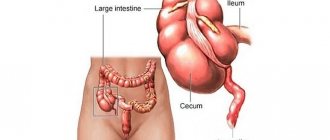
Gangrenous appendicitis is the penultimate stage of acute purulent appendicitis, in which necrosis of the wall of the intestinal appendix develops. The consequences of such a disease are very dangerous, especially for children: a perforation of the wall and a breakthrough of pus into the abdominal cavity may occur.
Symptoms for gangrene of appendicitis differ markedly from other types of this disease. Therefore, it is especially important to assess the danger in a timely manner and consult a doctor in order to immediately begin comprehensive treatment.
Gangrenous appendicitis causes
Acute appendicitis in its development goes through several stages and is divided into catarrhal and purulent (phlegmonous, gangrenous and perforated). In most cases, they speak of secondary gangrenous appendicitis - it occurs on the 2-3rd day of illness in the absence of medical care, in rare cases - after 6-12 hours. In children, gangrene of the appendix develops especially quickly.
In rare cases, the medical history records the primary type of purulent inflammation of the appendix. The following reasons can provoke this form of the disease:
- Damage to the walls of blood vessels in old age.
- Atherosclerosis of the intestinal arteries (cholesterol plaques on the walls).
- Congenital underdevelopment (hypoplasia) of the appendicular arteries in children.
- Thrombosis of the veins and arteries of the cecum.
Vascular problems cause circulatory problems, resulting in death of appendix tissue. Acute purulent appendicitis can also be accelerated by reasons such as various infections and autoimmune processes in the intestines.
Symptoms
Acute appendicitis in the gangrenous stage will be characterized by a special clinical picture. The perforated type of the disease increases the intoxication of the body, more and more decay products are released into the blood (the tissue dies and releases toxins). The following symptoms appear:
- Loss of appetite and inability to appreciate the appearance of food.
- The patient is constantly shivering.
- Body temperature increases, the thermometer shows 39 degrees. It is worth noting that this does not always happen.
- State of nausea and vomiting.
- The patient's stool is disturbed. Periods of constipation may be followed by periods of diarrhea.
- In the oral cavity, a white, yellow or brown coating appears on the tongue. The color change is noticeable near the root.
- More gases are produced in the intestines, and the stomach becomes hard.
- The patient feels weakness throughout the body and loss of strength.
- Dry mouth.
- The pulse quickens and reaches 120 beats in one minute.
- Young patients exhibit lethargy, moodiness, and tearfulness.
There comes a period when the patient feels that he is better, but this is only temporary relief, which is a false indicator of recovery. This means that along with the tissues of the appendix, the nerve endings responsible for pain also die.
Gangrenous appendicitis symptoms
The main difference between appendicitis gangrene and other forms of the disease is that many patients do not feel severe abdominal pain. The reasons are tissue necrosis and subsequent death of nerve cells of the appendix. In such cases, the medical history reflects symptoms such as mild pain throughout the abdomen, softness of the abdomen on palpation, absence of peritoneal irritation, and normal temperature.
The main symptoms of gangrenous appendicitis are:
- Severe pain in the right iliac region gradually subsides.
- Vomiting (from one-time to prolonged, which only torments the patient and does not bring relief).
- Normal or slightly reduced temperature in the general serious condition of the patient.
- Against the background of a normal temperature of 36.6º, there is a strong tachycardia of 100-120 beats per minute (this phenomenon is called “toxic scissors” syndrome).
- Dry mouth, white or yellowish coating on the tongue.
Signs of a dangerous stage
This stage of appendicitis does not occur immediately, but 2-3 days after the first signs of the disease appear. During this period, signs of phlegmonous-gangrenous changes in the tissues of the organ appear. Lack of therapy leads to deterioration of the patient's condition and the development of complications. The inflamed organ changes, the outer walls collapse and die. During the operation, the smell of rot comes from the wound.
The appearance of the process has characteristic features of the last stage:
- Significant increase in size;
- The color of the appendix has changed to a dirty green hue;
- Areas of blood are observed;
- Tissue necrosis is visible;
- Sources of pus leakage.
Risk to internal organs
The danger of acute damage to the appendix is that it affects internal organs located close to the appendix. In particular, inflammation affects organs located in the abdominal cavity. If medical assistance is not received, gangrenous appendicitis turns into a gangrenous-perforated disease, the wall of the organ becomes perforated, and pus leaks out.
Features of gangrenous-perforated appendicitis
Gangrenous perforated appendicitis is the final stage of acute inflammation of the appendix. In this form, one of the walls (or several) of the intestinal appendix ruptures and purulent release of the contents into the peritoneum.
The medical history of perforation of the appendix usually records sharp pain at the time of rupture of the appendix and the spread of pain over the entire surface of the abdomen. The temperature increases sharply, the abdomen is swollen and very tense, there is no stool completely. The vomiting almost never stops, and the coating on the tongue turns brown.
The only treatment for this diagnosis is surgery; in case of the slightest delay, perforated appendicitis can result in diffuse peritonitis, with a more favorable outcome - in an appendiceal abscess. In addition, purulent discharge into the abdominal cavity sharply increases the risk of complications after surgery - from wound infection to purulent peritonitis.
Consequences of the condition
Due to gangrenous inflammation, the appendix is filled with pus. When the signs of appendicitis do not cause discomfort, the disease progresses to the outpouring of exudate into the peritoneum with perforation of the appendix wall.
In some cases, peritonitis is localized. This happens when adhesions form on the tissues of the appendix. This allows the putrefactive contents not to spread.
When the gangrenous form is complicated by peritonitis, the symptoms change. The pain syndrome is not located in one place, but spreads throughout the abdomen. At the same time, additional signs of the consequences of untimely assistance are noted.
The course of gangrenous-perforated appendicitis is characterized by a decrease or absence of intestinal motility. Additionally, abdominal tension and signs of peritoneal irritation are observed.
Gangrenous appendicitis diagnosis
The main difficulties in diagnosing gangrene of appendicitis in adults and children are associated with atypical symptoms of the disease. The absence of pain, a soft abdomen, and normal temperature often mislead the doctor, and he believes that there is no reason for hospitalization. Upon re-application, the patient is already diagnosed with gangrenous lesions of the appendix, and immediate surgical intervention is required to prevent dangerous complications.
All forms of appendicitis - acute catarrhal, purulent phlegmonous, and gangrenous with suspected perforation - require special diagnostic methods:
- Conversation with the patient and collection of anamnesis (symptoms are recorded by the medical history).
- Careful sequential palpation of the abdomen (you need to act especially carefully in case of appendicitis in children).
- Urine and blood tests.
- X-ray and ultrasound of the abdominal cavity.
- CT scan.
- Laparoscopy (examination using a miniature camera).
One of the most crucial moments in diagnosis for gangrene of appendicitis is palpation. Gangrenous lesions are usually difficult to detect due to the almost complete absence of pain and irritation of the peritoneum. In this case, it is necessary to especially carefully examine the muscles of the right and left iliac region, so that if there is the slightest difference in their condition, the patient can be referred for x-rays and other studies.
Reasons for the development of the condition
Gangrenous appendicitis is directly associated with the algorithm for the formation of the inflammatory process in the area of the appendix. Mostly we are talking about a long duration of the condition. The main risk factors in terms of the development of primary gangrenous algorithm should be considered:
- advanced age and associated changes in the structure and structure of blood vessels;
- childhood and genetically determined hypoplasia (displacement) of arteries in the appendix area;
- atherosclerotic damage to the arterial walls in the intestinal area;
- the formation of blood clots in the arteries and veins of the appendix.
The presented data fully indicate that the direct causes of the acutely formed condition are precisely those disorders that are associated with microcirculatory functions. Their result should be considered destabilization of the blood circulation process in the process itself and, as a consequence, its necrosis (the appearance of necrotic tissue). All remaining “chains” of development, namely infectious lesions, destabilization of the outflow of contents from the appendix and much more, will be added subsequently, only aggravating the overall course of the process, provoking complications and negative symptoms.
It also happens that the main factor in the development of such a condition as gangrenous appendicitis is the transformation of simple forms of appendicitis into destructive ones. This can happen mainly due to incorrect or late initiation of surgical treatment. In such a situation, the appendix will be subject to purulent melting when the patient has to stay in the hospital after surgery, which takes a long period of time.
Development of appendicular infiltrate and its treatment
Gangrenous appendicitis treatment
Gangrenous appendicitis, like acute phlegmonous, requires a single treatment method - surgical removal of the inflamed intestinal appendix (appendectomy).
Treatment of gangrene of appendicitis includes preparation for surgery (no more than 2 hours), the operation itself and postoperative recovery. During the operation, the surgeon removes the purulent appendix and cleanses the abdominal cavity of purulent fluid.
The main types of surgery for gangrenous appendicitis are traditional appendectomy and laparoscopy.
In a classic operation, the surgeon makes a 9-12 cm incision, removes the damaged appendix into the wound (along with the cecum), removes and sutures the cecum. Then he sanitizes the abdominal cavity from pus and leaves a drainage tube.
Laparoscopy is the removal of the intestinal appendix through 2-3 small holes using special modern equipment. What is especially important is that during such a procedure the surgeon has the opportunity to monitor the progress of the operation on a special monitor. For gangrene of appendicitis, laparoscopy is more preferable: the medical history records complications after such an operation 2-4 times less often than with traditional appendectomy.
Treatment of acute appendicitis
Acute gangrenous appendicitis is treated surgically. For pain relief, local anesthesia or general anesthesia is used. In advanced cases with the development of peritonitis, doctors use endotrichial anesthesia with ventilation.
Appendectomy involves two types of surgical intervention: traditional and laparoscopic.
Traditional appendectomy
The preparatory stage for the operation lasts no more than two hours. It includes the collection of blood and urine tests, as well as a number of diagnostic procedures:
- Ultrasound.
- CT scan.
- Rectoscopy.
- Visit to the radiologist.
- For women – consultation with a gynecologist.
- ECG for heart problems.
After the tests are collected, the patient is prepared for surgery. Held:
- Bladder catheterization.
- Shaving the abdominal wall.
- Disinfecting the skin with an antiseptic.
Surgery to remove appendicitis
The operation is performed through an incision in the iliac zone on the right. The cecum is pulled out and the appendix is excised. After this, doctors suture or drain the wound. Inflammatory fluid is removed from the peritoneal cavity using an electric suction device and wipes.
In some cases, surgeons leave drainage - gauze swabs - in the abdominal cavity. This happens if:
- The appendicitis was not completely excised.
- Despite all measures, bleeding continues from the excision site.
- An abscess has opened and the pus needs to be drained.
- An infiltrate has been detected and removal of the appendage is impossible.
Video of appendectomy
Laparoscopy
A progressive method of surgical intervention, which is performed with a laparoscope and special surgical instruments. A laparoscope is a flexible tube with a video camera and lighting. With its help, the surgeon looks into the most remote places of the peritoneum and examines the organs from all sides. If necessary, organs are examined using a laparoscope before surgery.
Removing appendicitis using a laparoscope
Advantages of laparoscopy compared to traditional resection of appendicitis:
- Less tissue is injured.
- Wounds heal faster after surgery.
- The recovery period is halved.
- Minimal risk of complications.
- Scars after laparoscopy are almost invisible.
The disadvantages of laparoscopy are high cost and individual contraindications to surgery. In rare cases, due to equipment malfunction, unforeseen consequences occur: intestinal burns and damage to adjacent organs.
Video of laparoscopic appendectomy
Recovery after surgery for gangrenous appendicitis
After gangrenous inflammation of the appendix, particularly careful recovery after surgery is necessary, especially for the elderly and children. Comprehensive treatment and strict adherence to medical recommendations will prevent complications and speed up recovery.
The main therapeutic methods after removal of purulent appendicitis are:
- Taking antibiotics of various groups (ornidazole, cephalosporins, amikacin).
- Painkillers.
- Powerful detoxification treatment (plasma, saline solutions, glucose, etc.).
- Daily blood tests to identify any possible complications in time.
- Regular dressings (changing the dressing, washing the drainage tube and scar). Helps prevent suppuration and infection of the suture.
- Prevention of ulcers and blood clots (anticoagulants, gastric secretion blockers, elastic bandages).
- Breathing exercises and physical therapy. They help avoid complications such as intestinal obstruction, as well as cardiovascular and respiratory problems after appendectomy.
Diagnostics
Establishing the correct diagnosis can be quite difficult, for the reason that gangrenous appendicitis, in most cases, is a secondary disease. It is because of this that it is necessary to carry out a whole range of diagnostic measures.
Primary diagnosis includes:
- performing a detailed survey of the patient regarding the time of onset and degree of intensity of symptom expression;
- a doctor’s examination of the patient’s medical history and life history to identify the sources of the disease;
- conducting a physical examination with mandatory palpation of the abdomen.
The second step in establishing the correct diagnosis is conducting a laboratory examination:
- general and biochemical blood test - to detect an increased level of leukocytes, an increase in ESR and acute phase indicators;
- general urine test - to detect the presence of leukocytes and red blood cells, which should not normally be present;
- coprogram.
The last stage of diagnosis is instrumental examination of the patient, which involves performing:
- Ultrasound of the abdominal organs will provide information about the shape and condition of the appendix. The information content of such a procedure is reduced in the gangrenous-perforated form of the disease. This is due to the fact that the purulent contents of the appendix have penetrated into the peritoneum, causing its contours to be blurred;
- radiography and CT - to obtain more accurate information about the cecal appendage;
- Diagnostic laparoscopy is a procedure that is performed using endoscopic instruments to examine the internal surface of the gastrointestinal tract. It indicates thickening of the appendix, its greenish tint and tissue necrosis.
Diet after gangrenous appendicitis
Treatment of any form of inflammation of the intestinal appendix includes a gentle diet for the first month and a half. If acute purulent appendicitis is accompanied by any complications, you need to select a therapeutic diet especially carefully - the food should promote recovery and not irritate the diseased intestines.
The basic rules of the diet for gangrene of appendicitis are to eat 5-6 times a day in small portions; dishes should not be hot or cold; All intestinal irritants are prohibited: alcohol, factory-made sweets, preservatives, flavorings, spices, everything fried and smoked.
Treatment
Treatment of gangrenous appendicitis is carried out only after a complete diagnosis of the patient. It includes the following steps:
- External examination of the patient.
- Palpation of the abdominal cavity. The doctor needs to be extremely careful; one wrong movement and strong pressure on the muscles can cause the appendix to rupture.
- Blood analysis. If the number of leukocytes increases (several times), the diagnosis is confirmed.
- Analysis of urine. Protein may appear.
- Ultrasound. If tissue necrosis occurs, the appendix is not clearly visible.
It is important! Examination by one therapist will not be enough. You should definitely consult a surgeon. If the symptoms increase, the patient becomes worse, you need to call an ambulance and immediately go to the hospital.
Gangrenous appendicitis is not treated with medication; the only way is to remove the appendix.
Gangrenous appendicitis: complications after surgery
If it is possible to identify and operate on gangrene of appendicitis before perforation of the intestinal appendix, then the possibility of dangerous consequences occurring is minimal. The most common complications in this case are infection and suppuration of the suture after appendectomy. They are easy to treat and do not require repeated surgery.
If the patient went to the doctor too late or the history of the disease led to a ruptured appendix, the consequences can be much more severe:
- A breakthrough in the wall of the intestinal appendix with the release of pus and feces into the peritoneal cavity.
- Self-amputation of the appendix (complete separation from the cecum).
- Multiple local abscesses in the pelvic area, under the diaphragm or in the intestines.
- Appendicular infiltrate (accumulation of inflamed processes around the appendix). The only contraindication to surgery is that removal of the appendix is possible only after 3-4 months, after complete resorption of the infiltrate.
- Purulent peritonitis. It poses a threat to the patient's life and requires immediate surgery.
- Septic thrombophlebitis.
Gangrenous appendicitis is the most insidious type of acute appendicitis, which can lead to serious problems if misdiagnosed. The most common consequence of this disease is rupture of the appendix followed by an abscess or peritonitis. Knowledge of all the symptoms of this disease, the ability to suspect a dangerous diagnosis in time and immediate surgery will allow you to avoid all complications of appendix gangrene and bring recovery as close as possible.
Consequences
Lack of medical care in the event of gangrene of the appendix leads to a significant deterioration of the patient’s condition and the development of complications:
- Pylephlebitis develops inside. This means that the purulent inflammatory process provokes the formation of blood clots in the portal vein.
- The appearance of purulent sources in the peritoneal cavity. As a rule, the abscess is located between the intestines, in the area of the diaphragm and small pelvis.
- An infiltrate consisting of tissue begins to form around the appendix. Its formation prevents the spread of inflammation to other internal organs.
The most dangerous complication is the gangrenous form of peritonitis. This means that the walls of the appendix have ruptured. This development of the disease is fraught with blood poisoning. Surgeons try to prevent the onset of this stage, since the survival rate of patients is low.
Prevention
Specific preventive measures against the occurrence of such a disease are the timely elimination of acute appendicitis and other etiological factors, as well as regular medical examinations.
In the case of uncomplicated gangrenous appendicitis, the prognosis will be favorable, provided that adequate treatment is provided and the patient follows all the recommendations of the attending physician in the postoperative period.
The prognosis worsens significantly with the development of complications that can lead to death.
Rehabilitation
The duration and course of the postoperative period depends on the technique used to remove the appendix and the degree of complexity of the patient's condition. On the first day after the excision procedure, the patient is constantly monitored by a nurse. Her responsibilities include:
- monitor for symptoms of bleeding;
- control temperature;
- inspect the seam;
- question the person about the appearance of pain and appetite, monitor the need for bowel movements.
Those patients who had uncomplicated gangrenous appendicitis have good prognoses for these indicators. The postoperative period in the following days includes:
- taking antibiotics;
- anesthesia;
- infusion detoxification therapy;
- prevention of the occurrence of negative reactions of the body in people at risk (stress ulcers of the intestines and stomach, thromboembolic complications);
- daily blood sampling for tests;
- dressings;
- breathing exercises, physical therapy, massage.
Rehabilitation can last from one and a half weeks to a month. Young children and overweight people take longer to recover.
Treatment methods
Therapy involves surgical removal of the appendix. Appendectomy is performed traditionally or through laparoscopy.
In the first case, the doctor removes the appendix through an incision in the abdominal wall. Typically, this procedure is performed using general anesthesia.
Surgery for appendicitis using laparoscopy is less traumatic. The surgeon makes several microscopic punctures in the abdominal wall through which instruments for manipulation are inserted. The most important of them is the laparoscope - a tube with a camera at the end. During the operation, the doctor receives an image from it on a computer screen, which allows for the most accurate surgical manipulations.
Possible complications
This pathology is considered very dangerous, as it can lead to the development of complications quite dangerous to health. This process is especially critical for young patients.
What negative consequences can be accompanied by gangrenous appendicitis?
- Purulent peritonitis. This is a rather dangerous condition that requires immediate surgical intervention. If help is not provided promptly, blood poisoning may occur.
- Appendicular infiltrate. In the area of the inflamed appendix, a local conglomerate gradually forms, consisting mainly of organs and tissues. This problem always requires long-term conservative therapy.
- Septic thrombophlebitis. The inflammatory process develops in the venous walls. As a result, it leads to the formation of blood clots in the lumen of the vein.
- Local purulent abscess. Such formations predominantly develop in the diaphragm area.
Appendicitis should not be ignored. The purulent gangrenous version of this pathology requires immediate treatment. Otherwise, the likelihood of complications and even death increases. Such inflammation is especially dangerous for children; all pathological processes occur several times faster in them.
Reasons for maintaining a fever for more than 10 days after appendicitis removal
It is important to remember that postoperative hyperthermia indicates inflammation in the body. A short fever does not pose a danger to the patient, because it is a protective reaction of the body traumatized by the operation. This fever does not require treatment or diagnosis.
Fever that lasts longer than 10 days and is accompanied by symptoms of:
- pain in the stomach;
- constipation;
- vomit;
- cold sweat;
- loss of consciousness.
Reasons why the temperature does not subside after surgery to remove appendicitis:
- Extensive blood loss. The body lost a lot of blood during the operation.
- The doctor injured the peritoneum. The organs adjacent to the appendicitis, touched by a surgical instrument, became inflamed.
- There was no sterility in the operating room. The wound became infected and caused local inflammation.
- Weakened immunity. The body was struck by a respiratory infection.
- Medical staff error. Suppuration occurred due to poor treatment and improper dressing of the surgical wound.
- There was drainage left in the wound. The surrounding tissues rejected the foreign body, and an immune reaction began, which caused hyperthermia.
- The patient broke his diet. Hard, fatty and spicy foods led to constipation and poisoned the body, which caused fever.
- A complication arose - peritonitis. After surgery on the purulent stage of the appendix, the patient's hyperthermia lasts for two to three weeks.
- Intoxication occurred due to the breakdown of tissue formed after the operation.
- The stitches were removed before the wound was completely healed and the wound became inflamed due to infection.
Diet
For the first half day after the operation, the patient can gradually drink still water or weak sweet tea; eating is prohibited. On the second day, the patient is given low-fat broth, liquid porridges and purees, and finely chopped boiled meat are gradually introduced into the diet.
In the following days, baked vegetables and fruits, fermented milk products, stewed or boiled fish dishes are carefully introduced into the diet. Be sure to drink clean water in an amount of at least 1.5 liters per day.
It is important to monitor not only the quality of your diet, but also adhere to the following recommendations for better absorption of food:
- meals should be fractional, the patient should be fed at least 5 times a day at regular intervals;
- food should only be warm; eating hot or cold foods is prohibited.
For the first six months after surgery, it is important to adhere to the principles of dietary nutrition and give preference to lean varieties of meat and fish, and the basis of the diet should be boiled, baked without oil or stewed dishes.
The above recommendations will help to gradually improve intestinal motility and relieve the patient from stool disorders and flatulence.
Recommended video:
What foods should you exclude from your diet?
During the postoperative period and until complete recovery, the patient is prohibited from consuming the following products:
- legumes;
- cabbage;
- carbonated drinks;
- alcohol;
- spices;
- ketchup and mayonnaise;
- fast food;
- salted, smoked, fried, spicy dishes;
- sweets;
- canned food;
- store-bought sausages;
- bread.
The products described above negatively affect the condition of the entire gastrointestinal tract and intestines, increase peristalsis and can lead to complications in the postoperative period.