Pancreatic enzymes, their types and functions
Various enzymes of pancreatic secretion break down certain substances, that is, they have a “narrow specialization”; they are all divided into 3 groups:
- Proteolytic, or proteases, break down proteins.
- Amylolytic, or carbohydrases, break down carbohydrates.
- Lipolytic, or lipases, break down fats.
Proteolytic enzymes
This group includes: trypsin, chymotrypsin and elastase. They break down large protein molecules into simpler components - peptides. Then carboxypeptidase is activated, which breaks down the peptides into amino acid molecules. They are absorbed in the small intestine, with the exception of nucleic acid, since it needs to be broken down into nucleotides. This occurs under the influence of nuclease enzymes (ribonuclease, deoxyribonuclease).
Pancreatic diseases are becoming more common; they cannot be left without treatment, as this is fraught with disastrous consequences.
Amylolytic enzymes
These include amylase and lactase. The first breaks down complex carbohydrates, or polysaccharides (starch), into dextrin and maltose, then into simple sugars - glucose and fructose, which can be absorbed in the intestines. Lactase breaks down milk sugar - lactose, which is found in dairy products.
Lipolytic enzymes
They act “in pairs”: lipase is activated in the intestine by colipase, after which it is able to break down fat molecules into glycerol and fatty acids.
A necessary condition for the digestion of fats is their emulsification with bile acids - crushing into small fragments, thereby creating a large surface of contact with lipase.
This is how the digestive process occurs in the intestines with the participation of enzymes.
Symptoms of pancreatic enzyme deficiency
For the natural digestion of food, the required amount of enzymes is required in the produced pancreatic juice. Several diseases have been discovered that are associated with defective enzyme compounds. According to the mechanism of their occurrence, they are classified as food intolerance.
food intolerance
Insufficiency of external secretion is observed when the digestive enzymes of the pancreas gland are reduced, it can develop at birth or have an acquired course. The development of the first case is observed due to the formation of gene damage, in the next, the occurrence of the disease develops due to a malfunction in the parenchyma of the pancreas.
Factors that indicate an acquired deficiency in the production of pancreatic enzymes often do not depend on the position of the organ, but are interrelated with the influence or disorder in the internal organs.
- Various diseases that are severe.
- Unfavorable environment.
- Lack of microelements, vitamins, proteins.
- Drug poisoning.
- Infectious diseases.
- Pathologies associated with changes in intestinal microflora.
All factors that sometimes cause severe digestive disorders have common symptoms and signs. The degree of their manifestation is justified by the severity of the underlying pathology or the intensity of the influencing cause.
- Decreased appetite.
- Diarrhea.
- A feeling of pain under the rib on the left, pain occurs both after eating and regardless of eating.
- Bloating.
- Belching air.
- Vomiting, nausea, in severe situations - repeated, without relief.
- Sudden weight loss, sometimes with a normal diet.
- Children face delays in physical development.
Similar symptoms may occur when pancreatic enzymes are of congenital or acquired etiology. Against the background of a gene disease, an enzyme deficiency can appear after birth, manifesting itself:
- lethargy;
- tearfulness;
- restless state;
- regurgitation after eating;
- frequent diarrhea with a foul odor.
lethargy in children
The patient's stool is continuous, with foamy contents and a piercing sour aroma, which often indicates malfunctions in the carbohydrate process and enzymes.
In addition to the general symptoms characteristic of diseases of the pancreas, there are also specific symptoms depending on disturbances in the production of the enzyme element in the pancreatic secretion.
- With a lack of lipase, steatorrhea develops - the amount of fat in excrement increases. The feces become yellow or orange in color, with an oily, liquid consistency.
- Lack of amylase is manifested by a constant desire to defecate, stool has a watery structure, the patient loses weight, and vitamin deficiency occurs. There is also an inability to tolerate certain foods containing a lot of carbohydrates; the procedure for absorbing elements in the small intestine changes.
- If there is a lack of trypsin, undigested protein fibers are detected in the excrement. The patient faces the development of anemia.
If such signs occur, you need to contact them, where tests will be taken and the required medications will be prescribed.
Features of application
There are a number of features that should be taken into account when taking enzymatic agents:
- The doctor prescribes the medications, selects the individual dosage and indicates the duration of treatment.
- During therapy, a strict diet must be followed, completely excluding alcoholic beverages, fatty and fried foods, and very sweet confectionery.
- It is important to make sure that the specified drug has the dosage indicated in the prescription.
- You cannot split the tablets or increase the dosage yourself.
- If there are any adverse reactions or no results, you should inform your doctor.
If the medicine is chosen correctly, literally after the first use, stools normalize, abdominal pain during digestion disappears, and the patient’s weight also normalizes.
Biochemical blood test for pancreatitis
The well-being of the whole organism is clearly visible when taking a biochemical blood test. During the inflammatory process, the following indicators deviate from the norm:
Pancreatic amylase, a pancreatic enzyme responsible for the breakdown of starch, increases.
Other representatives of the enzyme group, such as trypsin, elastase, phospholipase, and lipase, also increase.
Insufficient insulin synthesis causes an increase in serum glucose.
Bilirubin changes more than normal if a swollen gland blocks the bile ducts.
In some cases, transaminases increase.
Total protein decreases.
Elevated amylase is the primary symptom of pancreatitis in its chronic or acute manifestations. This enzyme helps break down carbohydrates. Lipase is responsible for the breakdown of fats. Trypsin and elastase are representatives of a group of proteases whose function is to cleave the peptide bonds of amino acids in proteins.
Biochemistry for pancreatitis
is done within 24 hours from the day the patient is delivered to a medical facility during an acute attack. During hospitalization, the dynamics of amylase are studied, preventing further attacks and complications. The doctor is informed about this by its continuing increase, coupled with severe pain.
What role do pancreatic enzymes play?
The pancreas belongs simultaneously to two systems of the human body: endocrine and digestive, so its working functions operate with double the load.
The first function is the production of pancreatic enzymes, which are immediately released into the duodenum, where they immediately break down the following substances supplied with a new portion of food: fats, proteins, carbohydrates.
The second responsibility is responsible for the endocrine system, while beta cells are responsible for the production of the insulin hormone in the human body. In turn, insulin supplies the body with glucose, which is also important for the proper metabolism of carbohydrates, fats and proteins.
Diagnosis of pancreatic insufficiency
Symptoms are polymorphic. Some patients lose their appetite and noticeably lose weight. Others, on the contrary, suffer from polyphagia, that is, excessive absorption of food.
But in both cases, there is insufficiently formed stool or diarrhea, which will stop against the background of a starvation diet. Possible vomiting. Often these signs mistakenly begin to suspect intestinal diseases. In such cases, the laboratory comes to the aid of the doctor.
The most reliable way to determine impaired pancreas function is to evaluate the TPI test (trypsin-like immunoreactivity). With the disease, the concentration of trypsinogen in the plasma decreases significantly, which allows differentiation with diseases of the small intestine.
A general clinical blood test for inflammation will show leukocytosis, accelerated ESR (erythrocyte sedimentation rate), an increase in the number of platelets, and, God forbid, anemia in cancer.
A biochemical laboratory will give reason to suspect loss of gland cells, showing an increase in amylase, trypsin, and bilirubin. Particularly indicative in this regard will be an increase in amylase in the urine. Fibrosis of an organ can be suspected when an excess of glucose is detected in the blood.
In the stool they find a picture of undigested fats and proteins.
To exclude (confirm) oncology, tumor markers are determined.
A number of other test analyzes are also carried out, which only a doctor can interpret correctly.
But the most reliable results are obtained from studies using probes. After stimulating the secretion of the gland with secretin and cholecystokinin, a series of samples are taken with an interval of ten minutes from the contents of the duodenum using a probe. This method examines the rate at which the gland secretes enzymes. The degree of secretion growth in each sample taken will indicate the condition of the organ.
Pancreatic enzyme preparations
Prescribed only by a doctor after examination and the presence of the following clinical signs:
- Decreased appetite;
- Pain in the left hypochondrium;
- Attacks of nausea and vomiting after eating;
- Heaviness and bloating;
- General malaise, weakness;
- Changes in the characteristics of the stool - it becomes oily, or, conversely, watery. The feces contain fibers of undigested food and mucus. Stool color is yellow or orange.
Pancreatic enzyme preparations are designed to correct pancreatic enzyme deficiencies. There are two groups:
- Enzyme preparations – bring enzymes to the level necessary for the correct breakdown of substances;
- Anti-enzyme drugs - to eliminate enzymes produced in quantities exceeding the norm.
Examples of enzyme medicines:
- Pancreatin is obtained from the pancreas of cattle. Composition: trypsin, amylase. Reduces the acidity of gastric juice. Other indications for taking Pancreatin are functional dysfunction of the liver and pancreas;
- Festal - consists of active substances of bile - amylase, lipase, protease. Indicated for use in patients with heaviness and pain in the epigastric region;
- Oraza - prescribed for pancreatic dysfunction.
Other drugs of the same group are Creon, Mezim, Enzistal, Pangrol, Panezinorm, of plant origin - Somilase and Unienzyme. Examples of antienzyme agents:
- Pantrypin - inhibits the activity of proteolytic enzymes;
- Aprotinin - inhibits the activity of polypeptides.
Groups of enzyme preparations
| Group | Recommended medicine | Patient diagnosis |
| Pancreatic enzymes | Mezim forte, Creon, Pancreatin, Penzital | Chronic diseases of the pancreas |
| Gastric mucosal extracts | Abomin, Acidin-pepsin | Hypo- and anacid gastritis |
| Combination preparations containing pancreatin in combination with bile components | Digestal, Festal, Panzinorm forte, Enzistal | Hypomotor biliary dyskinesia |
| Important! By increasing pancreatic secretion, stimulating intestinal motility and gallbladder motility, they increase intraintestinal osmotic pressure and, consequently, abdominal pain syndrome. Contraindicated in patients with edematous and painful forms of chronic pancreatitis. | ||
| Plant enzymes | Pepfiz, Oraza | Drugs in this group are prescribed for allergies to animal meats. |
| Important! Plant enzymes cannot be used for bronchial asthma and allergy to fungi and penicillin antibiotics. | ||
| Combined enzyme preparations containing pancreatin in combination with plant enzymes and vitamins | Wobenzym | Chronic inflammatory diseases of the gastrointestinal tract, hepatitis, dysbiosis |
| Disaccharidases | Thylactase | Lactase deficiency of varying severity |
If there are problems with the functioning of the pancreas, you should not delay a visit to the doctor - pancreatitis, detected in the early stages, can be treated much better than the later stages of this disease. The use of the listed medications, their dosage and course of treatment must be agreed upon with the attending physician.
The best enzymes for adults
In this rating group we have collected the most popular digestive enzymes suitable for adults.
Micrasim
Rating: 4.9
A complex of pancreatic enzymes - pancreatin - containing amylases, lipases and proteases; placed in microspheres, which, in turn, are packaged in capsules. The capsule dissolves in the stomach, the microspheres mix evenly with the food bolus, passing into the intestines and dissolve there under the influence of an alkaline environment, releasing enzymes. Thus, the enzymes are evenly mixed with food and act as efficiently as possible.
Clinical recommendations for the treatment of exocrine pancreatic insufficiency specifically stipulate that the only effective form of supplying enzymes to the intestine are microspheres or microtablets, which are activated only in the lumen of the small intestine.
Take capsule three times daily with meals. Given the form of release of the medicine, the capsules cannot be chewed - if the shell of the microspheres is damaged, the enzymes are inactivated in the acidic environment of the stomach.
If the drug is used occasionally for overeating, a dosage of 10,000 units is sufficient. In other cases, the drug must be prescribed by a doctor, who will determine the required dose.
Possible analogues are Ermital, Creon.
Advantages
- microgranules ensure more efficient enzyme functioning.
Flaws
- high price.
Mezim
Rating: 4.6
Economy option: the same extract of animal pancreas - pancreatin, as in the previous product, but placed in enteric-coated tablets. Enzymes are not inactivated in the stomach, they begin to act only once they reach the intestines, but given that the tablet needs time to dissolve, it is more difficult to talk about the effective interaction of enzymes with food (as we remember, the higher the activity of enzymes, the higher their area of contact with food suspension ).
However, given the five-fold difference in price with the previous drug from our rating, it is not surprising that the drug has many fans. Nevertheless, we would recommend it primarily to healthy people, whose quality of life does not depend too much on the effectiveness of the medicine taken.
Possible analogues – Penzital.
Advantages
- low price.
Flaws
- less effective compared to drugs containing enzymes in microgranules.
Festal
Rating: 4.5
And again pancreatin, that is, amylase, lipase and protease. In combination with the enzyme hemicellulase, which breaks down fiber (normally produced by normal intestinal microflora) and bile components.
It is because of the complex of bile acids that we included the product in the rating of the best enzymes for digestion. They facilitate the absorption of fats and fat-soluble vitamins and correct biliary insufficiency - reduced activity of the gallbladder or its complete absence. Therefore, among the indications for the use of Festal, in addition to pancreatic insufficiency and overeating that are traditional for enzyme preparations, there are also pathologies of the liver and biliary tract:
- alcoholic and toxic diffuse liver damage, cirrhosis;
- biliary dyskinesia,
- cholecystitis,
- condition after cholecystectomy.
Hemicellulase, by breaking down fiber, helps reduce bloating and flatulence. characteristic of dysbiotic conditions.
Possible analogues: Enzistal.
Advantages
- contains bile acids that correct biliary insufficiency;
- affordable price.
Flaws
- reduced enzyme efficiency compared to preparations containing microgranules.
Acidin-pepsin
Rating: 4.4
While all other products in our rating are designed to support the functioning of the small intestine, this drug contains a complex of enzymes to improve digestion in the stomach.
As already mentioned, this is where the first stage of protein digestion occurs. But for gastric proteases to work, an acidic environment is necessary. With atrophic gastritis, the glands that produce both enzymes and gastric juice die due to prolonged inflammation. Digestive insufficiency in the stomach is manifested by heaviness after eating, rapid satiety, and belching of air. There are also frequent manifestations of dumping syndrome caused by the ingestion of large amounts of insufficiently processed food into the intestines:
- sudden weakness after eating, even to the point of fainting;
- drowsiness,
- pallor,
- sweating,
- hiccups
In such a situation, the doctor may prescribe Acidin-pepsin.
Contains a complex of gastric enzymes (pepsin) and betaine hydrochloride. Pepsin is an extract from the mucous membrane of the pork stomach. Betaine hydrochloride, when released into water, hydrolyzes (decomposes) to release hydrochloric acid, providing an optimal environment for the action of pepsin.
Two tablets should be dissolved in half a glass of water and drunk with meals.
Advantages
- low price.
Flaws
- inconvenient way to use.
Diagnosis and symptoms of decreased exocrine function
Laboratory tests are performed to determine which enzymes the pancreas does not produce in sufficient quantities. Based on the results of blood, urine and feces tests, instrumental studies, as well as taking into account existing symptoms, enzyme preparations may be prescribed.
The enzyme content standards are as follows:
- blood: amylase – 29-99, lipase – 22-66, trypsin – 19.7 – 30.3 mg/l;
- blood serum: elastase – 01 – 4 ng/ml;
- urine: amylase (diastase) – max 100 units/l;
- coprogram: elastase – from 200 mcg/g.
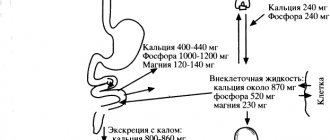
Pancreatic enzymes are produced in the acinar cells of the pancreas, then through the smallest tubules they enter larger ducts that form the main duct - Wirsung.
Deficiency of pancreatic enzymes leads to serious disorders of digestive function and the functioning of the body as a whole. In case of excessive production of enzymes, acute inflammation of the pancreas is diagnosed - pancreatitis. A decrease in enzyme synthesis means the disease becomes chronic.
The following reasons can lead to inflammatory-destructive changes in the pancreas and replacement of glandular tissue with fibrous tissue:
- overeating and abuse of fatty foods and alcoholic beverages;
- the presence of neoplasms - cysts, tumors (both benign and malignant), fibrosis;
- pathologies of the duodenum and biliary tract;
- surgical operations on the pancreas.
With enzyme deficiency, a number of characteristic symptoms occur:
How to check the pancreas
- polyfecality (large volumes of excreted feces);
- mushy, liquid stools of a grayish color with a shiny, oily surface and an unpleasant odor;
- the presence of undigested food fragments in the stool;
- feeling of fullness in the stomach and nausea, heartburn;
- unpleasant taste in the mouth;
- decreased appetite;
- flatulence, churning in the stomach;
- weight loss, anemia, weakness, insomnia and headache;
- abdominal pain after eating;
- intolerance to fatty and spicy foods.
Since the synthesis of lipase decreases first, stool disorder is one of the first to appear - it becomes viscous or semi-liquid. It is worth noting that the symptoms are almost the same both with an excess of enzymes and with a deficiency. However, in case of excessive production of enzymes, body temperature may increase, and the pain syndrome becomes sharp and pronounced.
Violation of the exocrine function of the pancreas requires mandatory treatment, since it can lead to the development of such serious diseases as pancreatic necrosis, gastric ulcer, hepatitis and cirrhosis
Norm
So, what are the normal levels of pancreatic chemistry tests?
Total protein is normally 75-85 g/liter. This indicator depends on age and gender. It indicates adequate nutrition and digestion of food. Consequently, in chronic pancreatitis, when there is severe enzyme deficiency, the level of total protein will decrease.
Amylase is usually no more than 64 units. During acute inflammatory processes of the pancreas, its level rises tens, hundreds and thousands of times. The increase lasts 2-3 days, after which the substance is removed from the blood. Amylase is used to make the diagnosis of pancreatitis. It increases during an attack in every fifth patient.
Lipase in a healthy person reaches 190 units. All values higher than this figure can be regarded as acute pancreatitis. Lipase is a more specific test. The enzyme level increases 3-5 days after the attack and remains at high levels for 10-14 days. After this, lipase slowly decreases.
Elastase is 0.1-4.0 ng/ml. The indicator is very specific for inflammation of this organ. The substance is found only in pancreatic tissue. It increases during an acute process 6 hours after the onset of the attack. Elastase decreases by the 10th day of illness. The enzyme reacts in almost all patients.
Glucose varies from 3.5 to 6.2 mmol/liter. Glucose increases in chronic pancreatitis complicated by diabetes mellitus.
Varieties
Pancreatic enzymes are different. They ensure the breakdown of proteins, acidic fats and the normal course of carbohydrate metabolism. When the action of enzymes is activated, they form simple molecules, which then enter the systemic bloodstream and through it enter the body's cells.
Pancreatic enzymes promote complete absorption of nutrients in the body. But each of them has its own “responsibilities”. Some of them ensure the production of insulin and glucagon (they are called endocrine), the other is directly responsible for the digestion of food components (exocrine).
Exocrine cells of the pancreas provide the production of:
- electrolytes;
- water;
- bicarbonates;
- enzymes for digesting proteins, fats and carbohydrates.
In turn, enzymes produced by the pancreas are divided into the following types:
- Amylase. This enzyme is responsible for processing glucose, which enters the body with food. Amylase first acts on starch and then breaks it down into carbohydrates and monosaccharide units. The former are absorbed by the cells of the body and serve as energy, the latter are excreted naturally (during bowel movements).
- Lipase. This enzyme “works” only with fat. Since this element of food does not have the ability to be absorbed into the blood, for better absorption, lipase breaks fat into smaller components - glycerol and fatty acid.
- Proteolytic enzymes. This enzyme helps break down proteins. It also breaks them down into micro components that are easily absorbed by the body. However, this process is much more complicated than those described above. Initially, the protease breaks down proteins into molecules that are built from the remainder of the amino linkage, that is, peptides. Then they are crushed into organic compounds and only after that they are absorbed.
Activation of pancreatic enzymes
Of all the substances produced by the pancreas, proteolytic enzymes in active form are considered the most dangerous. They are produced by the gland in a neutralized state, and their action is activated by trypsin. Its synthesis also occurs in an inactive form in the form of trypsinogen. However, unlike other enzymes, trypsin can activate itself independently. To do this, he needs to isolate the active part from trypsinogen. And so that this process does not activate in the tissues of the gland and does not have a destructive effect on them, it occurs in the intestines through the release of enterokinase from the walls of this organ.
This process can be disrupted by various factors: both external and internal. But most often, the process of activation of trypsin is disrupted by the destruction of cells by cytokinase. And in this case, collagenase poses a great danger, which has a destructive effect on the pancreatic septum, which leads to the opening of undamaged areas of the gland and their further damage.
The protective function against the acid breakdown of these substances is performed by a special secretion, which is also synthesized by the pancreas. It has an alkaline environment and is presented in the form of a substance generator.
Substances produced by the pancreas perform various functions
The pancreas also produces inhibitors, which are also directly involved in the process of digestion and metabolism. Inhibitors also have their own varieties:
- pancreatic glucagon, which controls the production of fluid, bicarbonates and other enzymes;
- pancreastatin, which reduces the release of acetylcholine produced in the efferent endings of the vagus nerve;
- neutropeptide, which contains calcitonin information peptide, which stimulates somatostatin, and enkephalin, which reduces the production of acetylcholine.
In total, the pancreas synthesizes about 20 types of enzymes from inactive precursors. The amount of enzymes produced is controlled by the quantity and quality of food consumed by a person. If a person often eats “heavy” foods (fatty, fried, flour, etc.), then the synthesis of enzymes increases. And in cases where this happens too often, the pancreas is overloaded, pathological processes arise in it, which entail disruption of enzymatic functions and the development of pancreatitis. Therefore, doctors urge all their patients to carefully monitor their diet. After all, only properly selected and balanced nutrition helps prevent the development of pancreatic diseases and maintain its functioning.
Operating principle
The principle of action of enzyme preparations is based on participation in the process of food digestion. After taking the medicine, their active components help break down proteins, fats and carbohydrates. As a result, the components are correctly distributed in the body, which helps prevent the development of severe complications.
The substances in the products create a kind of protective shell on the gastric mucosa, which prevents the negative effects of food and helps speed up the healing process of tissue lesions.
Pancreatic enzymes (the drugs have similar properties and often contain similar active ingredients) help speed up the digestion process and prevent the development of metabolic disorders.
Patients note easier digestion and weight loss due to the correct distribution of food components in the body and the involvement of fatty deposits in metabolic processes.
When using medications, there is an elimination of heaviness and heartburn, pain and other symptoms that accompany disorders of the digestive tract.
Diagnostics of amylase activity
You should start with blood amylase, which is produced by the pancreas and promotes rapid digestion. The main function of amylase is the breakdown of starch or glycogen to form the final reaction product - glucose. Alpha-amylase has become the most common due to its activity.
Normal levels of amylase in the human body are considered to be: • in the blood 16-30 μkal/l; • in urine 28-100 μ catal/l
Figures for amylase activity show a number of pathologies of the pancreas and different forms of pancreatitis. If amylase levels in the urine and blood are low, the patient can be diagnosed with cystic fibrosis or a previous attack of pancreatitis. An increase in amylase levels indicates severe alcohol poisoning, mumps, ectopic pregnancy, exacerbation of pancreatitis, stones, tumors in the pancreas.
And increased amylase in the urine indicates cholecystitis, appendicitis, pancreatitis or a gastrointestinal ulcer.
List of drugs
Of the pancreatic enzymes in medications, there are three main ones:
- amylase;
- lipase;
- protease.
The activity of the drug is calculated using lipase. This substance begins to act earlier than others. The list of pancreatic enzyme preparations includes few items. Their mechanism of action is almost the same. The difference is in the release form, which is responsible for the bioavailability of the drug, that is, its absorption by the body. Enzyme preparations are obtained from the pancreas of bulls, less often pigs.
Pancreatin
The very first drug from this group. Contains three active ingredients:
- protease - 200 units;
- amylase - 3500 units;
- lipase - 4300 units.
Pancreatin
The purpose of prescribing the drug is to improve the digestion of food. Used for inflammation of the pancreas and bile ducts. It is also prescribed for preparation for radiography or ultrasound of the abdominal cavity - to eliminate flatulence.
There are practically no contraindications to use - with the exception of individual intolerance. Take Pancreatin tablet before meals. Dosage calculations for children are based on body weight. A short course (3-4 days) is indicated to eliminate the consequences of a diet violation. Long-term use of enzymes (several years or lifelong) is recommended for chronic pancreatitis.
Composition and groups of enzyme preparations
Depending on the composition of the drugs, experts distinguish 3 groups of medications. In most cases, they contain enzymes that are necessary for patients with various digestive disorders. Some products are enriched with plant extracts, animal bile and microelements, which enhances their effectiveness and expands the spectrum of action.
Pancreatic enzymes
The vast majority of drugs contain pancreatin. This substance includes amylase, lipase and protease. The first enzyme is aimed at processing carbohydrates, the second - fats, the third - proteins. As a result, normal and rapid processing of food components occurs.
| Group of medicines | Peculiarities |
| Complex medicines | Typically, the products contain pancreatin, as well as trace elements and animal bile extracts. The drugs have pronounced properties, help improve the functioning of the digestive tract and reduce the load on the pancreas. |
| Maintenance medications | These medications contain only pancreatin, their action is aimed at improving digestion with minor disorders. In case of serious diseases, the drugs do not have a pronounced therapeutic effect. |
| Combination medications | These products usually contain not only pancreatin, but also some other components that help have a positive effect on the digestive tract of patients. |
Depending on the cause of the disorder, specialists select the most appropriate medications.
Signs of Enzyme Deficiency
The pancreas has the unique ability to adapt to the diet and produces exactly as many enzymes as necessary for normal digestion. For example, when carbohydrate foods predominate, amylase is secreted mainly, more trypsin is required for protein processing, and consumption of fatty foods contributes to increased lipase production.
Under the influence of a number of factors, pancreatic function may decrease, which is inevitably accompanied by deterioration of digestion due to a lack of enzymes. Impaired secretion and enzyme deficiency most often result from pancreatitis, in which the organ becomes inflamed and the glandular tissue is gradually replaced by connective tissue.
Damage to the pancreas is accompanied by the following symptoms:
- pain syndrome in the upper abdomen under the ribs;
- increased sweating and tachycardia;
- fever and general weakness;
- yellow tint of the skin and sclera;
- upset stomach, nausea and vomiting.
Modern enzyme preparations are made from the pancreas of cattle and pigs;
their effectiveness depends on the form of release and dosage. You can determine which enzyme is missing by looking at the color and consistency of the stool. Thus, with amylase deficiency, the urge to defecate becomes more frequent, and the stool becomes watery due to impaired absorption in the small intestine. Carbohydrate intolerance, vitamin deficiency and weight loss are observed.
Lipase deficiency is accompanied by a condition called steatorrhea, where the amount of fat in the stool increases. The color of the stool changes to yellow or orange, and the consistency becomes oily-liquid.
A lack of trypsin results in the presence of undigested fiber in the feces, which often leads to anemia.
Enzymes in postoperative therapy
The pancreas lacks enzymes during the postoperative period. In order to compensate for this deficiency, patients are prescribed enzyme preparations. After surgery, for normal restoration of the organ, enzyme medications should be taken in long courses.
The effectiveness of taking such drugs by patients during the rehabilitation period has been proven by scientific studies in different countries of the world.
Particularly effective are medications that contain bile acid with an enzyme that reduces bloating and helps to better absorb plant foods:
- Festal;
- Enzistal;
- Digestal;
- Pankurman.
Bile acid, which is part of the medicine, regulates the functions of the pancreas and the process of bile secretion.
To reduce gas formation in the intestines, use:
- Pankreoflat;
- Pepphys.
Strictly following the doctor’s prescriptions and following a diet will speed up the recovery of the pancreas in the postoperative period.
Reception features
You can take enzymes for inflammation of the pancreas only on the recommendation of a doctor. The required drug, dosage, frequency of use and duration of therapy can only be determined by a specialist. In this case, the patient’s condition, complaints, results of laboratory and instrumental examination methods, the severity of the pathological process, the degree of pancreatic insufficiency and other associated factors must be taken into account.
Enzyme preparations are indicated for use by people who have impaired production of digestive enzymes by the pancreas. The composition of the medicines includes lipase, protease, amylase and other components important for the digestion of food.
For pancratitis, Enzistal reduces the load on the pancreas.
The drug Creon can be taken to activate the active components in the duodenum.
The main enzymes for pancreatitis include Mezim.
Enzymes include Mezim, Panzinorm, Pankurmen, Ermital, Enzistal, Pancitrate, Penzital, etc. The active substance in each preparation is pancreatin. The main forms are tablets and capsules, which have an acid-resistant shell, due to which the activation of the active components and their mixing with the food mass occurs in the duodenum. Bile is excreted into the intestinal cavity, which actively participates in the digestive process.
You need to take medications with meals, this will ensure the breakdown of fats and help digest fiber.
In chronic form
Enzymes for chronic pancreatitis are safe means with which one can ensure normal digestive processes, the disruption of which develops as a result of absolute or relative insufficiency of the pancreas.
Pancreatitis: treatment + diet. Effective treatment of the pancreas without drugs or with drugs.
By reducing the load, rapid restoration of the affected tissue occurs.
In the acute stage
In the acute stage of the disease, the use of enzyme preparations is strictly prohibited. This medicine can further worsen the patient's condition.
Why should you not take enzymes during exacerbation of pancreatitis?
In acute pancreatitis, tissue inflammation and swelling occurs.
This leads to disruption of the synthesis of lipase, amylase and other enzymes in the digestive tract. The supply of enzyme preparations from the outside can further activate the work of the pancreas.
As a result, the organ experiences increased stress, which adversely affects the patient’s well-being. Sometimes self-digestion of organ tissue occurs, which leads not only to severe pain, but also damage to pancreatic tissue.
Methods for diagnosing pathologies
To diagnose the functional state of the pancreas, biochemical and instrumental research methods are used.
In addition, liver functions are determined - bilirubin, transaminases, total protein and its fractions, blood glucose.
The presence of amino acids is detected in the urine.
To detect phenylketonuria, a congenital pathology of the pancreas, the determination of phenylalanine in the blood is used. These tests are performed in maternity hospitals on all newborns on days 4–5 of life. According to WHO recommendations, the pathology is included in the list of hereditary diseases recommended for early diagnosis.
Celiac disease is detected by serological diagnostic methods with the determination of antibodies and antigens for gluten intolerance.
Lactase deficiency is confirmed by the results of blood tests and analysis of the lactose curve: lactose stimulation is carried out - the patient is given lactose in a small dosage, then the blood is tested. The level of lactose in the urine is also determined, where it enters in small quantities.
Instrumental research methods are used for differential diagnosis and exclusion of organic damage to pancreatic tissue or the presence of stones, cysts, and inflammatory processes. Conducted:
- Ultrasound,
- CT,
- MRI.
What tests are needed to determine enzymes?
Blood and urine tests are studied for the activity of the main enzymes:
- amylase,
- trypsin,
- lipases.
A coprogram in the presence of undigested muscle fibers, fats, and starch particles indicates insufficient enzyme content.
The main indicator when studying stool analysis is elastase. Reducing it can help cure the disease and make the digestive organs function normally.