FGDS of the stomach is, in official medical language, gastroscopy. This term is from the Greek γαστήρ - which means stomach and σκοπέω - which means I observe, look.
Let's imagine that a patient has a stomach problem. Diagnosing the problem of an internal organ is possible only with the help of tests. But this is an indirect diagnosis. But seeing and taking a piece of tissue from the source of the disease for analysis is more accurate.
A special instrument, a gastroscope, helps with this. In its modern form, a gastroscope is a flexible tube with a fiber-optic system inside, which allows you to visually examine the gastric mucosa from the inside.
The FGDS method allows you to examine not only the stomach. It is also possible to examine the esophagus and duodenum. A modern gastroscope (fibrogastroscope) is also equipped with an instrument for taking material for biopsy .
FGDS of the stomach - what is it
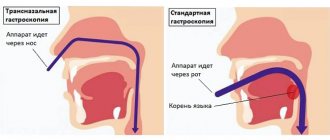
FGDS of the stomach is a diagnostic method that allows you to examine the mucous membranes lining the stomach and duodenum using an endoscopic device - a gastroscope (the device is inserted into the stomach through the mouth).
The EGD procedure of the stomach is a type of gastroscopy. The entire complex of gastroscopy is divided into:
- FGS (conventional gastroscopy and fibrogastroscopy) – during this examination only the stomach is examined;
- VEGDS (videoesophagogastroduodenoscopy) – using a video gastroscope, the mucous membrane of the esophagus, stomach and duodenum is examined;
- EGDS (esophagogastroduodenoscopy procedure) - the EGDS technique involves examining the mucous membrane lining the esophagus, stomach and duodenum using a gastroscope (a flexible fiber-optic system).
For reference. All gastroscopy techniques are similar to each other, the fundamental difference is only in the scope of the study (stomach, stomach and duodenum, all parts of the gastrointestinal tract).
Why is fibrogastroduodenoscopy performed?
FGDS of the stomach is performed using a flexible probe with a built-in video camera. Examination of the gastric mucosa using FGDS allows us to identify even minimal changes affecting only the superficial layers of the mucosa.
When displaying an image on a screen, it can be enlarged, so the doctor can identify pathological lesions ranging in size from several millimeters.
Also, when performing FGDS of the stomach and duodenum, tissue can be taken ( stomach biopsy ) for further research using histological, cytological and immunochemical methods.
For reference. If necessary, during an FGDS, the doctor can remove small polyps or stop gastrointestinal bleeding.
The advantage of FGDS over other diagnostic techniques is:
- high degree of information content and security;
- the procedure is well tolerated and painless (modern endoscopic tubes are significantly different from the old thick hoses previously used for gastroduodenoscopy);
- the possibility of taking biopsy material, portions of gastric juice, bile or duodenal contents during the procedure;
- the ability to assess the degree of gastroesophageal reflux (with reflux, the gastric fluid is thrown into the esophagus);
- the ability to promptly identify various tumors, erosive and ulcerative damage to the mucous membrane, polyps, and find the cause of bleeding;
- the possibility of stopping bleeding and removing small polyps during FGDS.
Diagnostic capabilities of FGDS
In the process of deciphering the results of fibrogastroscopy, the doctor can evaluate in detail the functional and structural features of the organs being examined.
So, during diagnosis the following is determined:
- patency of the stomach, esophagus and duodenum;
- the presence of strictures (stenoses, narrowings), scars;
- the consistency of the cardiac sphincter separating the esophagus from the stomach;
- structural changes in the mucosa (inflammation, ulcers, erosion, atrophy, hypertrophy, metaplasia, areas of atypical epithelium);
- the presence of esophagogastric and duodenogastric reflux;
- hernial protrusions of the esophageal opening of the diaphragm;
- diverticulosis - protrusion of the muscular wall of organs;
- neoplasms of various types (polyps, papillomas, tumors);
- stages of gastritis, ulcers and others.
All these diagnostic capabilities of FGS allow us to consider the procedure indispensable in gastroenterology, surgery, oncology, and other branches of medicine related to the treatment of the gastrointestinal tract.
Therefore, when prescribing it, you should never refuse, but it is better to read reviews about the examination in order to prepare yourself mentally for visiting the diagnostic room.
Fibrogastroduodenoscopy: what is it?
FGDS (endoscopy, gastroscopy) is considered a classic procedure in medicine, carried out to detect and also study diseases of the stomach and esophagus.
Prescribed by a specialist for both diagnostic and therapeutic purposes.
The essence of the method is for the patient to swallow a special diagnostic device - a gastroduodenoscope (endoscope) . It is in most cases presented in the form of a flexible fiber optical tube. It is based on a bundle of glass threads (rod) and a head with a built-in lens or video camera.
When the device is inserted into the esophagus, a thorough examination (including photo and video recording) of the mucous membranes of the gastrointestinal tract is carried out, revealing not only inflammatory processes, but also erosion, ulcers and even tumors . The procedure also makes it possible to evaluate the effectiveness of the patient’s course of treatment or to identify the cause and source of bleeding and eliminate it.
The procedure is performed by a specialized doctor - endoscopist .
The method is unique in a large number of positive features:
- High information content ;
- Painless;
- Safety for gastric tissue;
- Possibility of performing several diagnostic procedures ;
- Possibility of performing the procedure without hospitalization.
the disadvantages of gastroscopy, perhaps only slight discomfort directly during swallowing of the probe.
Indications and contraindications
The fibrogastroduodenoscopy procedure is prescribed by a gastroenterologist, therapist, surgeon or oncologist if the patient has:
- abdominal pain of unspecified nature;
- vomiting coffee grounds or blood;
- bloody stools;
- frequent belching with a sour smell;
- constant bloating, flatulence;
- discomfort and pain when swallowing;
- polyps;
- suspected tumor of the stomach or duodenum;
- bleeding from the gastrointestinal tract.
FGDS can also be prescribed to take biopsy material from pathological areas in the stomach and duodenum, to collect gastric juice and determine acidity, to assess the effectiveness of therapy, and in the diagnosis of pyloroduodenal organic or functional stenoses.
When you can’t perform FGDS of the stomach
Absolute contraindications to performing FGDS of the stomach include: agonal conditions, acute myocardial infarction and recent stroke, aortic aneurysm, as well as diseases in which it is impossible to insert an endoscope into the stomach (severe burn of the esophagus, severe cicatricial stricture of the esophagus).
Relative contraindications include:
- serious condition of the patient;
- post-stroke and post-infarction conditions;
- transient cerebrovascular accidents;
- the patient has a hypertensive crisis, exacerbation of asthma (bronchial asthma), mental illness, severe blood clotting disorders, severe diseases of the respiratory system, severe cardiovascular pathologies.
Contraindications
Contraindications are absolute and relative. Absolute - if present, the examination cannot be carried out in principle; relative - the procedure is postponed until recovery.
| Absolute | Relative |
|
|
Be sure to read:
Histological examination of intestinal tissue: preparation and implementation
How to prepare for FGDS of the stomach
Preparation for FGDS of the stomach is divided into general and local. The patient is prepared by an endoscopist who will perform FGDS. The doctor who referred the patient for examination (gastroenterologist, surgeon, oncologist) can also provide additional advice.
For reference. Poor preparation can significantly complicate or make it impossible to conduct an FGDS, so it is important to strictly follow all the doctor’s recommendations.
General preparation includes three stages:
- Conducting psychological preparation of the patient. The doctor explains to the patient the goals and objectives of the upcoming study, argues for the need to conduct an FGDS of the stomach, and explains why this study will be more informative than other methods. The doctor also explains how the procedure will be performed. Patients with increased emotional lability may be prescribed mild sedatives, sleeping pills or tranquilizers.
- Detection and correction of blood clotting disorders, diseases of the heart, blood vessels and respiratory organs. This stage is especially important, since diseases such as angina pectoris, asthma, arrhythmia, severe respiratory failure, heart failure, and arterial hypertension require special drug correction several days before the study.
- Identification of diseases that may affect the choice of drugs used in preparation for EGD of the stomach. This stage includes identifying individual intolerance to drugs used in endoscopic examinations (intolerance to some local anesthetics), the presence of glaucoma (atropine is contraindicated in such patients), gallstones (salt laxatives are contraindicated in patients). In women, it is also necessary to exclude pregnancy, since most drugs are contraindicated for pregnant women.
How to do an FGDS of the stomach
The entire procedure for FGDS of the stomach is performed in a specialized endoscopic room. FGDS is performed by an endoscopist.
Patients wearing glasses or dentures will need to remove them before the procedure. Large earrings and chains are also removed from the neck.
After local anesthesia with lidocaine or dicaine, you need to wait five minutes until a feeling of numbness appears. Then the patient is placed on his left side and given a special mouthpiece (a plastic ring that acts as a mouthpiece). The mouthpiece must be held with your teeth and lips.
The endoscopic tube is inserted through the mouthpiece. During insertion of the endoscope, it is recommended to relax your throat as much as possible and breathe slowly deeply.
When the endoscope is inserted to the root of the tongue, the doctor asks the patient to swallow the tube. Free movement of the hose and absence of coughing indicate that the endoscope is in the esophagus. There is a slight resistance as the tube moves into the stomach.
After inserting the endoscope into the stomach, the doctor examines its mucous membrane on the monitor. If necessary, the study may be recorded.
If a pathological focus is identified, the doctor can perform a biopsy (take tissue for further research). Also, according to indications, chromoscopy, removal of polypous formations, stopping bleeding or administering medications can be performed.
If additional examination of the duodenum is necessary, after examining the stomach, a probe is inserted into the intestine. The inspection results are also displayed on the screen and, if necessary, recorded.
How long does FGS last?
The duration of the procedure refers to the time from the moment the endoscope is inserted until it is removed. FGS lasts from 5 to 15 minutes (FGDS will take a few minutes longer).
If complex medical procedures are additionally performed, then the endoscopy time can last, on average, up to 30–40 minutes.
For reference. After the usual FGDS, the patient is recommended to lie down or sit for a while (5-10 minutes). After this, the patient can go home or to his room.
If polyps were removed or a biopsy was performed during FGDS, the time the patient spent in the department will depend on the main diagnosis and the scope of the intervention performed.
Is it painful to have a gastroscopy?
Most patients who have undergone FGDS in the traditional way, if asked to describe their feelings from the procedure, call it unpleasant.
To reduce the severity of these sensations, a local anesthetic is used, which is applied to the back wall of the oropharynx. However, it does not always save the patient from discomfort.
The most common complaints from patients:
- nausea;
- a feeling of discomfort in the neck, behind the sternum or in the abdomen;
- increased salivation;
- belching;
- feeling of lack of air;
- panic attacks;
- aching or cutting pain in the neck or abdomen.
For reference. Oddly enough, pain syndrome is relatively rare. It is possible in the presence of acute pathology (for example, exacerbation of peptic ulcer disease in young patients), complications (wall perforation) or careless examination, however, swallowing the intestine to check the stomach is unpleasant.
The main thing is to behave correctly during the procedure and listen to the doctor’s recommendations.
Choosing the right doctor
Choosing a qualified doctor with a friendly approach to his patients can significantly reduce anxiety before the procedure, as well as reduce the severity and frequency of side effects.
A good approach from a specialist relieves anxiety and helps the patient relax. This allows the procedure to be carried out without unnecessary trauma (for example, scratching the throat), since the probe advances more easily.
In clinical practice, there are situations when, due to low professionalism, the doctor applies the wrong or insufficient anesthetic. Also, some medical professionals do not explain the essence of the procedure, possible risks, and nuances of patient behavior.
Important. The doctor must carefully explain the nuances of preparing for the study, as well as select the most appropriate method of performing the procedure (nasal insertion of a probe, sedation or anesthesia) for a particular patient.
Breathing feature
Before starting the procedure, the doctor must explain to the patient how to breathe correctly during FGDS. Breathing should be through the nose, deep and smooth. In this case (despite popular belief) there is no need to swallow while moving the endoscope through the oropharynx and larynx.
Preparation: some important tips
You should prepare very seriously for gastroscopy, as for any other research method, since the comfort and effectiveness of the procedure depends on this. The following is a reminder for the patient that will help simplify the process of fibrogastroduodenoscopy:
You should not eat at least 8 hours before the procedure, as your stomach must be empty. If you neglect this rule, doing the test may be pointless because either the results will end up being inaccurate or the procedure will cause vomiting.
- On the day of FGDS, you must be careful about taking medications (it is advisable to consult with a gastroenterologist first).
- Some time before gastroscopy, you need to give up cigarettes and alcohol , as they irritate the stomach and create a feeling of nausea.
- Do not use perfume before the procedure .
- It is important to warn the specialist before the procedure about all concomitant diseases and medications taken (this point is especially important for allergy sufferers, chronically ill patients, and pregnant women).
- It is necessary to come to the procedure in loose clothing and with the appropriate attitude (in a calm, relaxed state) .
- You can drink water an hour before the procedure . No more than half a glass of water.
- You can brush your teeth before the examination . But you should refrain from chewing gum.
If acidity is to be determined, then it is necessary to stop taking medications that affect it . We are talking about several types of drugs:
- Antisecretory (lowering pH). These include proton pump inhibitors (Omeprazole, Lanzoprazole), anticholinergics, bismuth preparations , etc.
- Stimulating/replacing pH . Pentagastrin, Lemontar, preparations based on plantain, etc.
- Antacids . Neutralizers that maintain normal acidity or reduce it (Rennie, Tams, Maalox, Gastrocid, Gaviscon, etc.).
To make the examination comfortable and easy, it is important to follow a special diet for several days before the examination, while temporarily changing your rhythm of life. So, in 3-4 days you should exclude from the diet :
- Liquid food;
- Fatty, spicy, salty foods;
- Pickles;
- Some drinks (sparkling water, juices, alcohol);
- Nuts, seeds;
- Vegetables/fruits with a high content of acids (tomatoes, peaches, plums, apples, etc.);
- Legumes;
- Baking;
- Dairy products.
As dietary foods, you can eat baked vegetables, low-fat fish, boiled chicken, eggs (except fried), herbal teas (without sugar), water . In the evening the day before the test, have a light dinner at least 2 hours before bedtime .
Please note: If you follow a diet before gastroscopy, you need to eat 5-6 times a day (little by little). If discomfort occurs in the stomach even while taking certain dietary foods, you should also avoid them.
It is worth noting that endoscopy is completely safe for pregnant and lactating women . If gastroscopy is performed on a child, it is very important to first prepare him for diagnosis by describing in detail the essence of the procedure, as well as practicing measured breathing through his nose with his mouth open.
It is equally important for mothers to behave correctly during the procedure : the voice should be calm and quiet, since babies always feel any changes in their mother’s mood.
Complications after the procedure
For reference. FGDS of the stomach is a safe procedure. Complications after the procedure are extremely rare and do not pose a threat to the patient’s health or life.
The main complications are sore throat and discomfort after removing the endoscope. There may also be discomfort in the abdomen due to the entry of air. After belching air, the discomfort disappears.
When a biopsy is taken, slight swelling and discomfort in the epigastric region may be observed for several days.
More serious complications are rare. Minor bleeding may be due to damage to the esophageal mucosa by the endoscope.
Perforation of the wall of a hollow organ (esophagus, stomach, duodenum) can be observed in patients with large ulcers of the mucous membrane and gastrointestinal tract.
Bleeding may also occur after endoscopic removal of polyps. Most often, bleeding stops on its own, or after drug or endoscopic hemostasis.
Preparation for the procedure
To have a successful examination, you need to prepare properly. Preparation contains several mandatory points.
Is a diet required before the procedure?
A long-term diet is not required, since any food eaten leaves the stomach (if there are no contractions or tumors) within 12 hours.
However, 2 days before the study you should not eat irritating foods that can change the gastroscopic picture. These products include:
- spicy pepper dishes;
- alcohol;
- chocolate and products made from it;
- all types of seeds and nuts;
- fresh vegetables.
12 hours before the appointed time you need to stop eating any food. The last meal before the break should consist of easily digestible dishes - chicken with porridge, fish with stewed vegetables, and the like. Food is prepared with a minimum amount of oil and without spicy seasonings. The serving size is small, about the size of a dessert plate. Too much food may not have time to move to the lower parts of the digestive system, and the examination will have to be repeated.
Can I drink water before the procedure?
Immediately before the examination, you should not drink anything; excess fluid in the stomach will not allow it to be thoroughly examined. The last intake of water or sweet tea is allowed 2 hours before the start of the procedure.
Is it possible to brush your teeth before FGDS?
Can. A small amount of gastric mucus, which is released in response to brushing your teeth, manages to be absorbed on the way to the hospital.
Is it possible to smoke before FGDS?
It is better not to smoke, because it is known from practice that smoking increases discomfort during the examination.
Be sure to read: In detail about intestinal colonoscopy: preparation and procedure
Other preparation tips
If the patient systematically takes medications, then on the eve of the procedure only those that dissolve are allowed. Tablets and capsules should not be taken. Injections are allowed, but if possible it is better to postpone them for several hours. Emergency injections (insulin and the like) are given on time.
If the test is scheduled for 11 am or later, at home you need to drink one glass of clean water or weak tea, which can be sweetened.
Alternative research methods
For reference. Only capsule endoscopy can be considered a direct analogue of FGDS, but this method is very expensive, and with capsule endoscopy it is not possible to take material for research.
This endoscopic research method involves the advancement of a special capsule that contains a microvideo camera through the gastrointestinal tract. The patient is asked to swallow it, after which an image appears on the monitor.
Alternative methods also include:
- Ultrasound of the abdominal organs;
- X-ray with contrast;
- tomography.
Contrast x-rays are the most popular. The risk of misdiagnosis is about 15%.
Similar articles:
- What is excretory urography of the kidneys, how is it performed? Excretory urography is a research method. Let's look at the name of the method so that...
- What does a gastric biopsy show, preparation and conduct of the procedure? A gastric biopsy is a diagnostic procedure for taking a sample of mucosal tissue...
- What is Diaskintest, how is it carried out and what does Diaskintest show? This is one of the methods for diagnosing tuberculosis. Tuberculin diagnostics is constantly...
- Stool analysis for coprogram: what is it? Before undergoing a coprogram, you should know what it is and how...