In some cases, inflammation of the mucous membrane in the esophagus occurs due to exposure to Candida fungi. These microorganisms belong to the opportunistic microflora of the digestive tract. If the fungus begins to multiply in large quantities, then this is referred to as the pathological development of the disease.
When this pathogen infects the walls of the esophagus, candidal esophagitis is diagnosed. The disease can be asymptomatic or manifest itself in the form of serious signs and stages.
What is candidal esophagitis?
The microflora of the human body also includes Candida fungus. Pathogens are located on the mucous membranes of the mouth, stomach, intestines and vagina. Immunity determines the vital activity of the fungus, and when exposure to irritating or favorable factors occurs, microorganisms begin to multiply. Depending on the location of the lesion, accompanying symptoms are observed.
Candidal esophagitis is considered a fungal infection of the esophageal mucosa. The disease is common in only 2 forms of pathology:
- acute;
- chronic.
In the acute course of a fungal infection in the esophagus, the intensity of inflammation increases. During the initial stages, the patient may exhibit primary signs of pathology. The incidence of the disease in acute form is due to poorly treated pathologies of the digestive tract. The symptoms of fungal esophagitis are characterized by a rapid increase in symptoms.
During the acute form, mycotic esophagitis is isolated. This disease is classified as a secondary pathology, which develops as a result of inflammatory processes in the digestive organs. Candida fungi are located in the lower part of the esophagus.
When chronic fungal esophagitis occurs, the symptoms are not pronounced. The common cause of the development of this disease is considered to be improper treatment of pathologies of the digestive organ. Otherwise, if the patient did not seek help when candidal esophagitis was in acute form. Symptoms appear during relapses.
Photos of different types of esophagitis
The patient should know that the chronic form of candidal esophagitis cannot be completely cured. Therefore, it is recommended not to start the disease at the moment the first symptoms appear. Otherwise, the patient will need long-term treatment, which will help increase the duration of remission.
If the patient does not seek help for a chronic form of fungal inflammation of the esophagus, then there is a risk of complications. Candida pathology develops into ulcerative formations, which in medicine is referred to as erosive esophagitis. Foci of inflammation are able to penetrate into the deep layers of the epithelium.
Diagnosis of mycosis
Candidal esophagitis in most cases occurs when the mucous membrane of the overlying organs of the digestive tube is damaged, so the presence of fungal infection of the oral cavity and pharynx can be an indirect sign of the disease. However, if the oral mucosa is not affected by the fungus, this is not evidence of the absence of fungus in the esophagus.
Since the symptoms of the disease are nonspecific, diagnosis is possible only after instrumental and laboratory examinations. In order to visually assess the condition of the esophageal mucosa, an endoscopic examination is performed. A soft tube equipped with a video camera is inserted into the patient through the mouth.
With candidal esophagitis, the mucous membrane is red, easily wounded, a whitish or yellowish coating is visible on its surface, which can be easily removed, however, erosions and inflamed tissue are found underneath. There are three types of esophageal lesions:
- separate foci, the plaque of which consists of keratinized epithelial cells, fungal filaments and leukocytes. Pseudomycelium invades between squamous epithelial cells;
- Dense deposits form. The threads penetrate the submucosal layer;
- pseudomembranous overlays that develop on lesions of the mucous membrane. Pseudomycelium penetrates necrotic tissue, penetrates the muscular lining of the esophagus and affects blood vessels.
The fungus grows more intensively where necrosis is more pronounced. In a chronic course, connective tissue grows around the source of inflammation or a granuloma forms. During an endoscopic examination, materials are taken for histology in order to make a differential diagnosis between candidiasis, aspergillosis and nocadia.
A cytology brush or balloon catheter passed through the mouth or nose can be used to quickly diagnose esophageal infections, and a special probe can be used to prevent contamination. In the laboratory, using certain methods, it is possible to examine the yeast-like fungus itself, its pseudomycelium and phagocytosed elements.
At the initial stage of candidiasis, a necrotic-inflammatory reaction occurs
Determination of the serotype and identification of the candida species is carried out using specific immunofluorescence. The cultural method, which consists of growing a colony for several days on a nutrient medium, makes it possible to judge the etiology of the infectious process. An important diagnostic criterion is an increase in antibody titers and an increase in the number of fungi during repeated studies of pathological material.
Why does the disease develop?
Factors in the development of candidal esophagitis are considered to be untreated diseases of the gastrointestinal tract. However, antibacterial therapy creates a favorable environment for the proliferation of fungi. Treatment with strong medications should be combined with the use of vitamins. Antibiotics disrupt the microflora of the digestive organs.
Common causes of fungal inflammation of the esophagus are:
- taking hormonal medications;
- oncological pathologies;
- diseases of the endocrine system;
- HIV or AIDS;
- connective tissue pathologies;
- diabetes;
- frequent consumption of alcoholic drinks.
In some cases, candidal esophagitis occurs due to decreased immunity. Especially when a person undergoes rehabilitation after surgery on the digestive organs, the body is under stress. If the recovery process is not followed by the patient, then this becomes a favorable environment for the development of fungi of the genus Candida.
Mycotic esophagitis: what it is and the causes of the disease
Candida yeast is present on the skin and mucous membranes of most people. But if a person is healthy, these organisms “sleep” and may never make themselves known once in their life. Favorable conditions are necessary for their activation. As soon as they arise, the fungi “wake up”, begin to multiply and cause pathogenic processes.
Most often, Candida causes the well-known thrush. And in some cases, its “activity” is localized in the esophagus. This is how fungal esophagitis occurs, the treatment of which can take quite a long time.
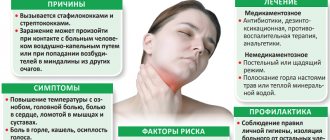
Pathogenic bacteria are activated when a person has a reduced immune system or the body is weakened after surgery, illness, chemotherapy, etc. Often the trigger for the spread of fungus is taking a large number of medications (in particular, hormonal and antibacterial). The following categories of people are at risk:
- those suffering from cancer, AIDS or diabetes;
- chronic alcoholics;
- people who have had organ transplants;
- women who regularly take hormonal contraceptives.
One more category should be highlighted. These are newborns whose mother had thrush during pregnancy. During the birth process, the baby can catch an infection, and since his immunity is still very low, esophagitis immediately develops.
Clinical picture of fungal esophagitis
When the disease develops, the symptoms are clearly expressed in acute mycotic inflammation. Symptoms of candidal esophagitis include many manifestations that are easily confused with other signs of pathologies of the digestive tract.
When inflammation occurs:
- heartburn;
- increased body temperature;
- pain when swallowing;
- dry cough;
- anemia;
- chest pain after eating;
- sour belching;
- bad breath;
- pressure in the abdomen;
- dizziness;
- attacks of nausea after eating.
A clear sign of candidal esophagitis includes dysphagia or odynophagia, when the patient has difficulty swallowing food. Clinical manifestation occurs in 70% of cases. In addition, damage occurs not only to the esophageal mucosa, but also to the spread of infection into the oral cavity.
When the fungus multiplies throughout the mucous membrane of the esophageal tube, symptoms appear in the mouth. Lesions or a cheesy coating appears on the tongue. Foci of inflammation are easily removed. There is swelling under the opened wound. The color of the inflammation takes on a bright red hue. At the same time, patients often experience abdominal pain, attacks of nausea and vomiting. When such signs appear, biological discharge is observed with a white film. Heartburn is observed along with a sour taste.
The prolonged course of the disease forces the patient to abstain from eating. This is associated with the occurrence of unpleasant pain while eating, which leads to weight loss. Complications from inflammation of the mucous membrane occur infrequently. However, with fungal esophagitis of the esophagus, bleeding occurs. An unpleasant symptom is accompanied by vomiting with blood. In this case, the patient feels general malaise and weakness.
When vomiting blood occurs, the unpleasant consequence is complete destruction of the wall of the esophagus. This leads to perforation. Therefore, if the symptoms described above occur, you need to seek medical help, otherwise the process will lead to death.
How and who carries out the diagnosis?
If signs of the disease appear, you should seek help from a gastroenterologist. The doctor diagnoses the patient for the presence of candidal esophagitis. First you will need to find out the complaints and conduct an inspection. The patient is then sent for laboratory tests.
Methods for diagnosing fungal inflammation of the esophagus include:
- radiography;
- fibrogastroscopy;
- general blood analysis;
- X-ray examination.
If the diagnosis is carried out in a woman, then fibrogastroscopy is done with a targeted biopsy. This helps to detect the source of the inflammatory process. In addition, fibrogastroscopy determines the severity of damage to the mucous epithelium. The use of x-ray examination makes it possible to observe incomplete closure of the lumen at the bottom of the esophageal tube. In the results obtained, the doctor examines the structure of the mucous epithelium. In this case, damage, dysplasia or metaplasia are observed.
Establishing the extent of the disease
Pathology is divided into several degrees. This depends on the severity of the inflammatory process. Therefore, candidal reflux esophagitis of the first severity is determined using formations on the walls of the esophageal tube. The area of all erosions combined should not cover more than 50% of the mucous epithelium.
To confirm the 2nd degree of severity of fungal esophagitis, a sign in the form of a white coating is isolated. Foci of inflammation fill more than 50% of the area of the esophagus. The pathology is accompanied by hyperemia of the mucous tissue.
When the patient has stage 3 inflammation, the white plaques begin to unite. This leads to the formation of folds. Doctors note that in some cases ulcers can occur on the mucous membrane.
To confirm stage 4 candidal esophagitis, more pronounced plaques, folds and enlarged ulcers should be observed during laboratory tests. Doctors identify swelling of the mucous epithelium. The tissues of the esophageal tube become loose.
Pathology treatment methods
When the gastroenterologist has established the diagnosis and extent of the disease, they begin to treat candidal esophagitis.
Therapeutic measures to eliminate the fungal inflammatory process are carried out comprehensively . Otherwise, the treatment will not provide a positive result. Therefore, therapy consists of medications, proper nutrition and diet.
Traditional methods in the treatment of candidal inflammation of the esophagus are used as additional help, nothing more.
Medications
Taking antifungal medications for candidal esophagitis is required as prescribed by a doctor. Inflammation in the esophageal tube is relieved:
- Ketoconazole;
- Nystatin;
- Fluconazole.
To eliminate additional symptoms of the disease, other medications are prescribed. In most cases, you want to prevent heartburn. That's why antacids are used.
The effectiveness of antifungal therapy lies in the sensitivity of pathogens to the drugs taken. To do this, the doctor conducts a histological examination.
Sometimes patients complain of insomnia, so they recommend taking sedative medications. However, this condition can occur due to taking medications. There are rare cases when, due to sleep disturbances, a patient turns to a psychologist or neurologist. The patient complains of irritability after therapy. Doctors recommend taking more vitamins. In addition, immunostimulants help.
Treatment at home
Among the folk recipes for additional therapy of candidal esophagitis, decoctions are taken. Herbal medicines for the preparation of products are used with anti-inflammatory and bactericidal properties. In most cases, chamomile is used.
To prepare an anti-inflammatory remedy with chamomile, you will need 2 tbsp. l. raw materials. In addition, licorice root, lemon balm and motherwort leaves, 1 tbsp each, are added to the dried plant. l. The raw materials are brewed with 500 ml of boiling water. The resulting drink is infused for 2 hours. Then the product is filtered, and it is recommended to take half a glass 3 times a day. Thus, decoctions are prepared from the leaves of mint, calendula, oak bark or sage.
Proper nutrition and diet
In addition to medications, a therapeutic diet for candidiasis esophagitis is considered an important point in the recovery process. If inflammation is severe, the patient is advised to fast. If difficulties arise while eating due to obstruction of the esophagus, the patient is fed with a tube.
When candidal esophagitis occurs, it is necessary to avoid the following products:
- spicy dishes;
- fatty foods;
- sweet;
- bakery products;
- alcoholic beverages;
- smoked dishes;
- canned products;
- citrus fruits;
- fermented milk products.
Diet and nutrition for candidal esophagitis should be balanced. Therefore, it is recommended to eat dietary meat and fish. Steamed or pureed vegetables will be useful for restoring the body. Otherwise, the products are baked in a steam oven. After eating food, you should not take a horizontal position.
Conservative treatment
How effective such treatment will be depends on many factors. Depending on the form of the disease, its location in the body, the degree of damage, and if there is no allergy to the medications prescribed to the patient.
Taking medications that kill the fungus is the most important part of treatment.
Additionally, the patient is prescribed:
- Special diet. The food that is allowed to be consumed does not contain harmful, dangerous substances, and also prevents the proliferation of Candida fungi. The diet must be prescribed by the attending physician, taking into account the individual indications of the patient.
- Be sure to take vitamin complexes, the body will recover soon.
- Lead an active healthy lifestyle.
- Give up bad habits forever. They interfere with treatment and provoke the development of pathology in the future.
- Treatment using traditional medicine. Be sure to consult your doctor before using such medications. Otherwise, you will cause irreparable harm to the sick body, aggravating the course of the disease.
Take herbal and berry decoctions, tinctures, teas. It is recommended to drink decoctions of chamomile, echinacea, and St. John's wort.