Autoimmune pancreatitis
Autoimmune pancreatitis
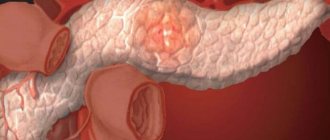
is a rare systemic disease of the pancreas and other organs caused by damage to connective tissue by immunoglobulins G4.
Manifested by abdominal pain, icteric syndrome, dyspepsia, stool changes and signs of malnutrition. Diagnosed using ultrasound, MRI of the pancreatic gland, coprogram, determination of the level of immunoglobulins and histological analysis. Corticosteroids and monoclonal antibodies are used for therapy. If conservative treatment is ineffective, drainage, stenting, and ostomy of the pancreatic and bile ducts are performed.
Causes of autoimmune pancreatitis
The exact causes of autoimmune pancreatic disease are unknown. Provoking factors include:
- rheumatoid arthritis;
- inflammatory diseases of the digestive system;
- Sjögren's syndrome (autoimmune connective tissue disease);
- the presence of chronic foci of infection.
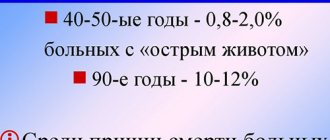
General information
Although autoimmune pancreatitis is considered a rare disease, its share in the structure of chronic inflammation of the pancreas reaches 4-6%. The prevalence of the disease does not exceed 0.0008%. The pathology was first described by the French clinician G. Sarles in 1961. The disease was recognized as a separate nosological entity in 2001 after the development of the etiological classification of pancreatitis TIGAR-O. Autoimmune damage to the pancreatic gland in men is detected 2-5 times more often than in women. Up to 85% of patients become ill after 50 years of age. The disease is often combined with rheumatoid arthritis, retroperitoneal fibrosis, sclerosing cholangitis and other autoimmune processes.
Causes
The etiology of autoimmune pancreatitis has not been established. Typically, the disease is diagnosed by exclusion when G4 type immunoglobulins are detected and there are no other possible causes of pancreatic damage. Experts in the field of clinical gastroenterology admit the leading role of hereditary burden; in the course of medical genetic studies, an association of the autoimmune process with the HLA serotypes DRβ1-0405, DQβ1-0401, DQβ1-57 was established. A serum protein weighing 13.1 kDa, which is considered a specific antigen, was isolated from the blood of patients.
Carbonic anhydrase, present in the tissues of the digestive organs, the bronchial tree and distal renal tubules, lactoferrin, detected in pancreatic acini, bronchial and gastric glands, components of cell nuclei and smooth muscle fibers, pancreatic inhibitor of trypsinogen and trypsin are considered as probable autoantigens. Cross-sensitization with infectious agents cannot be ruled out—molecular mimicry was discovered between antibodies to proteins of the causative agent of Helicobacter pylori and plasminogen-binding protein.
Pathogenesis
The trigger for changes in the pancreatic gland and other sensitive organs is the connection of serum Ig G4 with autoantigens of acinar cells, normal epithelial cells of the pancreatic, bile, salivary ducts, etc. Antigenic damage is accompanied by a violation of apoptosis of cellular elements of the immune system. The key link in the pathogenesis of autoimmune pancreatitis is considered to be the accumulation of persistent activated T- and B-lymphocytes, neutrophils and eosinophils in the connective tissue, provoking fibrous-sclerotic processes.
Cytological examination reveals signs of fibrosis and sclerosis in the pancreatic stroma in the absence of pseudocysts and calculi. Due to lymphoplasmacytic, neutrophilic and eosinophilic infiltration, the walls of the ducts are compacted, narrowed, and fragmented during a long course of the autoimmune process. The spread of inflammatory infiltration to the lobules of the pancreas leads to the loss of the lobular structure of the organ and is often combined with phlebitis. As with other types of chronic pancreatitis, calcification of the parenchyma and stroma is possible.
Classification
When systematizing the forms of autoimmune pancreatitis, the prevalence of the fibrosclerotic process, the presence of concomitant lesions of other organs, and the morphological features of inflammation are taken into account. In the focal variant of the disease, individual areas of the pancreatic parenchyma are damaged, mainly the head of the organ. Usually at least 1/3 of the gland is affected (segmental form of pancreatitis). The diffuse form of pathology is characterized by involvement of the entire organ.
In the absence of other autoimmune diseases, pancreatitis is called isolated. In the case of systemic damage to several organs, they speak of syndromic autoimmune pancreatic inflammation. Taking into account the histological picture, two main variants of the disease are distinguished, each of which has characteristic clinical features:
- Lymphoplasmacytic sclerosing form of pancreatitis
. Infiltration of immunoglobulin-producing cells, pronounced fibrosis of the organ stroma and obliterating phlebitis predominate. Combined with IgG4-associated autoimmune pathology. It is characterized by an often relapsing course with progression of sclerotic changes. - Ductal-concentric idiopathic pancreatitis
. Morphologically it manifests itself as neutrophilic infiltration with cellular accumulations resembling microabscesses. Phlebitis and fibrosis are less pronounced. Serum IgG4 levels are usually normal. In 30% of cases it is associated with ulcerative colitis. It occurs without relapse. It occurs 3.5-4 times less often.
Symptoms of autoimmune pancreatitis
The clinical picture of the disease differs from typical inflammation of the pancreas. With the autoimmune variant of organ damage, the pain is less intense, dull, and is not associated with errors in the diet. Pain syndrome develops in only half of patients. Another important symptom of autoimmune pancreatitis is obstructive jaundice, which occurs on average in 60-80% of patients and is manifested by icteric discoloration of the skin and sclera, itchy skin, and discoloration of stool.
Autoimmune pancreatic pathology is often accompanied by dyspeptic disorders: nausea, changes in stool character (profuse, fetid, grayish stool), and bloating. As the disease progresses, malabsorption and nutritional deficiency occur, which is manifested by a decrease in the patient's body weight, protein-free edema of the face and lower extremities. In the later stages of pancreatitis, constant thirst and polyuria develop (symptoms of impaired glucose metabolism).
Autoimmune pancreatitis: symptoms, treatment and diagnosis
Autoimmune pancreatitis is a pathology of the pancreas caused by damage to the organ parenchyma by autoantibodies. In addition to the pancreas itself, other organs of the digestive system may also be involved in the pathological process. Autoimmune pancreatitis is a type of chronic pancreatitis.
Etiology of the lesion
There are currently no exact reasons for the development of the disease. It is known that the damaging factor is autoantibodies that aggressively act on pancreatic tissue. The reason for their activation remains unknown. Autoimmune inflammation quickly leads to tissue sclerosis and organ dysfunction.
Features of the clinical picture
The disease tends to be latent. In most cases, it does not manifest itself for a long time and can only be detected when complications develop.
Main symptoms of the disease.
- Pain syndrome. It is observed in 50% of patients. The pain is localized in the upper abdomen and may be girdling in nature. Patients describe it as a monotonous, nagging or aching pain, lasting from several minutes to several hours. An attack of pain can be triggered by eating fatty or fried foods or overeating.
- Jaundice discoloration of the skin and mucous membranes. It is observed when there is an obstruction to the exit of bile from the bile ducts into the duodenum. In this case, the patient may notice yellowing of the skin and sclera, lightening of the stool, darkening of the urine. With pronounced jaundice, skin itching occurs. It occurs due to irritation of the nerve endings of the skin by bilirubin.
- Phenomena of dyspepsia. Each patient manifests differently. This may be an unpleasant sensation in the mouth - dryness, bitterness, unpleasant odor. Belching after eating, gas formation and bloating, upset bowel movements.
- Pathological weight loss - develops as a result of impaired digestion of food.
- Asthenic syndrome. It manifests itself in the form of a decrease in the general resistance of the body, increased fatigue, irritability, and weakness.
- When accompanying organs are damaged, corresponding symptoms develop.
Principles of classification of autoimmune pancreatitis
The disease is classified according to several characteristics.
According to histological examination, pancreatitis can be:
- Lymphoplasmacytic sclerosing pancreatitis. The lesion in this case diffusely covers the entire parenchyma of the pancreas. Histologically, lymphocytic contamination of the tissue is observed.
- Idiopathic ductal pancreatitis with granulocytic lesions. This variant is characterized by a concentration of pathological foci around the pancreatic ducts. Histologically, granulocytic tissue is detected.
Based on the presence of concomitant autoimmune pathologies.
- An isolated variant of the disease is pancreatitis, in which case the patient has the only autoimmune disease.
- Autoimmune syndrome - in this case there is another pathology associated with the activity of autoantibodies.
Damage to related organs.
- Foci of sclerotic tissue appear in the lungs. Respiratory function is impaired due to a decrease in the working surface of the lungs, and shortness of breath develops.
- Kidneys. Tubular reabsorption is disrupted, and renal failure develops.
- Liver. Tissue sclerosis is also observed; the patient may complain of heaviness and discomfort in the right hypochondrium.
- Sialadenitis. There is inflammation of the salivary glands, which is manifested by pain and difficulty swallowing.
Diagnostic methods
To confirm the diagnosis, a full comprehensive examination is necessary. The diagnosis is based on clinical data, laboratory and instrumental studies.
- To confirm the presence of an autoimmune process, the level of IgG4 in the blood serum is determined - an increase of several tens of times is observed.
- General clinical tests are prescribed - blood, urine, biochemical blood test.
- Coprology is needed to assess the functional state of the pancreas.
- To exclude an oncological process in the pancreas, tumor markers are determined.
- Ultrasound examination of an organ - the size, condition of the organ parenchyma, and the preservation of functionally active tissue are assessed.
- CT scan. Determines the presence of foci of fibrosis in the tissue around the ducts.
- Biopsy and histological examination. The method is quite informative if a piece of tissue is taken from the site of the lesion. The type of pancreatitis can be determined.
Treatment options
It is impossible to completely cure an autoimmune disease. Therefore, treatment is mainly aimed at relieving symptoms and slowing down the progression of the process.
First of all, constant adherence to the diet is necessary to prevent the development of pain.
- Canned food, smoked foods, fatty foods, fried foods, and spices are excluded from the diet.
- It is recommended to consume lean meat, plant and dairy foods.
To suppress the activity of autoantibodies, immunosuppressive therapy is prescribed - cytostatics, glucocorticoids.
To reduce the manifestations of pain, antispasmodics are used.
To maintain the functional state of the pancreas and improve digestion, enzyme preparations are prescribed.
With the development of difficulty in the outflow of bile and the appearance of jaundice, drugs based on ursodeoxycholic acid are used.
If the gastric mucosa is damaged—the development of erosive gastritis—proton pump inhibitors and antacids are prescribed.
There is surgical treatment used for pancreatic duct stenosis.
Therapy is considered adequate if, against its background, the pain syndrome decreases, manifestations of jaundice disappear, and laboratory parameters normalize.
Forecast
The disease is chronic and stays with a person for life. Adverse outcomes are quite rare. The most serious complication that can develop is diabetes.
Source: https://1PanKreatit.ru/vidy/autoimmunnyj-pankcreatit.html
Complications
In most patients, autoimmune pancreatitis occurs with the involvement of other organs and tissues in the pathological process. Most often, the disease spreads to the biliary system with the development of sclerosing cholangitis and acalculous cholecystitis. The connection of these nosological forms with pancreatitis is indicated by typical lymphohistiocytic infiltration of the walls of the biliary tract and a good response to hormonal therapy. Sometimes the liver is affected, causing pseudotumor or cirrhosis.
A common complication of pancreatic autoimmune inflammation is diabetes mellitus, which occurs as a result of gradual necrosis of the cells of the islets of Langerhans, accompanied by a sharp decrease in insulin production. More rare consequences of the disease are immunocomplex damage to the renal parenchyma such as tubulointerstitial nephritis, interstitial pneumonia. The circulation of IgG antibodies in the blood leads to sclerosis of the tissues of the salivary glands.
Diagnostics
Making a correct diagnosis is difficult, which is explained by the rare occurrence of the pathology and the diversity of its clinical manifestations. In most cases, the diagnostic search for autoimmune pancreatitis is aimed at excluding other forms of pancreatic inflammation. The most informative research methods are:
- Stool examination
. The coprogram identifies typical signs of malabsorption and maldigestion: a large number of undigested food particles and muscle fibers, an increased content of fatty acids. Additionally, a fecal elastase test is performed, which confirms the presence of pancreatitis. - Serological reactions
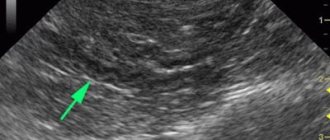
. A blood test for specific antibodies reveals hypergammaglobulinemia - an increase in the level of IgG and IgG4 several times, which is a pathognomonic symptom of autoimmune lesion type 1. Antimitochondrial and antinuclear antibodies are also detected. - Sonography
. A standard study confirms the disease only in an advanced stage. Endoscopic ultrasound of the pancreas visualizes focal or diffuse tissue compaction, alternating areas of dilation and narrowing of the pancreatic duct (“sausage-shaped” pancreas). - Tomography
. The autoimmune type of pancreatitis is characterized by a diffuse increase in organ size or the presence of limited tumor formation, deformation of the contours of the ducts. MRI of the pancreas is also used to monitor the effectiveness of glucocorticosteroid therapy. - Histological examination
. Cytological analysis is the “gold standard” in the diagnosis of autoimmune inflammation. A morphological examination reveals lymphoplasmacytic infiltration around the pancreatic ducts, areas of parenchyma destruction, and involvement of the vascular network in the process.
Treatment
An autoimmune disease is almost impossible to completely cure. However, it is possible to stop the progression of pancreatitis and eliminate some complications of inflammation in other organs. To do this, a complex effect is used, including diet and one of two methods of primary therapy - medication or surgery.
As a rule, for autoimmune pancreatitis, diet number 5 is prescribed. It involves eating five or six meals a day in small portions, as well as excluding foods rich in coarse fiber from the diet. In addition, during the diet you should not eat fatty, smoked, salty foods, as well as sweets, confectionery, and baked goods.
The maximum dosage of table salt per day is three grams. Along with this, with concomitant diabetes mellitus, restrictions are imposed on simple carbohydrates.
Drug treatment includes the use of the following groups of drugs:
- Glucocordicosteroids. Treatment with medication usually lasts several weeks.
- Immunosuppressants (medicines that suppress the activity of the immune system). They are used when hormonal therapy shows insufficient effectiveness.
- Enzymes (Pancreatin, Festal, Mezim). Necessary to improve digestion and relieve excess stress on the gland.
- Antispasmodics and painkillers (No-Shpa, Drotaverine). Relieve and prevent pain.
- Agents that block the production of digestive juices (Almagel, Maalox). Promotes restoration of stomach and gland tissues.
Insulin is also used to treat diabetes. If all treatment recommendations are followed, the use of the hormone is subsequently discontinued. In this case, the prognosis of the entire therapy is often positive.
Surgery shows good results if conservative therapy is useless and the bile ducts are significantly narrowed. In this case, one of two methods is used:
- decompression (restores the lumen of the gallbladder ducts);
- stenting (a specialized stent is inserted into the ducts to level the lumen).
As a rule, with sufficient and timely therapy, the use of medications and a therapeutic diet is sufficient. Surgery may be necessary if complications are at an advanced stage.
Treatment of autoimmune pancreatitis
Since spontaneous recovery with complete restoration of exocrine and endocrine pancreatic functions is possible in some patients, drug therapy is carried out only if there are appropriate indications. In asymptomatic cases, the prescription of medications is justified in the case of persistent formation of the pancreatic gland, persistent changes in liver parameters in combination with signs of sclerosing cholangitis. Recommended treatment regimens for autoimmune pancreatitis usually include:
- Glucocorticosteroids
. Steroid hormones are first-line drugs and often provide long-term therapeutic effects within 2-3 weeks. In the absence of obvious fibrosis, the size and structure of the pancreas can be completely restored. Prescribing steroids is effective not only for signs of pancreatitis, but also for autoimmune damage to other organs. - Monoclonal antibodies
. Indicated for resistant disease or the presence of contraindications to steroid therapy. Synthetic immunoglobulins Ig G1-k are used to bind the B-lymphocyte CD antigen. A rapid decrease in the number of B-lymphocytes is accompanied by a drop in Ig G4 levels and the induction of remission of autoimmune pancreatic inflammation.
In symptomatic therapy, taking into account clinical manifestations, pancreatic enzymes, hypoglycemic agents and proton pump blockers are used. To relieve pain, non-steroidal anti-inflammatory drugs and myotropic antispasmodics are recommended. Patients with persistent compression undergo stenting of the main pancreatic duct, percutaneous transhepatic drainage of the bile ducts, and nasobiliary drainage during RPCP. If minimally invasive techniques are unsuccessful, pancreatojejunostomy and cholecystoenterostomy are performed.
Treatment of the disease
It is almost impossible to recover completely when treated for autoimmune pancreatitis. That is why the main methods of therapy are aimed at relieving symptomatic signs and inhibiting the progressive pathological process.
First of all, the recommendations of such specialists as Igor Veniaminovich Mayev (Honored Gastroenterologist and Doctor of Science) and Yuri Aleksandrovich Kucheryavy (Candidate of Medical Sciences) consist of strict adherence to a dietary diet to ensure the prevention of pain and maximum relief from the workload of the pancreas.
Immunosuppressive therapy, consisting of cytostatics and glucocorticoids, is also prescribed. To reduce the pain that manifests itself during periods of exacerbation of the disease, antispasmodic drugs are prescribed.
In case of obstructed outflow of bile and the development of yellowness of the skin and mucous membranes, medications containing ursodeoxycholic acid are used.
If stenosis develops in the cavity of the pancreatic ducts, surgical treatment is prescribed.
Prognosis and prevention
The outcome of the disease depends on the degree of tissue damage and the severity of complications. Although steroid therapy achieves remission in more than 90% of patients, the prognosis of autoimmune pancreatitis is relatively unfavorable; in some patients, an irreversible decrease in the endocrine and exocrine functions of the organ occurs. Due to the insufficiently studied etiopathogenetic mechanism, specific prevention measures have not been developed. To prevent complications, it is important to promptly identify and treat autoimmune diseases of the digestive tract.
source
Symptoms of autoimmune pancreatitis
The main features of autoimmune pancreatitis are the moderate severity of all symptoms and the absence of acute attacks (episodes of sudden deterioration of the patient’s condition). In some cases, there may be no symptoms, and the diagnosis is made only when complications develop.
- Abdominal pain syndrome (a stable set of symptoms): pain or discomfort in the upper abdomen, less often in the lumbar region, occurs in approximately half of patients, and can last for several minutes or hours. The pain intensity is moderate or insignificant. As a rule, pain is provoked by eating spicy, fatty and fried foods.
- Jaundice is a yellow discoloration of the skin, mucous membranes (for example, the oral cavity) and biological fluids (for example, saliva, tear fluid, etc.). Develops as a result of a violation of the flow of bile into the duodenum (the initial part of the small intestine) due to narrowing of the pancreatic ducts and bile ducts: stool is lighter than usual;
- urine is darker than usual;
- yellow staining of saliva, tear fluid, plasma (liquid part) of blood, etc.;
- skin itching.
- Dyspeptic manifestations (digestive disorders): loss of appetite;
- nausea and vomiting;
- bloating;
- bitterness and dry mouth in the morning;
- bad breath.
- Violation of the exocrine function of the pancreas (the secretion of enzymes involved in the digestion of food) in most cases has no manifestations and is detected during a special laboratory test.
- Diabetes mellitus (disorder of carbohydrate-sugar metabolism) develops rapidly as a result of deterioration of the endocrine function of the pancreas (production of hormones that regulate carbohydrate metabolism). A feature of diabetes mellitus in autoimmune pancreatitis is its favorable course with possible reverse development (recovery) against the background of full treatment.
- Loss of body weight.
- Asthenic syndrome: decreased performance;
- increased fatigue;
- weakness;
- daytime sleepiness;
- decreased appetite;
- depressed mood.
- Damage to other organs. Lungs. It manifests itself as shortness of breath (rapid breathing), a feeling of lack of air due to the formation of areas of compaction of the lung tissue.
- Kidney. It manifests itself as renal failure (impairment of all kidney functions) and the appearance of protein in the urine (normally this should not be the case).
- Liver (liver pseudotumor) - development of compaction of liver tissue without tumor cells. It is detected by palpation (palpation) or instrumental research methods. May be accompanied by prolonged heaviness in the right hypochondrium, not associated with food intake.
- Salivary glands (sclerosing sialadenitis) - inflammation of the salivary glands with the replacement of normal tissue with scar tissue. Manifestations: dry mouth;
- pain in the salivary glands;
- difficulty swallowing, breathing and speaking due to dry mouth.
symptoms
Autoimmune pancreatitis (AIP) is difficult to diagnose. Often this does not cause any symptoms. When this occurs, its symptoms and symptoms are similar to those of pancreatic cancer.
Symptoms of pancreatic cancer may include:
- Dark urine
- Pale stool or stool that floats in the toilet
- Yellow skin and eyes (jaundice)
- Pain in the upper abdomen or mid back
- Nausea and vomiting
- Weakness or extreme fatigue
- Loss of appetite or feeling full
- Weight loss for an unknown reason
The most common sign of autoimmune pancreatitis, present in about 80 percent of people, is painless jaundice caused by blocked bile ducts. AIP can also lead to weight loss. Many people with autoimmune pancreatitis have masses in the pancreas and other organs that may be misdiagnosed as cancer.
Other differences between AIP Type 1 and Type 2:
- In type 1 AIP, the disease can affect other organs in addition to the pancreas. Type 2 AIP affects only the pancreas, although the disease is associated with another autoimmune condition, inflammatory bowel disease.
- Type 1 AIP responds quickly to steroid treatment.
- Type 1 AIP is likely to recur if treatment is stopped.
When to see a doctor
Autoimmune pancreatitis often does not cause any symptoms. However, consult your doctor if you experience unexplained weight loss, abdominal pain, jaundice, or other signs and symptoms that concern you.
Forms
Based on the histological picture (changes in the structure of the pancreas identified under a microscope), two types of autoimmune pancreatitis are distinguished:
- Type 1 - lymphoplasmacytic sclerosing pancreatitis;
- Type 2 - idiopathic ductal-concentric pancreatitis with granulocytic epithelial lesions.
The differences between these options are only histological (that is, they are revealed during histological examination - studying pieces of an organ under a microscope).
Depending on the presence of other autoimmune diseases (which develop when various organs are damaged by the forces of one’s own immunity - the body’s defense system), two types of autoimmune pancreatitis are distinguished:
- isolated autoimmune pancreatitis – develops in a patient who does not have other autoimmune diseases;
- autoimmune pancreatitis syndrome - develops in a patient who has other autoimmune diseases.
Depending on the localization (location) of the lesion, the following are distinguished:
- diffuse form (damage to the entire pancreas);
- focal form (damage to individual areas of the pancreas, most often its head, during instrumental examination resembles cancer (malignant tumor) of the pancreas).
Diagnostics
- Analysis of the medical history and complaints (when (how long ago) pain in the upper abdomen, jaundice (the appearance of a yellow color of the skin, mucous membranes (for example, the oral cavity), biological fluids (for example, saliva, tear fluid, etc.)), decreased body weight, increased volume of feces and other symptoms, with which the patient associates their occurrence).
- Life history analysis. Does the patient have any chronic diseases, are there any hereditary diseases (passed from parents to children), does the patient have bad habits, has he taken any medications for a long time, have he had tumors, has he been in contact with toxic substances ( toxic) substances.
- Physical examination. Reduced or normal body weight is determined, yellowness of the skin and mucous membranes is possible. When palpating (feeling) the abdomen, pain in the upper sections is possible. By percussion (tapping) of the abdomen, the sizes of the liver, spleen, and pancreas are determined.
- Laboratory research methods. A general blood test can reveal an increase in the erythrocyte sedimentation rate - red blood cells (an indicator reflecting the ratio of blood proteins), and less often - an increase in the number of lymphocytes or eosinophils (special types of leukocytes - white blood cells).
- Blood glucose (simple carbohydrate) level. If the intrasecretory function of the pancreas (the production of hormones that regulate carbohydrate metabolism) is impaired, glucose in blood taken on an empty stomach increases.
- Glycosylated hemoglobin (an indicator reflecting the average glucose level in the blood over a long period - up to three months) may increase.
- A lipidogram (the content of fat-like substances in the blood) can reveal an imbalance in the ratio of potentially dangerous and protective types of lipids.
- Blood chemistry. The level of creatinine (a protein breakdown product), uric acid (a breakdown product of substances from the cell nucleus), alkaline phosphatase (ALP), gamma-glutamyl transpeptidase (GGT), alanine aminotransferase (ALAT or ALT), aspartate aminotransferase (AST or AST), bilirubin (bile pigment - a coloring substance, a breakdown product of erythrocytes - red blood cells), electrolytes (potassium, sodium, calcium, magnesium).
- Tumor markers (substances that increase in the blood when a tumor occurs): CA 19-9 and carcinoembryonic antigen are signs of cancer (malignant, that is, a tumor growing with damage to surrounding tissues) of the pancreas.
- A general urinalysis reveals a darker color of the urine than it should normally be; bile pigments (coloring substances secreted by bile) and sometimes proteinuria (protein in the urine) are found in the urine. Also, a general urine test is necessary to monitor the condition of the urinary tract and organs of the genitourinary system.
- The content of immunoglobulin G4 (IgG4 is a special type of protein that increases during autoimmune reactions - damage to one’s own cells by the forces of the immune system - the body’s defense system) in the blood increases more than 2 times.
- Coprogram - stool analysis (undigested fragments of food and fat, coarse dietary fiber can be detected, the level of elastase and chymotrypsin (pancreatic enzymes that break down proteins) may decrease during a biochemical analysis of stool).
- Ultrasound examination (ultrasound) of the abdominal organs allows us to assess the size and structure of the liver, pancreas and spleen, the presence of obstacles to the outflow of bile at various levels in the form of narrowing of the ducts, stones, tumors, etc.
Diagnosis of the disease
A correct and accurate diagnosis can only be made on the basis of a complete examination of the patient’s body, tests and additional diagnostic procedures.
To obtain a complete clinical picture of the development of the disease, the following diagnostic procedures are recommended:
- determination of the concentration of immunoglobulin IgG4 in the blood serum; with pathology, it can increase 10 times,
- general clinical tests are prescribed: blood for biochemistry, general analysis of urine and feces,
- scatological examination of stool,
- determination of tumor markers,
- to determine the degree of damage and the condition of the parenchymal organ, computed tomography and ultrasound are prescribed,
- and also one cannot do without biopsy and histology.
After receiving a complete clinical picture, the doctor makes an accurate diagnosis, determines the prognosis for the development of the disease and develops the most effective and safe treatment regimen.
It is worth noting that a small child can also develop a similar disease, although this is quite rare. However, when it occurs in a baby, it is manifested by excessive yellowness of the skin, which cannot be ignored by doctors.
Ultrasound diagnosis
Ultrasound diagnostics allows you to accurately measure the external parameters of the affected organ, assess the structural features and degree of progression of pathology in the cavity of the pancreas, liver and spleen.
Using this research method, the causes that contribute to the disruption of bile outflow are identified, as well as the presence of tumor-like neoplasms and stones in the gland cavity.
Determination of IgG4 immunoglobulin concentration
When conducting a clinical study of blood tests, special attention is paid to the concentration of immunoglobulin IgG4. In a healthy person, its concentration does not reach 5% of the total amount of blood serum. With a sharp increase in its concentration, we can safely talk about the development of a pathological disorder in the human body, accompanied by the process of infiltration of organs secreting this immunoglobulin.
In other words, there is an active development of the inflammatory process in tissue structures with the formation of fibrosis and scarring.
In patients with the development of autoimmune pancreatitis in more than 88% of cases, an increased level of immunoglobulin is observed, 5 and even 10 times higher than normal.
Treatment of autoimmune pancreatitis
In rare cases, self-healing occurs (that is, without the use of medications).
Basics of treatment of autoimmune pancreatitis.
- Diet therapy. Diet No. 5 - eating 5-6 times a day, excluding spicy, fatty, fried, smoked, coarse (rich in fiber - difficult to digest part of plants) foods from the diet, limiting table salt to 3 grams per day. Food should contain sufficient amounts of vitamins, calcium salts and phosphorus (for example, fish, boiled meat, vegetable broth soups, moderate-fat dairy products, etc.). The purpose of this diet is to reduce the load on the pancreas.
- With the development of diabetes mellitus (carbohydrate-sugar metabolism disorders) as a manifestation of autoimmune pancreatitis, you should sharply limit your sugar intake, you can replace it with sweeteners.
- With the development of diabetes mellitus, there is a high risk of hypoglycemia (a sharp drop in the level of glucose (simple carbohydrate) in the blood, accompanied by disturbances of consciousness). Therefore, the patient must have sweet foods (lump sugar or candy) with him to restore blood glucose levels.
- Conservative (non-surgical) treatment. Glucocorticoids (synthetic analogues of adrenal hormones) - taking these drugs is the basis of treatment. Most patients need to take glucocorticoids for several weeks. Some patients may require long-term use of low doses of these drugs.
- Immunosuppressants are a group of drugs that suppress the excessive activity of the immune system (the body's defense system), which damages its own organs. Immunosuppressants are used when glucocorticoids are insufficiently effective or when their use is impossible (for example, when complications develop).
- Antispasmodics (drugs that relax the smooth muscles of internal organs and blood vessels) are used to treat pain that occurs when the pancreatic ducts narrow.
- Pancreatic enzymes are used to improve food digestion.
- Ursodeoxycholic acid preparations are used to improve the outflow of bile and restore liver cells.
- Proton pump inhibitors (drugs that reduce the production of hydrochloric acid in the stomach) are used to restore the surface of the stomach if it is damaged.
- Simple (short) insulin (a solution of the insulin hormone without special additives that increase the duration of its action) is usually used to normalize blood glucose levels during the development of diabetes mellitus.
- Long-acting insulins (solutions of the insulin hormone with special additives that slow down its absorption) can be used to normalize blood glucose levels during the development of diabetes mellitus.
- Surgery. Surgical decompression (restoration of normal lumen) of the pancreatic and bile ducts is used when there is significant narrowing of the ducts that cannot be treated with glucocorticoids. Duct stenting is preferable (introducing a stent into the narrowing of the duct - a mesh frame that expands the lumen), since this operation is usually easily tolerated by patients.
Autoimmune pancreatitis: clinical case
We conducted a study of a patient with a difficult to diagnose pathology of the pancreas – autoimmune pancreatitis.
History, complaints:
A 72-year-old man had no active complaints. After taking a more detailed history, it was possible to find out that the patient periodically experiences abdominal pain, and the blood glucose level rises to 7-7.5 mmol/l. Denies cancer history. Before MRI of the abdominal cavity and retroperitoneal space, the patient underwent an ultrasound examination (not in our clinic); conclusion – pseudotumor form of pancreatitis.
What was revealed during the MRI study:
Diffuse (along its entire length) increase in the size of the pancreas, smoothness of its outer contour, deformation of the gland’s “sausage-shaped” shape. At the same time, no MR signs of the presence of additional space-occupying formations in the pancreas were identified according to native and post-contrast studies. The pancreatic duct is unevenly narrowed throughout. The common bile duct (choledochus) is narrowed in its lower third and unevenly expanded in the overlying sections. In addition, in both kidneys, numerous additional irregularly rounded formations with fairly clear, even contours were identified, having uniform low intensity in all scanning modes.
At the same time, enlarged lymph nodes and space-occupying formations of other localization were not detected at the visualization level.
What we discussed at the Skype meeting on this occasion:
Together with the doctors of our operating companies, we discussed this complex case. The doctors of our OCs identified all the above-described structural changes, and during further discussion we were able to come to a consensus.
Among various diseases that can give a similar MR picture, a differential series was built: a) pseudotumor pancreatitis; b) acute pancreatitis with an increase in the size of the pancreas; c) pancreatic tumor with the presence of secondary (metastatic) changes in the kidneys; d) pseudotumorous pancreatitis, which, first of all, has pancreatic (in the pancreas) changes, but also extrapancreatic ones - in particular, multiple focal changes in kidney tissue.
What conclusions were reached at the Skype meeting:
From the resulting differential series, OK doctors consistently excluded individual diseases. It was revealed that acute pancreatitis is not characterized by the absence of edema around the pancreas, and the clinical data do not correspond to the expected diagnosis. A pancreatic tumor is not characterized by the homogeneity of the gland tissue, the absence of data for its focal lesion, as well as the presence of a narrowed pancreatic duct (in tumors, as a rule, it is dilated); Also, the clarity of the contours and uniformity of the structure of focal changes in the kidneys are not characteristic of metastatic lesions.
There were 2 pathologies remaining in the differential series: pseudotumor and autoimmune pancreatitis. During the joint discussion, the doctors expressed arguments in favor of each of the remaining pathologies. At the same time, it was found that the totality of the identified signs, namely: smoothness of the contour, narrowing of the gland duct, narrowing of the common bile duct in the distal and its expansion in the proximal (upper) sections, as well as the presence of extrapancreatic changes are characteristic of autoimmune pancreatitis. What else needs to be done: taking into account the results obtained, it is necessary to recommend that the patient consult a gastrosurgeon. An additional examination is possible - RCP - an X-ray research method in which the pancreatic duct and bile ducts are filled with an X-ray contrast agent in order to better identify areas of their narrowing (stenosis). A biopsy of pancreatic tissue may also be required, followed by morphological examination.
What did the MRI method give in this case:
It is possible to assume with very high confidence the autoimmune nature of changes in the pancreas and exclude its tumor lesion. Given the autoimmune nature of the disease, these patients require hormonal therapy (glucocorticosteroids), after which the condition improves. Such therapy is not carried out for other diseases from the initially established differential diagnostic series.
Interestingly, in this case, the presence of changes outside the pancreas (kidneys) helps to make the correct diagnosis of autoimmune damage to the gland. The nature of the changes in the kidneys is focal autoimmune lymphocytic infiltrates.
Often, according to medical sources, an incorrect diagnosis of pancreatic cancer can lead to unjustified surgical intervention and removal of part of the gland (resection) or referral of the patient for treatment to an oncologist, which is also unjustified.
What is necessary for final confirmation/verification of the diagnosis: biopsy and morphological examination.
On the presented T2 images in axial (left) and coronal (right) projections, an increase in size and a “sausage-shaped” deformation of the pancreas is determined; the presence of numerous similar focal kidney formations.
Complications and consequences
Complications of autoimmune pancreatitis.
- Impaired absorption of nutrients in the intestine. Protein deficiency (a condition that develops as a result of a reduction or cessation of protein intake into the body).
- Hypovitaminosis (insufficient content of vitamins in the body), especially fat-soluble ones (A, D, E, K).
- Loss of body weight up to cachexia (a state of deep exhaustion and weakness of the body).
- Disturbances of water and electrolyte balance in the body. Thirst.
- Edema.
- Dehydration (dry skin and mucous membranes).
- Cramps (paroxysmal involuntary muscle contractions).
- Subhepatic jaundice is a yellow discoloration of the skin, visible mucous membranes and biological fluids (for example, saliva, tear fluid, etc.) due to a violation of the outflow of bile.
- Infectious complications: inflammatory infiltrates (increase in the volume and density of some parts of the organ due to the accumulation of unusual cells in them - for example, microorganisms, blood cells, etc.) of the pancreas;
- purulent cholangitis (inflammation of the bile ducts);
- sepsis (blood poisoning – a disease caused by the presence of pathogenic microorganisms and their toxins (waste products) in the blood);
- peritonitis - inflammation of the peritoneum (the membrane lining the inner surface of the abdominal cavity and covering the organs located in it).
- Erosions (superficial defects) and ulcers (deep defects) of various parts of the digestive tract (esophagus, stomach, intestines).
- Subhepatic portal hypertension (increased pressure in the portal vein system (the vessel that brings blood to the liver from the abdominal organs) due to obstruction of blood outflow from the liver).
- Chronic obstruction of the duodenum due to its inflammation and compression by the enlarged pancreas.
- Abdominal ischemic syndrome (impaired blood flow to the abdominal organs) as a result of compression of blood vessels.
- Pancreatogenic ascites (accumulation of free fluid in the abdominal cavity).
- Cancer (malignant tumor - a tumor that grows with damage to surrounding tissue) of the pancreas.
Consequences of autoimmune pancreatitis.
- With timely, complete treatment and a short duration of the disease, complete restoration of the structure and activity of the pancreas is possible.
- With a long course of the disease, cicatricial changes in the pancreas lead to irreversible changes in its structure and activity, but even in these patients, complete treatment makes it possible to stop the progression (further development) of the process.
The prognosis for autoimmune pancreatitis depends on the severity of complications, concomitant autoimmune diseases (damage to one’s own organs by the immune system - the body’s defense system) and diabetes mellitus (carbohydrate - sugar metabolism disorders).
source
Autoimmune pancreatitis: symptoms, diagnosis and treatment
Autoimmune pancreatitis is considered a fairly rare disease. Its distinctive feature is that in addition to the pancreas, the bile ducts, lymph nodes, kidneys, salivary glands, lungs, etc. are affected.
The risk group consists of men over 50 years of age. According to statistics, women suffer from autoimmune pancreatitis almost half as often.
How does this disease manifest itself? What diagnostic methods do specialists use? What is the treatment?
Symptoms of autoimmune pancreatitis
What is autoimmune pancreatitis? An active pathological process leads to autoimmune antibodies, the so-called killer cells, becoming aggressive against healthy tissues of the body.
Inflammation occurs as a result of decreased immune defense. This disease is lifelong, progressing to a chronic stage, when acute attacks are replaced by a stable remission.
All of these stimulate the formation of pseudocysts, tissue damage and diabetes mellitus.
It can be extremely difficult to suspect the disease. The fact is that often autoimmune pancreatitis is completely asymptomatic. Even in the acute phase, no pronounced signs may be observed. Most patients become aware of the problem only after complications arise.
- Girdle pain of varying duration and intensity. Sometimes after eating spicy, fried or fatty foods, as well as alcoholic drinks.
- Jaundice, which is caused by narrowing of the ducts and the release of bile: yellowish skin, urine, mucous membranes, saliva, etc.
- Disorders of the digestive system: vomiting, diarrhea, nausea, loss of appetite, flatulence, dryness and bitterness in the mouth, accompanied by an unpleasant odor.
- Thyroid dysfunction.
- Weight loss, development of diabetes, increased fatigue, lethargy, lack of appetite.
- In case of liver damage, the patient experiences heaviness in the right hypochondrium, tissue compaction occurs.
- Shortness of breath and increased breathing may indicate hardening of the tissue in the lungs.
- Kidney failure, protein in urine.
- Pain while swallowing food.
Types of autoimmune pancreatitis
The disease occurs in several forms. Sometimes it is possible to distinguish one from the other only with the help of histological examination.
- The first type, as a rule, is observed in men over 60 years of age - lymphoplasmacytic sclerosing. It is characterized by yellowing of the mucous membranes and skin. The greatest blow falls on the pancreas. The prognosis is generally favorable. Recovery is ensured by steroid drugs.
- The second type is typical for women and men of young and middle age - idiopathic ductal-concentric with pathologies of the skin of the granulocytic type.
Classification of autoimmune pancreatitis according to the criterion of concomitant disorders that developed due to dysfunction of other systems and organs:
- Isolated, in which only the pancreas is injured.
- A syndrome when, in addition to the gland, other organs are damaged.
Based on the localization of the epicenter of the lesion, a diffuse variant is distinguished, i.e. the entire organ is inflamed, and focally with inflammation of the head.
Diagnosis of autoimmune pancreatitis
In order for the diagnosis to be correct, the patient will have to undergo a thorough examination of many specialists, including a therapist, gastroenterologist, endocrinologist, endoscopist, etc.
Attention is paid to weight, or rather its loss, the abdominal area is palpated for organ enlargement, a blood test is taken to determine the concentration of IgG4 immunoglobulin, and a general clinical blood test, in which particular importance is given to protein indicators and erythrocyte sedimentation rate, and biochemistry. Glucose levels are checked, a lipid profile, oncotests for the malignancy of neoplasms, a coprogram and a general urinalysis are done. The list of tests includes MRI, ultrasound, computed tomography, x-ray and biopsy.