Physiology of motility of smooth muscle organs
Most organs in which the process of peristaltic contractions occurs have two layers of smooth muscle in their walls, in one of them the muscle fibers are located longitudinally, in the other - circularly. The coordinated contractions of these muscles form a peristaltic wave. Smooth muscles, unlike striated muscles, contract relatively slowly. Their contractions are involuntary, that is, they cannot be controlled by consciousness.
For example, the muscles of the digestive tube organs are smooth, with the exception of the “input” (striated muscles are present up to the upper third of the esophagus) and the “output” (external sphincter of the anus). Therefore, after the start of swallowing and before the act of defecation, all processes associated with the movement of food, including peristalsis, are not controlled by consciousness.
The frequencies of peristaltic waves are different in different organs (departments). They are set by special pacemakers - clusters of nerve cells, among which the leading role is played by the interstitial cells of Cajal. Pacemakers generate slow waves of transmembrane potentials. Slow waves do not cause muscle contractions, but create a potential in the muscles close to the activation threshold. When slow waves of action potentials occur on a plateau, the muscle fiber contracts.
Pacemakers thus determine the frequencies of peristaltic waves (as well as other phasic contractions). In a healthy person they are as follows (in cycles per minute): in the stomach - 2-4, in the duodenum - 10-12, in the jejunum - 9-12, in the ileum - 6-8, in the colon - about 0, 6, as well as 3-4 and 6-12, in the rectum - about 3, in the sphincter of Oddi - 3-6.
In the small intestine, there are several types of waves that differ from each other. The speed of their passage can be smooth, slow, fast, and also rapid. As for the large intestine, the food bolus moves much more slowly, so the speed of the waves themselves decreases. Very strong contractions appear several times a day, which are what pushes food towards the anus.
Movements in the colon appear after the stomach cavity is filled.
If intestinal motility is disrupted, the absorption of vitamins and minerals is noticeably inhibited, food passes through the intestines with difficulty, and constipation develops. This condition requires urgent treatment, otherwise the situation will worsen. Against the background of slow peristalsis, food accumulates and becomes a source of toxins, bacteria, and parasites. If treatment is not started in time, the pathology provokes a number of diseases of the digestive tract.
The digestive system is one of the main mechanisms in human life. But at the same time, her organs begin to lose their functions first. An important point in the functioning of the gastrointestinal tract is intestinal motility. It can be strong or weak, but in any case, if violated, it causes a lot of unpleasant sensations.
Peristalsis is contraction of the intestinal muscles aimed at moving food masses throughout the organ.
Intestinal peristalsis is understood as wave-like contractions of the intestinal walls, which help push masses of feces towards the anus. This is one of several types of motor activity that occur in the intestines. It is thanks to the correct contractions that normal digestive processes are realized, during which all the necessary microelements are absorbed, and what is not absorbed leaves the body.
In order to maintain the normal functioning of the gastrointestinal tract for a long time, you need to monitor your diet, introduce physical activity and eliminate bad habits. In addition, it is necessary to promptly treat systemic diseases that affect the performance of the organ. If these conditions are not met, then peristalsis may be increased or, conversely, decreased, which is far from the norm.
Peristalsis begins to occur after the stomach has been filled with food. The norm is considered to be the case when 10-12 contractions occur per minute in the duodenum, 9-12 in the small intestine, 3 contractions in the large intestine, and no more than 3 in the rectum. If the patient experiences disturbances in peristaltic activity, they may constipation or diarrhea occur.
Treatment of intestinal motility disorders
To restore the functioning of the digestive organs, an integrated approach is used, which includes changes in diet and physical exercise. In case of chronic constipation and fecal hardening, drug therapy is indicated.
Medicines
First of all, it is necessary to cleanse the digestive tract of stagnant feces. For this purpose, laxative medications are prescribed (Guttalax, Phenolphthalein, Duphalac), presented on the pharmaceutical market in various forms - in the form of tablets, drops, rectal suppositories.
Natural laxatives are rhubarb roots, licorice, buckthorn bark, and senna leaves. Herbal-based drugs include Regulax.
Potent agents used when it is impossible to empty are Epsom and Glauber's salts. They affect the entire intestine, producing the desired effect within a couple of hours after administration.
Castor oil softens the food bolus and facilitates its movement towards the anus. The effect is usually observed after a few hours.
You should not get carried away with laxatives: they are addictive, the digestive organs can “forget how” to work independently, without external stimuli.
Proserin, Vasopressin, Aceclidine have a strengthening effect on the intestinal muscles. They enhance motor activity, stimulating the passage of food through the digestive tract.
Digestion is aided by Mezim, Festal, Creon, which are not recommended to be taken for longer than 10 days.
To correct psychosomatic disorders, sedatives and antidepressants are prescribed.
All medications, their dosage and treatment regimen are prescribed by a specialist. Replacing the medication or stopping it early is possible only after a re-examination. Self-use of any pharmaceuticals is prohibited!
Physiotherapy
An active lifestyle helps restore the motor skills of internal organs. Running, swimming, hiking, horse riding, and abdominal exercises will bring your intestines back to normal.
Regarding physical activity that is unusual for you, please consult with a physical therapy specialist first!
A set of exercises to strengthen motor skills:
- from a lying position (you can lie in bed immediately after waking up. It is important that the surface is not too soft!) lift your body;
- lying on your back, raise your knees bent at an angle of 90 degrees and perform the exercise “riding a bicycle”;
- remaining in the same position, grab your bent knees with your hands and pull them to your chest;
- lower your bent legs to your feet and lift your pelvis;
- in a kneeling position with emphasis on your palms, alternately move your legs back;
- from a kneeling position with emphasis on your elbows, alternately sit on your right and left buttocks;
- from a standing position, slow squats with the pelvis moving back;
- jumping with or without a skipping rope (in the absence of pathologies of the pelvic organs).
To reduce intestinal motility, abdominal exercises should be avoided. In this case, stretching will do.
Daily abdominal massage will also stimulate the functioning of the gastrointestinal tract.
A contrast shower or dousing with cold water followed by intensive rubbing with a terry towel also has a beneficial effect on the body.
Dietary recommendations
A necessary and effective method of treating the disease is to follow a diet based on the inclusion of plant fiber in the diet and reducing the consumption of high-calorie carbohydrate foods.
Basic rules for impaired dysfunction:
- It is better to eat more than 3 times a day (4-5) in small portions. Food must be chewed thoroughly;
- drink enough fluid (at the rate of 30 ml per 1 kg of weight in the absence of kidney problems). Get into the habit of drinking a glass of water at room temperature in the morning: this method will help the intestines start working;
- exclude from the menu foods rich in simple carbohydrates (sweets, especially chocolate, flour, fast food), starch (potatoes, rice, semolina), as well as irritating mucous membranes (carbonated drinks, fatty and fried foods, pickles, smoked foods, canned foods, sour fruits);
- use butter, boiled eggs, and legumes with caution, which increase gas formation;
- you will have to limit the intake of strong tea and coffee, hot drinks;
- to enhance motor skills, fresh vegetables (cabbage, carrots, beets) and fruits (green apples, apricots, plums), bran, cereals, flax seeds, oatmeal and buckwheat porridge, herbs, berries are shown;
- for cooking, use vegetable oils (preferably cold pressed): olive, linseed;
- freshly squeezed juices (especially carrot, cabbage and beetroot, as well as berries), compotes, fermented milk products, dried fruits are useful;
- If possible, eat more seafood and seaweed.
List of recommended products for increased peristalsis:
- pureed soups;
- porridge from barley, rice, semolina;
- dishes from lean meats, eggs;
- vegetable purees;
- astringent fruits and berries (quince, pear, bird cherry, chokeberry).
In any case, you will have to give up cigarettes and alcohol.
Traditional medicine
Non-traditional methods can effectively complement the main treatment: cleanse the clogged intestines, restore its motor function, stimulate the healing of damaged tissues and get rid of pathogenic bacteria.
Before using folk remedies, you need to consult a specialist!
Recipes for constipation:
- bran, fiber, which can be eaten separately or added to various dishes (salads, soups, cereals, jelly) 1-2 tablespoons per day;
- beet salad with prunes or garlic;
- a mixture of prunes and dried apricots. Grind 400 grams of seedless dried fruits in a meat grinder, adding 2 tbsp. propolis tinctures, senna leaves (1 pack) and 200 ml of fresh, not candied honey. All ingredients must be mixed thoroughly. Take 2 tsp. at night, with water at room temperature;
- A decoction of buckthorn bark is drunk instead of tea;
- crushed plantain seeds: 1 tsp. before eating.
Peristalsis as a physiological phenomenon
It is impossible to understand how the digestive system, and indeed the entire human body, works without an understanding of such a phenomenon as peristalsis. The word has Greek roots and means “to grasp and squeeze.” It describes the phenomenon of sequential wave-like contractions of muscles in the human body to transport certain substances. As a rule, the walls of organs capable of peristalsis have two layers of smooth muscle.
One of them is located longitudinally, and the second is circular. The autonomic nervous system provides the necessary coordination of these muscles, resulting in consistent movement. Peristalsis is the mechanism that ensures the movement of food along the digestive tract from the mouth to the anus.
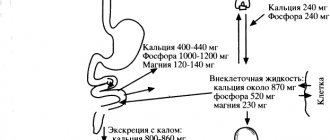
Thanks to this mechanism, food moves through the esophagus into the stomach, from there into the small intestine, and then into the large intestine, with its help defecation is carried out. Peristalsis also ensures the supply of fluids to the digestive tract, without which the digestive process would be impossible: bile from the liver and gallbladder, pancreatic juice from the pancreas. Peristalsis refers to the properties of the muscles of the urinary tract and fallopian tubes.
This article is devoted to the peristalsis of the gastrointestinal tract, in particular the intestines, so it needs to be given special attention. In each section of the gastrointestinal tract, peristaltic waves have their own specifics. In the esophagus, they simply deliver food to the stomach. If the next wave begins when the previous one is not yet finished, it extinguishes it. This is why gastroenterologists advise eating slowly and chewing food thoroughly. The motor function of the stomach not only transports food from the exit of the esophagus to the entrance to the duodenum, but also mixes and grinds it.
Through the pylorus, food passes from the stomach into the duodenum, the first section of the small intestine. Peristaltic waves in the small intestine occur due to stimulation by food. There are several types of them, all of them differ in speed: very slow, slow, increased and rapid. At any given time, several waves move in the small intestine. The fastest motility occurs in the duodenum, in the jejunum it is reduced, and in the ileum it is the lowest. As in the stomach, in the duodenum the digested food (chyme) not only moves forward, but is also mixed.
4
1. Indicate the main features of membrane digestion: + occurs under practically sterile conditions, – occurs with the participation of intestinal microflora, + is carried out by enzymes fixed on the membrane of the intestinal brush border, – provides initial hydrolysis of supramolecular aggregates and large molecules, + high degree of interaction between the digestion and absorption of food substrates , - carried out primarily by pancreatic enzymes.
2. Indicate the possible reasons for the development of gastric hyposecretion: – increased parasympathetic stimulation of the stomach, + damage to the lining cells of the gastric mucosa, + decreased production and release of gastrin, – increased production and release of histamine, – decreased production and release of secretin, + increased formation of enterogastron, – decreased secretion of cholecystokinin.
3. Indicate the gastrointestinal hormones, the excess of which causes hypersecretion of pancreatic juice: – gastrin, + cholecystokinin, + secretin, – motilin.
4. Indicate the possible reasons for the decrease in the secretory activity of the pancreas: – increased parasympathetic stimulation of the gland, + weakened parasympathetic stimulation of the gland, + decreased production and secretion of cholecystokinin, – increased production and secretion of cholecystokinin, + decreased production and secretion of secretin, – increased production and secretion of secretin , + gastric achylia, + acholia.
5. How will the evacuation of food masses from the stomach change with a simultaneous increase in the secretion and acidity of gastric juice? + will slow down, – will speed up.
6. How will the evacuation of food masses from the stomach change with a simultaneous decrease in the secretion and acidity of gastric juice? – will slow down, + will speed up.
7. Indicate the consequences of achlorhydria of gastric juice: + reduction in the secretion of secretin by the mucous membrane of the duodenum, + reduction in the activity of peptic enzymes of gastric juice, – slowdown in the evacuation of food masses from the stomach into the intestine.
8. The absorption of which vitamins will significantly worsen with acholia? + vitamin A, – vitamin B1, – vitamin B2, – vitamin B12, + vitamin D, + vitamin E, + vitamin K, – folic acid.
9. Which of the following digestive disorders can cause steatorrhea? – insufficiency of digestion and absorption of carbohydrates, + insufficiency of synthesis of pancreatic and intestinal lipases, – insufficiency of trypsinogen synthesis in the pancreas, + acholia.
10. Indicate the consequences of acholia: + deterioration of digestion and absorption of fats, – deterioration of absorption of water and electrolytes, + disruption of the activity of intestinal microflora, – increased secretion of pancreatic juice, – increased intestinal motility, + weakened intestinal motility, + deterioration of protein digestion, + deterioration of digestion carbohydrates.
11. Indicate the possible reasons for the development of gastric hypersecretion: + excessive parasympathetic stimulation of the stomach, – increased production and release of somatostatin, + increased production and release of gastrin, – deficiency of gastrin production, + increased formation and release of histamine in the stomach wall, – increased histaminase activity
12. Indicate the main reasons for the development of malabsorption syndrome: + atrophy of small intestinal microvilli, + extensive resection of the small intestine, – hyperacid gastritis, + chronic enteritis, + acholia, – cholecystectomy.
13. Name the manifestations of intestinal malabsorption syndrome: + weight loss, asthenia, – vomiting, belching, heartburn, + polyhypovitaminosis, – arterial hypertension, + anemia, + edema, – obesity, + immunodeficiencies.
14. Indicate the possible causes of intestinal autointoxication: – hyposecretion of gastric juice, + hyposecretion of pancreatic juice, – increased evacuation function of the intestine, + weakening of the evacuation function of the intestine, + extensive damage to the microvilli of the small intestine, – hypertrophy of the microvilli of the small intestine, + acholia.
15. Which factor is usually more important in the pathogenesis of duodenal ulcer? + acid-peptic aggression, – decrease in the protective properties of the intestinal mucosa.
16. What conditions are typical for pancreatic achylia? – polyhypovitaminosis A B C E, + creativeorrhea, + hyporexia, + steatorrhea, – bulimia, + amilorrhea.
17. In protecting the gastric mucosa from the acid-peptic aggression of gastric juice, the following roles play a role: + synthesis of Pg by the cells of the mucous membrane, + secretion of bicarbonate, – synthesis of internal factor, – restriction of blood flow in the stomach wall, + secretion of mucus containing mucin.
18. What mechanisms play a significant role in the pathogenesis of peptic ulcers of the stomach: + damage to the mucous membrane by bile acids and lysolecithin during reflux of intestinal contents, + decrease in the basal tone of the pyloric sphincter, – decrease in parasympathetic influences on the gastric mucosa, + increased reverse diffusion of H+ into the mucosa , + effect of Helicobacter pylori on the protective layer of the mucous membrane, + increased acidity of gastric juice, + inhibition of Pg synthesis by mucosal cells.
19. Which of the listed factors play a significant role in the pathogenesis of stomach ulcers under stress? + increased tone of the vagus nerve, + increased secretion of gastric juice, – increased synthesis of PgE2 by gastric epithelial cells, – increased mucus production, – increased vascular permeability, + weakened epithelial regeneration.
20. Indicate the factors involved in the pathogenesis of belching: + fermentation and putrefaction in the stomach, + increase in intragastric pressure, – cardiospasm, + pyloric spasm, + reflex contraction of the muscles of the stomach and diaphragm, + reflex contraction of the abdominal muscles.
21. What conditions lead to increased intestinal motility? + achylia, – decreased tone of parasympathetic nerves, + increased excitability of intestinal wall receptors, + inflammation of the gastrointestinal tract (enteritis, – constant consumption of foods low in fiber.
22.What types of pathological secretion of the stomach are known? + asthenic – normal + excitable + inert + inhibitory
23. Hyposalivation can be a consequence of: – toxicosis of pregnancy – nausea and vomiting – the action of vegetative poisons (pilocarpine) + mumps + fear, anxiety
24. Hypersalivation can be a consequence of: – dehydration of the body – formation of stones in the salivary ducts + helminthiasis + inflammatory process in the oral cavity and stomach + bulbar paralysis
25. The asthenic type of gastric secretion is characterized by: + increased excitability of the gastric glands to mechanical irritation - increased excitability of the gastric glands to chemical irritation + rapid exhaustion of the gastric glands - the total amount of gastric juice is higher than normal - pH of the gastric juice 4.0 - 6.5
26.What digestive disorders are observed with hypersecretion and increased acidity of gastric juice? + fermentation processes develop in the stomach - diarrhea - the amount of food gruel entering the intestines increases + belching + heartburn
27.What is characteristic of ahilia? + duodenal digestion is disrupted – secretion of secretin increases – constipation – weakening of intestinal motility – prolonged spasm of the pylorus
28.What is characteristic of the excitable type of gastric secretion? – increased secretion to mechanical and decreased secretion to chemical stimuli + increased acidity of gastric juice – increased time of soda test – pH of gastric juice on an empty stomach 3.0-5.0 + after a test breakfast, the pH is restored to the original level after 12-18 minutes and continues to gradually decrease over the next 1-2 hours
29.Name the reasons for the development of hypo- and acholia. + blockage or compression of the common bile duct + disorder of the bile-forming function of the liver – disorder of fat metabolism – disorder of portal circulation – disorder of the antitoxic function of the liver
30.What processes will develop if bile secretion is impaired? – increased absorption of fatty acids – increased absorption of cholesterol + steatorrhea + flatulence + decreased intestinal motility
31.Name the causes of violation of the exocrine function of the pancreas. + duodenitis + inflammatory processes + blockage or compression of the pancreatic duct – impaired fat absorption – impaired protein digestion
32.What processes develop during pancreatitis? + steatorrhea – hypertension + disruption of digestive processes in the intestines – the content of diastase in the urine decreases + hypotension
33.What is the reason for the slowdown in absorption in the small intestine? + with impaired regeneration of the intestinal mucosa + with ischemia of the intestinal wall + with impaired parietal digestion – with active breakdown of food masses in the stomach + with the development of pancreatitis
34.What should be classified as disorders of the motor function of the stomach? + hypertonicity of the stomach + gastric atony + heartburn + belching + hiccups + vomiting
35.When is parietal digestion disrupted? – with activation of cavity digestion + with impaired intestinal motility + with acholia + with acute intestinal infections + with the action of toxic substances
36. Indicate the origin of enzymes that carry out parietal digestion. + adsorbed from chyme + synthesized by enterocytes – supplied with blood proteins – transported to the brush border by blood cells
37. Specify the reasons for the acceleration of intestinal motility. – vitamin deficiency B-1 – increased acidity of gastric juice – food intake poor in fiber – poor nutrition + inflammatory process in the intestines
38. Specify the reasons for the slowdown in peristalsis. + lead poisoning – inflammatory process in the intestines – effect of fermentation and putrefaction products on the intestinal wall – achylia – increased excitability of the center of the vagus
39.What factors cause disruption of intestinal membrane digestion? – adrenaline + disruption of microvilli structure – cholesterol + intestinal motility disorders + effect of cytostatics
40. Indicate the mechanism of development of dumping syndrome. + reflex influence from the jejunum during its rapid overfilling – development of the Bainbridge reflex – with severe mental shock, the influence of the cerebral cortex on intestinal motility is lost – suppression of the activity of the food center – congenital disorder of peristalsis (with Hirschsprung’s disease)
41.What is the manifestation of increased vagal influence on the functions of the stomach? + the secretion of hydrochloric acid increases - the motor function of the stomach decreases + the formation of pepsin increases + the level of histamine increases - the secretion of gastrin decreases
42.What is the reason for the violation of the protective properties of the gastric mucosa? – with a decrease in the production of hydrochloric acid + with a decrease in mucin synthesis + with a decrease in the production of prostaglandins – a decrease in the effect of glucocorticoids + microcirculation disturbance
43. Mechanisms of pathogenesis of gastric ulcer? + disturbance of neurohumoral regulation + decrease in the protective properties of the gastric mucosa + activation of endogenous aggressive factors - decrease in pepsin production + influence of bacterial factors
44. Clinical symptoms of gastric ulcer? – intestinal paresis + pain + vomiting + heartburn – decreased blood pressure
45. Is the general acidity of gastric juice normal? – 20-40 units. – pH 7.4 – 120-160 units. + 60-80 units. – pH7.2
46. The main causes of digestive disorders include: + alcohol abuse and smoking + mental trauma + nutritional errors – heart failure – hypervolemia
DIGESTIVE SYSTEM
1. Damage to hepatocytes (cytolysis syndrome) can be diagnosed based on: + increased transaminase activity increased cholesterol levels increased alkaline phosphatase levels increased beta lipoprotein levels increased urokinase levels
2. Cholestasis syndrome is characterized by: + increased cholesterol levels + increased beta lipoprotein levels increased transaminase activity + hyperbilirubinemia + increased liver size increased spleen size
3. The formation of intestinal dysbiosis is promoted by: + early transfer to artificial feeding long-term breastfeeding + prescription of antibiotics + intestinal infections + disorders in the immune system
4. Pain syndrome with dyskinesia of the biliary system of the hypotonic type is characterized by: + constant bursting pain in the right hypochondrium, dull bursting pain in the umbilical region, paroxysmal short-term pain in the right hypochondrium, late pain in the upper half of the abdomen, sharp girdle pain
5. Characteristic clinical symptoms of gallbladder damage are: abdominal pain + pain in the right hypochondrium, symptoms of intoxication, nausea, vomiting, pain in the epigastrium, nausea, heartburn, girdle pain, repeated vomiting, pain in the left iliac region, symptoms of intoxication, tenesmus, pain after heavy physical activity, eating fatty foods
6. Clinical signs of gastrointestinal bleeding are: + vomiting “coffee grounds” severe flatulence + tarry stools + general weakness high fever
7. Pain syndrome with hypertensive biliary dyskinesia is characterized by: constant bursting pain in the abdomen, dull bursting pain in the umbilical region + paroxysmal short-term pain in the right hypochondrium, late pain in the upper half of the abdomen, sharp girdle pain
8. Symptoms characteristic of damage to the stomach and duodenum: Kera + Mendel Murphy Ortner-Grekov Mussi-Georgievsky
9. Symptoms characteristic of gallbladder damage: + Kera Mendel + Ortner-Grekov Mayo-Robson + Murphy + Skvirsky
10. Pain characteristic of damage to the duodenum: early early and late early and nocturnal + late and nocturnal
11. Intestinal dysbiosis is understood as: inflammation of the mucous membrane of the small intestine, inflammation of the mucous membrane of the large intestine + qualitative and quantitative disturbances in the composition of microorganisms that normally populate the gastrointestinal tract + quantitative disturbances in the species composition of the microflora, acute intestinal infection
12. When the pancreas is damaged, pain is characteristic at the following points: Kera Porges Openkhovsky + Mayo-Robson Boas + Kacha
13. The equivalent of abdominal pain in an infant is: increased body temperature oliguria regurgitation and vomiting loose stools + anxiety + breast refusal
14. Astheno-neurotic syndrome with damage to the digestive system is characterized by: + headache, pain in the paraumbilical area + fainting, vomiting + dizziness, anorexia
15. Endogenous intoxication syndrome with damage to the digestive system is characterized by: constipation, unstable stool + pallor + fever + headache, bulimia
16. Malabsorption syndrome is characterized by: + copious loose stools, gastrointestinal bleeding, pain in the epigastric region of the abdomen, flatulence + decreased body weight of the child + steatorrhea
17. Early abdominal pain occurs: + immediately after eating + 30 minutes after eating on an empty stomach 1-2 hours after eating at night
18. Late abdominal pain occurs: immediately after eating 30 minutes after eating + on an empty stomach + 1-2 hours after eating + at night
19. With the Moiningan rhythm of pain, food intake: + brings relief increases pain does not affect the intensity of pain
20. Gastric dyspepsia is characterized by: + belching + heartburn + nausea + vomiting diarrhea
21. Intestinal dyspepsia is characterized by: belching heartburn nausea vomiting + diarrhea
22. Damage to the colon is characterized by: + pain associated with defecation, girdle pain, uncontrollable vomiting, steatorrhea + mucus in the stool
23. Damage to the pancreas is characterized by: pain in the umbilical region + girdle pain + uncontrollable vomiting + steatorrhea, mucus in the stool
Peristalsis of the gastrointestinal tract
Peristalsis of the hollow organs of the human gastrointestinal tract (GIT) plays a critical role in the process of digestion and the movement of food from the upper to the lower sections. At the same time, peristaltic contractions are not the only type of motor activity of most of these organs. For each of them, the role of peristalsis and its contribution to general motor activity is different.
Peristaltic contraction for the digestive organs refers to synchronized contractions of the organ wall, spreading from its “entrance” to the “exit” and moving more or less digested food in the same direction. For tubular organs (that is, all organs of the digestive tube, except the stomach), it is assumed that peristaltic contractions completely or almost completely block the lumen of the organ.
Peristalsis is usually called a wave-like contraction of the walls of the intestine (small and large), which leads to the movement of food, chyme or feces in one direction. Peristalsis is a reflex act that involves intestinal muscle fibers. Their coordinated movement, controlled by the nervous system, creates a contractile wave. The frequency of formation of such waves in different parts of the intestine is different. Peristalsis also occurs during the interdigestive period.
This term refers to the rhythmic contractions of the muscular walls of the intestine, which promote the movement of food masses from the thin to the thick section. This factor plays an important role in the processes of absorption of nutrients and removal of waste products from the body.
Peristaltic contractions involve smooth muscle fibers that are present in the intestinal walls. One layer is located longitudinally, the other - transversely. Coordinated contractions contribute to the creation of waves, the frequency of which is different in different parts of the organ. Several types of contractile movements spread throughout the small intestine, which differ in speed. They can be slow, medium and fast. Often several types of waves appear simultaneously.
Food masses move slowly through the large intestine; peristaltic waves in this section have the lowest speed. 1–2 times a day, rapid contractions occur in the organ, promoting the movement of feces towards the anus. Peristalsis of the colon is based on a reflex that occurs when food enters the stomach. The normal frequency of contractions of the duodenum is 10 times per minute, small - 9-12 and large - 3-4. At the moment food moves towards the anus, the frequency indicator increases to 12.
Weak peristalsis slows down the absorption of nutrients and makes it difficult to move feces towards the rectum. Remains of undigested food, feces and toxins linger in the body, gradually poisoning it and creating ideal conditions for the proliferation of pathogenic microorganisms.
Impaired intestinal motility is the cause of most pathologies of the digestive system, characterized by constipation and diarrhea, abdominal pain, ulcers and benign neoplasms.
Normal contraction motility is possible due to the presence of smooth muscle fibers on the intestinal walls. They are located in several layers, some longitudinally, others transversely. Due to systematic contractions, waves of different intensities are created. In different parts of the intestine, the speed of movement of food masses differs.
Normally, the number of contractions per minute is 10 times in the duodenum, 9–12 in the small intestine, and 3–4 in the large intestine.
Intestinal peristalsis functions not only after eating, but also constantly, even at night. Several times a day, rapid contractions occur that push the contents of the intestines towards the anus. The first alarming sign of impaired peristalsis is often problems with stool, especially constipation, when motility does not reach the desired speed and waste products do not reach the rectum.
Diagnostics
Modern modifications of X-ray examination with contrast make it possible to accurately determine the types of motor activity of the stomach: tone, peristalsis, evacuation rate, the presence or absence of esophagogastric or duodenogastric reflux.
A method for recording biopotentials or electrogastromyography , based on recording signals that can be used to judge the motor activity of the gastrointestinal tract.
Balloonographic method . A balloon with a probe and an electromanometer is inserted into the stomach. The device records the vibrations that the gastric wall causes when it contracts to the medium (water or air) inside the balloon.
The open catheter method is recognized as the simplest, physiological and at the same time informational way to study disorders of motor activity of the stomach and intestines. A catheter filled with a special solution is inserted into the gastric cavity. A column of fluid senses and transmits changes in pressure in the stomach. These fluctuations are displayed graphically. The method makes it possible to evaluate the muscle tone of the organ, the frequency, amplitude and rhythm of contractions.
Normal peristalsis
The rate of muscle contraction in the small intestine is different from that in the large intestine. Depending on the situation, food gruel can move at a rate of contraction of the walls of the small intestine from 8 to 10 times per minute. In the large intestine, where feces are formed, the contraction rate is slower and ranges from 3 to 4 times per minute. Pathological changes that lead to faster or slower contractions lead to problems with bowel movements (diarrhea or constipation).
Video on the topic:
Causes of impaired motor function of the stomach
Changes in the tone of the muscular lining of the organ:
- increase – hypertonicity ;
- decrease – hypotonicity;
- complete lack of tone - atony .
This leads to a failure in the forward movement of chyme through the sections of the stomach to the duodenum. Violation of gastric motility in the form of hyperkinesis (increased) or hypokinesis (slowed down) of the process.
The causes of impaired gastric motility are various pathological processes: gastritis, erosion, ulcers, scars, tumors, polyps. Depending on the location of painful foci and their prevalence, peristalsis weakens or intensifies.
Gastric motility also suffers when there is a disorder in the humoral and nervous regulation of the motor activity of the organ. An increased concentration of hydrochloric acid, as well as the hormones secretin and cholecystokinin, slow down motility, and the secretion of gastrin and motilin, on the contrary, enhance peristalsis.
With the predominant influence on the smooth muscles of the stomach of the parasympathetic part of the autonomic nervous system (vagus nerve), motility increases, and activation of sympathetic fibers suppresses motor activity.
What leads to impaired peristalsis
There are many reasons (from minor to serious) that lead to impaired motor skills:
- changes in diet and water imbalance;
- constant stress;
- bad habits;
- side effects of certain medications;
- intestinal infection;
- previous operations on the gastrointestinal tract;
- helminthic infestations;
- pregnancy;
- oncological diseases of the intestine, etc.
As a rule, impaired peristalsis in the form of diarrhea or constipation is just a symptom of a disease. “Irritable bowel syndrome” is an example of a disorder of nervous and humoral regulation. With it, under the influence of negative emotions, the motor and absorption function of the intestine changes, which is accompanied by either constipation or diarrhea.
Prolonged diarrhea is a health condition that causes loss of electrolytes and fluids, disrupts the mineral balance in the body and contributes to dehydration.
Hyperperistalsis symptoms
Gastric hyperperistalsis is a symptom. It may be accompanied by many other symptoms or occur on its own. Given that the term "belly churning" is a bit vague at times, it can also be loosely used to describe nausea, bloating, and occasional abdominal cramps.
We all know some of the normal stomach sensations we experience throughout the day, especially when we are hungry or after eating. When we are hungry, we experience hunger pangs, sometimes burning sensations and strong contractions. In many ways this is normal. When we eat well, we feel a feeling of fullness in our stomach. Sometimes there is a feeling of bloating from overeating and gurgling sounds in the stomach. To a large extent, this is also normal.
Abnormal sensations in the stomach can vary in nature and intensity. A feeling of extreme squeezing or bloating is not normal. There may also be a burning sensation, dull ache, or pain in the abdomen. Mild contractions when hungry or after eating can be normal, as can audible sounds in the stomach. However, excessive and forceful contractions with/without abnormally loud sounds are not normal. This is largely what is perceived as stomach churning along with the other symptoms discussed below.
Other symptoms
- Nausea is one of the common symptoms that accompany stomach churning.
- In some cases, nausea may be accompanied by vomiting.
- Bloating with a feeling of fullness (“bloating”) in the upper abdomen.
- Borboryla (stomach noises) that are excessively loud and/or prolonged.
- Changes in bowel habits, such as diarrhea or constipation.
- Excessive gas formation in the form of frequent belching or flatulence.
- Abdominal pain or cramping, which in some cases can be described as churning in the abdomen. Also refer to stomach cramps.
- Heartburn, which is a burning pain in the chest due to reflux (increased levels of stomach acid in the esophagus).
Increased and weakened peristalsis
Increased intestinal motility occurs when contraction of the intestinal walls occurs too often. As a result, food does not have time to be completely digested, and beneficial microelements obtained from food do not have time to be completely digested. Because of this, food masses enter the anus with difficulty, which causes constipation. And there is also a deficiency of many useful substances.
Weakened intestinal motility is an equally serious disorder in which the number of contractions of the intestinal walls occurs less frequently than normal. As a result of insufficient rhythm, food lingers in the intestines longer than necessary. The consequences are the same as in the case of increased peristalsis: constipation and other disturbances in the gastrointestinal tract appear.
The causes of all types of violations may be the same factors. Both increased and weakened peristalsis leads to complications, disruptions in the digestion of food and the absorption of beneficial microelements.
Advice from a gastroenterologist
Disturbances in the motor activity of the stomach and the entire digestive system as a whole can be both functional and pathological in nature.
The doctor has all the tools at his disposal for timely detection of the disease and prescribing adequate treatment. Therefore, at the first signs of discomfort in the gastrointestinal tract, you should seek advice from a medical institution, and not try to cope with the problem with painkillers or traditional medicine.
Intestinal atony or decreased peristalsis
Atony translated from Latin means lack of tone. Intestinal atony is associated with loss of muscle tone, resulting in excessive relaxation of the intestines, leading to constipation. Often the cause of loss of tone is errors in eating food with insufficient fiber content. In addition, psychogenic, endocrine, and toxic causes of atony and constipation are distinguished.
We are talking about intestinal atony if a person has not had a bowel movement for more than 2 days. Obvious symptoms of constipation include:
- abdominal pain;
- bloating, flatulence;
- general discomfort;
- loss of appetite.
Stool retention does not go away without a trace: fecal stones form and pathogenic microflora multiply. Harmful substances enter the bloodstream, poisoning the body. Against the background of constipation, the intestinal mucosa becomes inflamed, the biocinosis of beneficial microorganisms is disrupted, which predisposes to the development of intestinal cancer.
Symptoms of increased intestinal motility
The symptoms of hyperperistalsis are similar to those of an intestinal disorder. A person experiences the following discomfort:
- pain in the epigastric region of varying severity;
- bloating, flatulence;
- frequent stools (not necessarily loose);
- bowel dysfunction: diarrhea most often occurs, but sometimes constipation may develop;
- decreased overall tone due to constant discomfort;
- changes in body weight due to malabsorption of nutrients.
It is noteworthy that pain, bloating and rumbling in the abdomen begin immediately after eating, even before the chyme enters the intestines. The fact is that intestinal contractions begin not from the moment food enters it, but from the moment the meal begins.
At an early stage of pathology development, a person may ignore the symptoms, since they are not too pronounced. But gradually a person’s well-being deteriorates, the constant process of fermentation in the intestines provokes intoxication of the body, due to insufficient absorption of vitamins and microelements, vitamin deficiency and various pathologies develop.
Types of physiological contractions
- Rhythmic segmenting. When circular fibers work, the intestinal contents are sequentially divided into segments, mixed and processed by digestive juices.
- Pendulum-shaped - movement of the food bolus back and forth.
- Wave-shaped peristaltic - move digested food towards the exit. The waves can be slow (speed 0.1-0.3 cm/s) and fast (speed up to 21 cm/s).
- Tonic - longitudinal muscles contract and narrow the intestinal lumen.
Regulation
Intestinal motility is the result of the coordinated work of hormones, the autonomic and central nervous systems:
- cells of the neuromuscular plexus of the intestinal wall provide background rhythmic activity;
- motility is enhanced by the influence of food breakdown products;
- irritation of rectal zone receptors inhibits upper motor skills;
- food intake first reflexively inhibits, then stimulates the motor activity of the intestines;
- hormones that enhance motility: gastrin, histamine, vasopressin;
- hormones that reduce motility: secretin, vasoactive intestinal peptide.
With normal intestinal motor function, the digestion process lasts from 1 to 3 days.
Weak motor skills
Decreased motility leads to infrequent and insufficient bowel movements. Chronic constipation appears.
Symptoms
- defecation less than once every 3 days;
- small amounts of hard feces;
- the need to strain hard during bowel movements;
- aching pain in the abdomen;
- bloating;
- decreased appetite;
- irritability, drowsiness.
Causes
- An unbalanced diet - lack of plant fiber, excess carbohydrates, pureed food, poor drinking regime.
- Physical inactivity. With a sedentary lifestyle, smooth muscle tone decreases.
- Pregnancy. The hormone progesterone relaxes smooth muscles. 50% of women suffer from constipation during pregnancy.
- Elderly age. More than 60% of people over 65 years old have problems with bowel movements. With age, the sensitivity of intestinal wall receptors decreases, and the function of nerve cells that regulate motility is impaired.
- Heredity. The tendency to intestinal atony is inherited. If parents suffer from constipation, the likelihood of problems with bowel movements in children reaches 52%.
- Side effects of drugs. Intestinal motility is inhibited by iron supplements, antidepressants, antispasmodics, and antiulcer drugs.
- Irritable bowel syndrome with a tendency to constipation is a functional disease of the digestive tract associated with a violation of autonomic regulation. Main signs: abdominal pain and stool disorders. Chronic diseases: scleroderma, hypothyroidism, diabetes.
Treatment
How to improve intestinal motility depends on the form and cause of the disease. Dysfunction of motor function requires an integrated approach to therapy. Basic principles of restoring motor function: selection of diet, methods of physical therapy and drug correction. The importance of natural pharmacy products in the form of decoctions of various herbs cannot be ruled out.
Diet therapy
Considering the high importance of food consumed in maintaining or disrupting the functions of the digestive system, personal correction of peristalsis begins in the selection of adequate nutrition that affects the impaired function. Products can speed up contractile impulses or slow them down.
Products that improve intestinal motility:
- fermented milk products (kefir, cottage cheese, sour cream, fermented baked milk, bifidok, yogurt and others);
- high fiber vegetables and greens;
- seafood;
- dried fruits;
- buckwheat, oatmeal and egg;
- compotes and jelly with various berries and fruits, mineral water.
Those that reduce secretion include:
- coffee, tea, cocoa with various pastries;
- puree from various vegetables;
- chocolate;
- rice porrige;
- butter, eggs, meat;
- bird cherry and chokeberry fruits and compotes from them.
Knowing the effect of various foods on the motor function of intestinal smooth muscles, you can influence its work by changing the diet as necessary. For minor disorders, proper nutrition can restore intestinal function, but in old age and situations of long-term impairment this will not be enough.
Movement therapy
How to restore intestinal motility with the help of active movement or special exercises will be suggested by a physical therapy specialist working with the population in the clinic or a doctor observing at the site.
For treatment, you can use special exercises or simple warm-ups in the form of morning exercises or yoga.
A simple set of exercises to improve intestinal motor function:
- immediately after sleep, you can, while in bed (preferably on a hard surface), stretch your arms along the body or put them on your stomach, draw in and protrude your abdominal muscles, you can breathe;
- bend your legs at the knees and “roll the falcon on the floor.” It looks like another pressing of the tailbone and lower back to the floor;
- being in the same position, raise and lower the pelvis;
- bike;
- lifting straight legs alternately with weak physical fitness and both with strong;
- pulling the knees to the chest alternately and together (can be performed from a lying or standing position);
- complete the complex by simply walking in place, preferably to rhythmic music.
Article on the topic: Causes and treatment of vomiting in children without fever
Any set of exercises can be used, lying down, sitting, standing, with a ball, with a jump rope, with a gymnastic stick. The main thing is to practice consistently and in a good mood. Any contraction of the abdominal muscles leads to increased bowel function.
Drug therapy
The most effective way to stimulate peristalsis without effort on the part of the patient is to prescribe medications. However, such treatment without lifestyle support has a short-term effect.
Drugs that improve intestinal motility are selected individually based on the diagnosis:
- if there is a significant decrease in motor function, the doctor may prescribe Proserin or Vasopressin;
- for constipation, choose herbal, salt, oil or synthetic laxatives;
- in case of intestinal dysfunction due to prolonged stress, antidepressants and drugs that affect the central nervous system are prescribed: antipsychotics or tranquilizers;
Important. Any medications should be taken only with the consent of a doctor; the information provided on the site is for informational purposes only and cannot be taken as a guide to action.
ethnoscience
In the “people's first aid kit” there is a remedy to treat any disease, including peristalsis disorders.
- Wheat bran can be used to treat constipation. Which should be steamed with boiling water or consumed raw in a volume of 2 tablespoons and washed down with water. By analogy, in stores you can buy fiber, which is added to any dishes (porridge, soups) or drinks (juices, compote). 1-2 tablespoons per day is enough;
- buckthorn decoction, use instead of tea;
- beet salad with garlic;
- jelly made from oatmeal or wheat sprouts;
- freshly squeezed vegetable juice;
- a mixture of apple, nuts and honey with the addition of lemon (consumed throughout the day in unlimited quantities; in addition to its effect on the gastrointestinal tract, it has immunomodulatory properties).
When using traditional medicine, one should take into account the cause of the pathological process and one’s own tolerance to the various components. If after using any product for more than 3 days there is no improvement, it does not work and requires replacement.
Enhanced motor skills
With high intestinal motility, food remains in the body for less than a day. During this time, it does not have time to be completely digested and absorbed. Diarrhea occurs.
Symptoms
- loose stools from 3 times a day;
- lumps of undigested food in the stool;
- cramping abdominal pain;
- signs of dehydration: thirst, dry mouth, decreased skin elasticity, irregular heartbeat.
Causes
- Errors in nutrition - excess of rough, indigestible food, fats.
- Medications – overdose of laxatives, side effect of antibiotics.
- Inflammation of various parts of the intestine. With enteritis and colitis, the sensitivity of mucosal receptors increases.
- Acute intestinal infections. Toxins from pathogenic bacteria and viruses irritate the intestinal wall.
- Helminthiases. Parasites mechanically affect the intestinal wall and release harmful substances.
- Nervous tension. Stress hormones activate peristalsis, causing diarrhea – “bear disease”.
- Chronic diseases of the liver and pancreas. Digestion of food is disrupted, the volume of intestinal contents increases, and peristalsis reflexively increases.
- Irritable bowel syndrome with a tendency to diarrhea is a form of the disease in which loose stools are observed in more than 25% of bowel movements.
Causes of hyperperistalsis of the stomach and intestines
There are a number of possible conditions that may be accompanied by gastric hyperperistalsis.
There are a number of possible conditions that may be accompanied by gastric hyperperistalsis. Some are more serious than others, especially with excessive vomiting and diarrhea. These conditions can be divided into acute and chronic.
Acute causes (sudden, short-term)
Acute conditions usually begin suddenly and persist for a short period of time until they resolve on their own or after treatment.
- Stomach upset (dyspepsia), often associated with overeating, fatty/spicy foods, unpleasant irritants (unpleasant tastes/smells/sights), alcohol and excessive caffeine consumption, anxiety.
- Infections of the stomach, small and large intestines - food poisoning, gastroenteritis, cholera.
- Over-the-counter and prescription medications, especially NSAIDs and some antibiotics.
- Excessive use of laxatives.
- Oral poisoning or poisoning due to overdose.
- Motion sickness.
- Computer vision syndrome (sometimes).
- Prolonged hunger, strict diet/fasting.
- Strenuous exercise (sometimes), especially ab workouts.
- Pregnancy, especially in the first trimester when morning sickness occurs.
- An attack of gallstone disease, when the pain is not in the stomach or intestines, but adjacent to it.
Chronic causes (long term)
Chronic conditions last much longer, from about 3 months. Some for life. It usually develops gradually, compared to the sudden onset of acute conditions. However, there can be acute flare-ups with many chronic conditions where symptoms are severe and begin suddenly. These outbreaks are short-lived.
- Irritable bowel syndrome (IBS), in which the bowel tends to be overactive (diarrhea-predominant type).
- Inflammatory bowel disease (IBD), especially during flare-ups.
- Lactose intolerance (milk intolerance), when symptoms appear after consuming milk/dairy products. Similar symptoms may occur with intolerance to other foods or malabsorption.
- Celiac disease, which is an autoimmune reaction to gluten (wheat protein).
- Diseases of the pancreas and/or gall bladder, in which the breakdown of food may be impaired.
- Adhesions, which are clumps of scar tissue that some people develop after abdominal surgery.
- Premenstrual syndrome (PMS), which occurs monthly and in which nausea/vomiting is a prominent symptom.
- Obstruction of the gastrointestinal tract, especially around the gastric outlet or in the lower intestine.