetables and fruits (leads to a lack of plant proteins, fiber, vitamins).
Causes of lymphoma in the pancreas
There is no answer to the question of why the lymphatic vessels adjacent to the secretory-digestive organ are affected by this type of oncology. But, despite the fact that the causes of pancreatic lymphoma have not been established, experts, based on the results of numerous studies, have identified a number of factors that can increase the risk of developing this disease.
Most often, pancreatic lymphoma occurs under the influence of the following pathological factors:
- Long-term poisoning of the body with alcohol, nicotine and carcinogens from low-quality products or those containing flavorings, preservatives and dyes.
- Immunodeficiency conditions in which the human immune system destroys the cells of its body, mistaking them for strangers for some unknown reason (HIV infection).
- Exposure to the bacterium Helicobacter pylori, which provokes the development of most dangerous pathologies in the digestive tract.
- The Epstein-Barr virus (a prototype of the herpes virus), which remains in a latent form in the human body for a long time, causing irreparable harm to the immune system at this time.
Heredity plays an important role in the development of cancer pathology that affects the walls of lymphatic vessels. Most often, this type of disease occurs in people whose blood relatives suffered from autoimmune conditions or immunodeficiency. If we talk about the risk group, then the majority of patients with this diagnosis are elderly people. But gender is a controversial issue. Data on this feature vary. Some sources include men as the main risk group, while others give predominance to women. Age category. Most often, older people develop this disease. The main group of patients with this diagnosis turned 60 years old.
Classification
Benign pancreatic tumors differ in their histological structure and origin from a specific type of tissue. There is no typical localization for them, but the diagnosis reflects the location in the body, the head part of the organ or the tail. In case of multiple foci, they are considered combined.
The starting cells can be:
- epithelial covering of excretory ducts,
- fat deposits (lipomas),
- nerve or muscle cells (neurinoma, ganglioma, leiomyoma),
- fibrocytes (fibromas),
- vessels (hemangiomas, lymphangiomas),
- glandular and hormone-producing (insuloma, adenoma).
List of pancreatic tumor symptoms
Clinical manifestations depend on the type of tumor. Formations that do not produce hormones are easily tolerated, are not detected for a long time and do not give symptoms until they increase in size.
Manifestations of a large tumor are associated with a compressed organ or vessel. The patient experiences constant aching pain that intensifies with movement.
An enlarged head of the pancreas gives pain in the right hypochondrium and epigastrium. If the neoplasm lies in the body, pain appears in the upper half of the abdomen, the caudal localization is characterized by irradiation to the lumbar area on the left.
When the common bile or pancreatic duct is compressed, jaundice of the skin and sclera, itching, darkening of urine and light gray feces appear (signs of obstructive jaundice). Reducing the intestinal lumen contributes to intestinal obstruction with severe pain, impaired passage of gases and stool, and vomiting.
Attention: if the growing formations affect the cells of the pancreas that produce hormones, then the patient will experience endocrine disorders.
Insulinomas produce extra insulin and therefore cause a drop in blood glucose levels. Signs of hypoglycemia are observed (dizziness, weakness, sweating, palpitations, irritability). Lack of treatment leads to coma.
Gastrinoma is a tumor of cells that synthesize the digestive hormone gastrin. Patients have been treated for a long time without success for ulcers of the stomach, duodenum and jejunum. Intense pain in the epigastric region, heartburn, belching, acid vomiting, and intestinal dysfunction are typical.
Glucagonoma - stimulates an increase in glucose levels in the blood and urine. It manifests itself as weight loss, a brownish-red rash on the thighs, buttocks, dry and flaky skin, inflammation of the gums, stomatitis, and in women - vaginitis.
It is important that diabetes mellitus developing with glucagonoma does not require antihyperglycemic drugs in therapy and is compensated by diet. Rarely gives complications.
Hemangioma and lymphangioma with significant sizes turn into a cyst, cystadenoma or solid (malignant) tumors.
Symptoms of pancreatic head cancer
In the early stages, the tumor usually does not manifest itself. Then some symptoms appear, but they are non-specific, most often they indicate some other disease.
The most characteristic manifestation of pancreatic head cancer is jaundice. It is often the first symptom with which a patient consults a doctor. Next to the head of the gland is the bile duct. As the tumor grows, it compresses it, disrupting the flow of bile. As a result, the toxic breakdown product of hemoglobin - bilirubin - is not excreted into the intestines, but enters the blood. This leads to the skin and whites of the eyes becoming yellowish and causing itching.
Since bilirubin in bile is not excreted into the intestines, the stool becomes light-colored. Urine, on the contrary, darkens.
Other possible symptoms: abdominal pain, nausea and vomiting, weight loss, indigestion, deep vein thrombosis of the leg, fever. In rare cases, the tumor destroys the endocrine cells that produce insulin. Blood sugar levels rise and diabetes develops.
Major complications
Living with a benign tumor and refusing to remove it means constantly feeling the fear of possible complications. These include:
- threat of transformation into a malignant formation (malignancy),
- the formation of obstructive jaundice with severe intoxication due to obstruction of bile secretion into the duodenum,
- development of chronic pancreatitis,
- obstruction at the level of the upper small intestine,
- uncompensated endocrine disorders, hormonal shifts.
Diagnostic methods
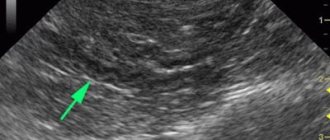
Usually, an ultrasound examination method is sufficient to detect a benign pancreatic tumor. It has been introduced into the research standard and is available in district hospitals.
An ultrasound specialist detects a hypoechoic formation with a thin wall. These are signs of a cyst prone to malignancy. If the contents are anechoic, the process is considered safe. Hyperechogenicity indicates lymphoma or lipoma.
It is important to notice an increase in infiltration in the surrounding tissues and increased vascularization. The symptom indicates an increased risk of progression to a malignant course. Benign tumors are not surrounded by many vessels.
For more accurate diagnosis, computed tomography and magnetic resonance imaging, a combination of ultrasound and an endoscopic approach are used. The techniques make it possible to detect tumor formations less than a centimeter in diameter.
Tumor markers, hormones are examined in the blood, and biochemical tests are performed to determine the functioning of the pancreas.
Treatment of a benign tumor
Treatment activities for patients with malignant and benign processes in the pancreas are organized by the oncology clinic of the regional center where the patient lives.
If necessary, the patient can be consulted with leading specialists from centers in Moscow. Once the diagnosis is confirmed, the patient is hospitalized in a specialized department, where further examination is carried out, and the question of the advisability of the operation is decided.
There is no need to waste time searching for traditional methods. It is impossible to get rid of the tumor using an unconventional method. The surgical technique offers different possibilities.
Head resection
Removal of the tumor along with part of the organ parenchyma (partial resection) is usually used for caudal tumor localization. Separate resection of the head is complicated by the common blood supply to the duodenum.
Enucleation
Removal of a delimited tumor using exfoliation from the tissue is carried out for insulinomas, gastrinomas, somatostatinomas and other neuroendocrine formations that produce hormones.
The operation is indicated for clear contours and tumor sizes less than 2 cm, located in the tail of the gland. Enucleation is not indicated for glucagonoma accompanied by pancreatitis.
It is performed laparoscopically through a minimal incision under visual control. Patients are discharged home on days 3–4 feeling well. During the rehabilitation period, a diet (table 5) and a decrease in physical activity are recommended.
Improvements in laparoscopic technology have made it possible to expand its use in regional centers. For example, in Krasnodar there are 38 clinics that are ready to perform enucleation on a paid basis.
Pancreaticoduodenectomy
Pancreaticoduodenal resection - excision of the head of the pancreatic gland together with the gallbladder, the initial part of the small intestine, part of the stomach, and nearby lymph nodes. Complex surgical interventions are performed only by high-class specialists.
More often indicated for a malignant tumor or a large node of dubious origin. The surgeon performs sequential removal of organs and the formation of an artificial duct between the remaining part of the gland and the intestine.
Gastrectomy
Complete removal of the stomach and the formation of an anastomosis with the intestines may be required for multiple ulcers caused by pancreatic gastrinoma. At the same time, resection of the affected initial part of the small intestine is performed.
Selective arterial embolization
The method is based on the introduction of a thrombotic substance into the vessels of the pancreas to stop the flow of blood to the hemangioma. This reduces the size of the tumor and prevents internal bleeding. The operation is performed under the control of computed angiography.
The resected tumor or part of it must undergo histological examination.
Treatment of benign tumors in Moscow
A benign pancreatic tumor in Moscow can be treated using the compulsory medical insurance system. To do this, referrals must be issued locally.
Residents of Moscow and the region receive all the possibilities of diagnostics and surgical care. A modern technique is the non-surgical treatment of a tumor with a CyberKnife. This is one of the types of targeted radiation effects on tumor cells.
Most often used in oncological neurosurgery. The effect on abnormal cells does not affect healthy tissue. The course requires from 1 to 5 sessions. Each procedure lasts about an hour. The method may eventually become an alternative to surgical treatment.
Israeli clinics have accumulated significant experience in using Cyber Knife. According to patient reviews, there are no side effects of therapy. Some note transient weakness and nausea.
Pancreatic adenocarcinoma
Types of pancreatic cancer include tumors of different etiologies, the most common of which is adenocarcinoma. This is a malignant formation, which includes glandular tissue. If the tumor is benign, then a pancreatic adenoma is diagnosed. Symptoms of a benign pancreatic tumor do not appear until the tumor is large.
As education grows:
hormonal balance is disrupted;- there is a feeling of heaviness in the stomach;
- a bursting sensation on the left side of the hypochondrium;
- nausea, which is accompanied by a gag reflex;
- A large tumor puts pressure on the nerve endings, causing quite severe pain.
Adenocarcinoma that develops in the interlobular ducts of the gland is called ductal (ductal, canal). In terms of prevalence, this tumor ranks third among the total number of gastrointestinal cancers.
Causes of pancreatic cancer:
- family history;
- a large amount of animal fats in the diet;
- long smoking history;
- presence of diabetes mellitus;
- development of chronic pancreatitis;
- obesity.
Often, a ductal tumor is localized in the head of the gland - up to 70% of cases. Using ultrasound and tomography, it is possible to detect a formation as small as 1 cm, that is, the early stage of pancreatic cancer. In practice, adenocarcinomas ranging in size from 2 to 5 cm are diagnosed when signs of the disease are already present. Ductal formations are grayish-yellow and do not have clear boundaries.
Often, a developing tumor puts pressure on the bile duct that passes through it. Stenosis of the main excretory duct of the pancreas may develop. It serves to transport digestive juice to the duodenum, and tumor growth into the intestinal wall is possible.
Further spread of the tumor passes through the vascular structures, affecting:
- aortic opening;
- portal vein;
- inferior vena cava.
In order for pancreatic cancer treatment abroad to be as effective as possible, diagnosticians need to accurately determine the path of tumor spread. During the diagnostic process, the histological structure of the formation is also assessed. Ductal adenocarcinomas are characterized by atypical ductal glandular structures that are well differentiated and accompanied by mucous discharge.
Types of pancreatic cancer in the context of ductal adenocarcinomas:
- adenosquamous carcinomas - such formations include flat stratified epithelium of the pancreas;
- mucinous non-cystic carcinomas - this type of carcinoma is characterized by the formation of mucinous or folded formations;
- Anaplastic or undifferentiated carcinomas - during the development of tumors, cells and tissues become undifferentiated.
The prognosis of pancreatic cancer depends on the stage of the disease, namely the presence of a metastatic process. There is no definite answer to the question of how long people live with pancreatic cancer, because the prognosis is affected by various factors, including not only the extent of the prevalence of the formation, but also the type of tumor and the age of the patient. Moreover, if proper cancer treatment is organized abroad, then doctors will take all measures to ensure the greatest possible life, even if it is stage 4 pancreatic cancer.
The process of metastasis begins with damage to nearby lymph nodes. The spread of metastases through the bloodstream leads to metastatic liver damage. With further spread, all digestive organs are affected, so treatment of stomach cancer abroad may become a necessity.
Adenocarcinomas that affect the tail and body of the gland are diagnosed less frequently. But they are the ones who pose the greatest danger, as they develop to large sizes and often affect the liver with metastases. The entry of tumor cells into the peritoneum leads to the development of peritoneal carcinosis.
Prevention of pathology and prognosis
To prevent the appearance of tumors in the pancreas, it is necessary to exclude the main causes and risk factors. Proper nutrition without canned food, fatty meats, spicy seasonings, with enough fruits and vegetables helps maintain functional order in the digestive organs.
Giving up bad habits, dry snacks, and addiction to fast food will rid the body of excess toxic substances and improve the prognosis for people at risk.
Bibliography
- Vinogradov V.V. Tumors and cysts of the pancreas. M.: Medgiz, 1959.
- Danilov M.V., Fedorov V.D. Pancreas surgery. M., Medicine, 1995
- Zollinger R. Atlas of surgical operations M., 2002.
- Beger H.G., Prokopchuk O. Benign tumors of the pancreas - limited surgical operations for cystic and neuroendocrine neoplasms, revision of surgical interventions. Annals of surgical hepatology. 2015 No. 20 pp. 73–89.
- Danilov M.V., Fedorov V.D. Repeated and reconstructive surgeries for diseases of the pancreas. M., Medicine. 2003
- Bozhenkov, Yu. G. Practical pancreatology. Guide for doctors M. Med. book N. Novgorod Publishing House NGMA, 2003
Features of the appearance of neoplasms
The pancreas is an element of the human digestive system. Plays a key role in the process of digesting substances necessary for human life. Located in the abdominal cavity, it has an oblong curved shape, vaguely reminiscent of a bean pod. It is divided into three components: head, tail, body. All malfunctions of the gland lead to insufficient production of necessary hormones, disruption of the endocrine and digestive systems.
The pancreas is a “fragile” organ in the human body, easily susceptible to diseases of various etiologies: infectious and other inflammations, the appearance of benign formations, and oncology.
Scientists are struggling with the problem of the occurrence of tumors in the body, but the causes of the pathological process remain unclear. It is known that at a certain moment a cell appears with an incorrect DNA structure. If a person’s immunity is fully functioning, such a cell is immediately destroyed. Another way of development of events is possible: a malfunction of the body occurs, malignant cells capture new territories.
According to statistics, pancreatic tumors are more common in men after 60 years of age. Women and young people are less susceptible to the appearance of neoplasms in the organs of the digestive system. A typical portrait of a person at risk is a man over retirement age, with an addiction to smoking and alcohol and a history of chronic diseases of the pancreas, liver and digestive tract.
The tumor can cover the entire surface of the organ, be located inside or affect individual areas of the pancreas. The International Classification of Diseases divides neoplasms depending on their location in the organ. The tumor can affect areas of the gland:
- tail;
- body;
- head;
- duct;
- islet cells;
- other parts;
- may have blurry outlines.
A tumor of the head of the pancreas is diagnosed in more than half of the cases of its occurrence. About a quarter of neoplasms affect the body or tail of the organ.