Rectal fissure is one of the common diseases of the rectum, which is localized in the inner part of the intestine in the anal area. This disease can occur for a variety of reasons and cause unpleasant symptoms in the sick person. Let us consider in more detail how to treat a rectal fissure at home and what needs to be done for this.
Causes of the disease
Most often, a rectal fissure develops for the following reasons:
- A sharp disturbance of blood circulation in the anus. This is usually observed in patients who lead a sedentary lifestyle and do not exercise at all. In such people, blood gradually stagnates in the pelvis, which first provokes inflammation of the mucous membrane, and then the development of a crack in the intestine.
- Frequent constipation or, conversely, digestive disorders can seriously injure the intestines and give rise to the appearance of cracks.
- Postpartum injuries very often cause fissures in the intestine. This is explained by the fact that during childbirth, a woman greatly overstrains the birth canal, which leads to the formation of a crack. Moreover, the situation becomes more complicated if, even during pregnancy, the expectant mother often suffers from constipation.
- Anal sex, which leads to intestinal injury.
- Hemorrhoids (link), which are not treated on time, contribute to poor circulation. This in turn weakens the anus and makes it more vulnerable to injury and subsequent fissures.
- Various disorders in the central nervous system (stress, neuroses, depression, etc.) can disrupt the functions of the sphincter and lead to its spasms. In this condition, a rectal fissure is a pattern.
Important! In more than half of the cases, the unstable psycho-emotional state of the patient can lead to exacerbation of chronic diseases, as well as the development of ulcers, pancreatitis and other diseases. Moreover, frequent experiences lead to exhaustion of the body and weakened immunity, so a person becomes more vulnerable to various types of pathologies.
- The anatomical features of the structure of the rectum in some cases make it prone to the appearance of cracks.
- Improper administration of an enema can easily lead to severe injury to the intestine, infection and the appearance of a crack.
- Lifting weights, which led to a sharp increase in intraintestinal pressure and gave impetus to the appearance of a fissure.
- Impaired tissue nutrition in the rectal area.
- Smoking and frequent drinking of alcoholic beverages cannot directly affect the formation of a crack, but it makes a person predisposed to this disease.
- Poor nutrition (eating too spicy, fatty, fried foods) can irritate the rectal cavity, which makes it vulnerable and easily injured.
Causes of rectal fissures
Mechanical factors
- Damage to the mucous membrane of the anorectal area during the passage of dense feces. Due to infrequent bowel movements with chronic constipation, the contents of the intestine stagnate and become hard. When emptying, the rectal canal is severely injured and tears form.
- Irritation of the anus due to frequent loose stools. Occurs with repeated diarrhea associated with irritable bowel syndrome or intolerance to certain foods.
- Compression of the perineal muscles during pregnancy. An enlarged uterus disrupts the normal blood supply and innervation of the rectum. The mucous membrane is easily damaged.
- Muscle stretching and overstrain of the walls of the rectal canal during physiological childbirth.
- Injury to the anus during medical procedures. When conducting diagnostic studies (colonoscopy, sigmoidoscopy, anoscopy) or therapeutic procedures (enema, gas tube), the mucous membrane of the anorectal area may be damaged.
- Entry of foreign bodies or undigested food components into the intestines. Children can swallow small parts of construction toys, buttons, coins, and more. These foreign objects damage the mucous layer of the rectal canal during defecation. Eating berries and fruits with large seeds, sunflower or pumpkin seeds with shells, fish with a ridge, etc. contributes to the formation of anal tears. Undigested food components transit through the digestive tract and, when released with feces, injure the mucous membrane of the anus.
- Anal sex.
Inflammatory factors
- Haemorrhoids. Due to impaired blood circulation and stagnation of blood in the pelvic organs, the walls of the rectal canal become weak. Hemorrhoidal veins and the rectal mucosa become inflamed and damaged when passing stool.
- Muscle spasm of the anal sphincter. Occurs with injuries, diseases of the rectum and anus, as well as in people with neurological symptoms. Accompanied by increased muscle tone. Patients deliberately prevent the act of defecation due to severe bursting pain in the anal ring. This causes constipation and hardening of stool. The process becomes chronic with increased vulnerability of the rectal mucosa.
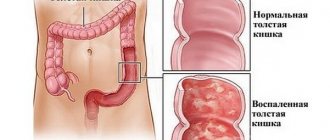
- Diseases of the digestive system (gastritis, cholecystitis, proctitis, nonspecific ulcerative colitis, etc.). They cause impaired digestion, poor peristalsis, improper motility and evacuation of intestinal contents. Gastrointestinal distress can cause chronic constipation or diarrhea. With constant irritation of the rectal mucosa by hard or liquid stool, erosive and ulcerative defects are formed.
- Worm infestations. More common in children. During enterobiasis, female pinworms lay eggs in the perianal folds. This causes severe itching. When scratching, the anal mucosa is injured, causing swelling and inflammation. Anal tears may form during bowel movements.
Other factors
- Sedentary lifestyle or excessive exercise. Physical inactivity and constant lifting of weights lead to hemorrhoids, which often cause rectal fissures.
- Weakness of the muscles of the pelvic organs. May be associated with the period of pregnancy and childbirth. It also occurs due to frequent inflammation of the genitourinary organs and rectum. Excess weight, lack of normal physical activity, and hereditary predisposition provoke the development of this problem. Infectious processes occur in the pelvis. They are accompanied by unpleasant symptoms – urinary or fecal incontinence (encopresis). Irritation of the anal area by biological secretions leads to its inflammation. Anal fissures form.
- Uncontrolled use of laxatives for the purpose of losing weight or normalizing stool for constipation. Constant diarrhea injures the mucous membrane of the lower intestines.
Be sure to read: Rectal cancer: symptoms, stages, treatment and prognosis for life
Features of the forms of intestinal fissures
A crack in the rectal mucosa has two forms of occurrence: acute and chronic. Each of these forms is characterized by its own characteristics.
The acute form of the disease usually develops spontaneously due to intestinal rupture. In this case, the patient experiences severe acute symptoms. His condition is rapidly deteriorating.
As a rule, the acute form of cracks goes away just as quickly. On average, the healing time for an injured intestine is 3-5 days.
The chronic form of intestinal fissure is considered much more serious. It can last for months without causing too severe symptoms in the patient. Occasionally, the pathology will worsen and make itself felt.
The main danger of this condition is that it can lead to serious complications, because a person will develop inflammation in the body for a long time, and the intestine will become increasingly affected by microbes.
Alternative treatment for rectal fissures
With regular use and the right approach, folk treatment for rectal fissures is very effective. In fact, folk remedies are actively used to treat rectal fissures and in traditional medicine. Medicinal herbs in various forms are very effective - in the form of pastes, decoctions, infusions, baths, enemas, and also in the form of medicinal tea. For topical use, chamomile, sage, oak bark, and yarrow are used. Aloe and Kalanchoe juice are used in the form of microenemas. For a general effect on the gastrointestinal tract, medicinal tea made from chamomile, sage, and St. John's wort is consumed.
Alternative treatment for rectal fissures can be successfully combined with the use of pharmaceuticals, allowing to reduce the drug load on the body, which is especially important in chronic forms of the disease.
Video from YouTube on the topic of the article:
Features of symptoms
The acute form of rectal fissure has the following features and symptoms:
- At the very beginning of the disease, the intestinal mucous layer is torn. This leads to sharp pain. Over time, the torn edges of the wound become rougher. The width of the crack increases, affecting the intestine even more.
- Due to the physiological ability of the intestine, it quickly closes and the crack is covered with a small film, but with subsequent constipation, the wound opens again and bleeds.
- A patient in the acute form of the disease experiences severe itching and burning in the anus. There may also be pain radiating to the perineum and rectum.
- If an infection is attached to the crack, the pain may become permanent. An elevated temperature and all signs of intoxication of the body (loss of appetite, chills, headache, weakness) may also be observed. In addition, infection of the wound can lead to the development of a fistula.
- The appearance of scarlet blood during defecation indicates injury to the capillaries in the rectal area. If dark blood appears, this indicates damage to the veins. Such bleeding will be similar to hemorrhoidal bleeding.
Chronic cracks usually have the following characteristics:
- A person weakens and his immunity decreases due to frequent blood loss. The patient may lose weight and be malnourished.
- Women experience menstrual irregularities and pain when urinating.
- Perineal pain may occur.
- Attacks of angina and arrhythmia often develop.
- It is difficult and painful for a person to sit in one position for a long time.
- The patient experiences irritability and fear of defecation.
- In addition to blood, pus may be discharged from the anus.
Causes of anal fissures
The etiology of the development of anal fissures in men and women is the increased tone of the circular muscles. The development of the defect can be triggered by:
- frequent, regular bowel movements;
- anal sex;
- traumatic damage to the mucous membrane during defecation;
- the process of obstetrics: pushing and childbirth itself, which often lead to ruptures of the mucous membrane;
- the presence of hemorrhoids;
- traumatic injuries from foreign objects: enema, proctological instrument or adult toys;
- sedentary lifestyle;
- lifting heavy weights or exerting yourself excessively;
- frequent consumption of alcoholic beverages or spicy foods;
- disorders in the functioning of the cardiovascular system and pathological conditions that are associated with them: thrombophlebitis, vasculitis, inflammatory processes of the colon, etc.;
- pathological conditions of the upper gastrointestinal tract.
Symptoms during pregnancy
Due to the physiological structure of internal organs, women are more predisposed to problems with stool. Moreover, this statistic increases when a woman is pregnant.
The appearance of a crack during pregnancy can be explained by the following:
- An enlarged uterus causes compression of the veins in the pelvic area, which leads to poor circulation in the rectum.
- Due to the influence of hormones that are produced during pregnancy, tissue swelling develops, which leads to increased susceptibility of the intestines to negative influences.
- If a pregnant woman eats improperly, her digestion is disrupted. This leads to the problem of constipation and its direct consequence – anal fissure.
Symptoms of a fissure in the intestine during pregnancy will be:
- Feeling of fullness in the lower abdomen. Another reason is rectocele.
- Pain and burning in the anus.
- Sharp spasms during bowel movements.
- The appearance of a small amount of blood during bowel movements, which does not mix with feces.
- Frequent constipation.
- Urinary dysfunction.
Symptoms
The following types of symptoms inherent in this disease are distinguished:
- Sitting or walking for a long time causes itching in the perineum, which cannot be tolerated.
- During defecation, a strong and sharp pain is felt, which quickly passes.
- There is a slight discharge of scarlet blood.
- In response to constant pain, frequent constipation occurs.
If such symptoms appear, you must immediately consult a doctor to prevent the development of this problem and begin treatment on time.
Diagnostics
When the first alarming symptoms of the disease appear, you should immediately contact a proctologist. Women are also recommended to undergo additional examination by a supervising physician and gynecologist.
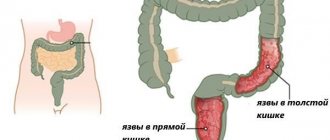
After collecting anamnesis, the doctor will conduct a digital examination of the rectum. Externally, the crack appears as a long red ulcer. It can be detected during anoscopy or rectomanoscopy.
To further confirm the diagnosis, the patient is recommended to undergo general clinical blood and urine tests to determine whether there is inflammation in the body.
Treatment
Treatment for rectal fissure is selected for each patient individually, depending on the cause of the pathology, symptoms and general neglect of the disease.
Traditional drug therapy includes the following:
- Prescribing painkillers to the patient in the form of oral tablets and ointments for local application.
- Antispasmodics (No-shpa) are prescribed for spasms.
- At elevated temperatures, the patient needs to take antipyretic drugs (Paracetamol).
- To facilitate bowel movements and normalize stool, laxatives are prescribed.
- It is very useful to use rectal suppositories based on oils. They will soften the intestine, help reduce pain and heal the fissure. The following drugs of this drug group are usually prescribed:
- candles with sea buckthorn oil;
- Proctosan;
- Relief Advance;
- Posterizan (ointment and suppositories).
In addition, glycerin suppositories have an excellent healing effect. They can be used not only for the treatment of adults, but also for therapy in children.
- If the intestine is infected and pus is discharged, the patient is prescribed strong antibiotics. They must be taken for at least ten days in a row. The dosage and name of the medicine is selected individually depending on the causative agent of the infection.
- When treated with antibiotics, the patient must be prescribed drugs to restore microflora and improve digestion. The best drugs in this group are Mezim, Hilak Forte, Linex.
- If stress is the cause of the crack, the patient should be prescribed antidepressants.
Important! If a patient with a fissure in the rectum is pregnant, then most oral medications are contraindicated for her to take. In this case, rectal pain relievers and healing ointments based on herbs and oils are usually used.
In addition to drug therapy, treatment of this disease involves a number of procedures. The best of them are:
- Daily use of microenemas with a weak solution of potassium and oils.
- Using beeswax based candles.
- Performing cleansing microenemas.
- Carrying out sitz baths. To prepare them, you need to pour warm water into a basin and dissolve potassium permanganate in it to get a pink color. Next, the patient should squat down so that the anal passage can be completely washed in the medicinal solution. The duration of this procedure is fifteen minutes.
In addition to potassium permanganate, you can also use medicinal decoctions of herbs that have anti-inflammatory and analgesic effects (chamomile).
It is best to perform sitz baths after a cleansing enema before bed.
Treatment of rectal fissure
Treatment of rectal fissures begins with the use of drug therapy, and if it is unsuccessful, surgical intervention is resorted to.
Drug treatment of rectal fissures includes the following measures:
- Ensuring regular soft stools, which is achieved by prescribing a dairy-vegetable diet with a sufficient amount of fiber, as well as prescribing enemas. Enemas are carried out daily with a weak antiseptic solution, usually decoctions of medicinal herbs are used for this purpose;
- The use of painkillers and anti-inflammatory drugs in the form of rectal suppositories, microenemas and warm baths, and in severe cases, injections directly into the area of the crack;
- Since in most patients rectal fissures are combined with other diseases of the gastrointestinal tract, treatment of the underlying pathology is necessary.
In most cases, treatment of rectal fissures with conservative methods is successful. However, in some cases, usually in chronic forms of the disease, accompanied by significant growths of granulation and scar tissue, more radical measures are necessary, then they resort to rectal fissure surgery.
Currently, rectal fissure surgery is performed using minimally invasive methods - laser coagulation or cryodestruction. These are bloodless techniques that do not require general anesthesia and a long hospital stay.
In persistent cases, as well as with large defects, they resort to the classic rectal fissure operation. The operation is performed under general anesthesia and consists of dissecting the sphincter, excision of the edges of the fissure and subsequent suturing of the edges of the wound. In the postoperative period, local anti-inflammatory therapy is prescribed for a month. It is also necessary to follow a diet that prevents the formation of dense feces.
Surgical and hardware treatment
If after two weeks drug therapy has not improved and the patient’s condition remains as acute, he is prescribed surgical treatment. This operation involves partial excision of the intestine and removal of the fissure.
This surgical intervention is performed under general anesthesia, so the patient does not feel pain during it. The person regains consciousness when the procedure is completed.
The duration of wound recovery and healing is usually 2-3 weeks. During this time, the person is advised to completely limit physical activity and maintain bed rest.
Most often, such surgical procedures are performed on patients with a chronic form of fissure, which is difficult to respond to drug therapy.
You should be aware that fissure removal does not always involve traditional open surgery. Modern medicine does not stand still and new treatment methods are already being actively practiced.
For example, an operation called lateral sphincterotomy, as well as an infrared coagulator, is considered very effective.
Prevention of anal fissures
Preventive measures aimed at preventing the development of anal fissures are as follows:
- A balanced diet that excludes the development of stool disorders;
- Regular hygiene procedures;
- An active lifestyle in order to eliminate congestion in the pelvic area;
- Consume at least two liters of fluid per day;
- Using soft toilet paper;
- Avoiding excessive physical activity;
If you notice symptoms indicating the possible development of an anal fissure, do not delay your visit to the proctologist. You can make an appointment with a specialist at the Doctor Nearby clinic by filling out the online form in this section of our website or by calling us by phone.
Medical nutrition
One of the most important roles in the treatment of rectal fissures is proper nutrition. The diet requires compliance with the following mandatory rules:
- Alcohol and sweet carbonated drinks should be completely excluded from the diet.
- It is necessary to enrich the menu with products containing fiber (vegetables and fruits). It will improve bowel function and soften stool.
- Dried apricots, raisins, prunes and other dried fruits, as well as decoctions from them, will help improve bowel movements.
- It is important to completely exclude the following products from the menu:
- fat;
- roast;
- salt;
- sugar and confectionery;
- White cabbage;
- beans;
- fast food;
- semi-finished products;
- potato;
- bakery products (only biscuits are allowed).
- The basis of the menu should be steamed or boiled dishes. At the same time, you should also give preference to homemade food rather than store-bought semi-finished products.
Important! Often people are unable to eat normally during working hours, so they satisfy their hunger with coffee and various sweets. If you have a rectal fissure, such a diet is extremely harmful. The way out of this situation can be homemade meals that need to be packed in convenient lunch boxes. They will not only be able to saturate a person with healthy food, but will also keep it fresh.
- The patient's menu should include low-fat fermented milk products (cottage cheese, sour cream, kefir) every day. They will improve digestion.
- It is recommended that the patient eat frequently, but the portions should be small.
- Do not eat too hot or cold food.
- It is important to avoid overeating so as not to complicate digestion and bowel movements.
- If you have a problem with constipation, it is recommended to further enrich your diet with vegetable fats (olive or sunflower oil).
Diagnosis of rectal fissure
If there are characteristic symptoms of a rectal fissure, an examination of the anus is performed, and a digital examination of the rectum is also used. Due to the significant pain and possibility of infection of the perirectal area, they try not to use retromanoscopy in this case, and in case of urgent need (for example, if a rectal tumor is suspected), anesthesia is first used.
Inspection makes it possible to detect a linear defect of the mucous membrane with smooth edges in case of an acute rectal fissure, and in case of a chronic one - an oval or triangular defect, with overgrown granulations and scar tissue.
Additionally, laboratory tests of blood (for HIV, syphilis, hepatitis, blood sugar and general analysis) and stool are carried out. In case of a rectal fissure in children, the stool must be examined for worm eggs.
Possible complications
In the absence of timely diagnosis and treatment, the patient may develop the following complications:
- Bleeding. At first it will be minimal and occur only after defecation, but over time the loss of blood will become more abundant. This in turn can lead to anemia, dizziness, weakness and headaches.
- The development of paraproctitis is associated with infection entering the deep layers of the intestine.
- Intestinal inflammation.
- The entry of pathogenic bacteria, which will lead to an abscess and suppuration.
- Sometimes the infection spreads to the prostate gland, which threatens the development of prostatitis in men.
- Chronic pain that will manifest itself not only during bowel movements, but also during physical activity and sitting.
- The spread of a crack along the intestine can lead to a sharp deterioration in the patient’s well-being and the penetration of feces into the intestinal cavity. This, in turn, threatens serious infection and intoxication of the body. This condition requires immediate surgical treatment.
Diet for intestinal fissures
As soon as the disease begins to be treated, the patient must immediately begin to adhere to a strict diet. Ideally, start doing this only if you suspect such an illness. In this case, the patient’s diet should consist exclusively of products that help soften the stool. Ideally, if the stool is even close to liquid. It is necessary to completely exclude from the diet foods that can cause constipation (rice, potatoes).
It is best to include in your diet during treatment and recovery period:
- dairy products. It is especially worth focusing on fermented milk products (kefir, yoghurt);
- oatmeal;
- foods rich in fiber;
- plums, apricots, pears.
You also need to drink as much fluid as possible. Ideally, of course, if it is water without gas. Since soda and mineral water can cause excessive flatulence, which in this case will put additional stress on the anus.
Smoked, fried, fatty, salty foods should also be consumed in minimal quantities - this puts additional stress on the intestines, and also leads to even greater irritation of the already inflamed mucous membrane.