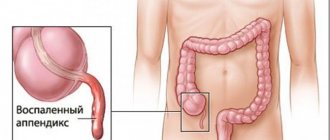
Chronic appendicitis is a rare form of sluggish inflammation of the appendix (appendix), which develops after an attack of acute appendicitis and is accompanied by atrophic and sclerotic changes in the wall of the appendix. The disease is more often detected in young women. It practically never occurs in children and older people.
Chronic appendicitis is more common in young women
Forms of the disease
There are three forms of chronic appendicitis:
- residual (residual) form - develops after a previous acute appendicitis, which ended in recovery without surgical intervention;
- primary chronic form - develops slowly, without a previous attack of acute appendicitis. Some experts question its presence, so the diagnosis of primary chronic appendicitis is made only after excluding the presence of any other pathology that can cause a similar clinical picture;
- relapsing form - characterized by recurrent symptoms of acute appendicitis in the patient, which subside after the disease goes into remission.
At any time, chronic appendicitis can turn into an acute form, and untimely surgical operation in this case threatens the development of peritonitis, a potentially life-threatening condition.
Causes
The first cases of surgery to remove appendicitis were described in the 1st century AD, although in Europe - only in the 17th. In women, inflammation of the appendix was mistaken for postpartum complications and was called “ uterine abscess.”
" The emergence of such a diagnosis was facilitated by the fact that appendicitis occurs much more often in women, and pregnancy provokes its occurrence. But this is one of the reasons for the development of an acute form of the disease, but what about the chronic form? After all, some experts do not define it at all.
There are many theories explaining the reasons for the development of acute appendicitis. It itself becomes the root cause of the chronic course, which is called the “cold period” of inflammation
. What happens in the process? The fibrous connective tissue of the appendix grows, and the mucous membrane and muscle layer die. The ulcerated mucosa is replaced by scar tissue, which gradually increases and narrows the lumen of the cecum, causing serous fluid, pus and mucus to accumulate here. The muscular layer atrophies, as do the muscular layers of blood vessels, and nerve nodes are destroyed. Adhesions immediately form, which cover the process and lead to its kinks.
This process can last several years, periodically exacerbating - this is its danger.
Classification of chronic form
Sometimes chronic inflammation of the appendix is diagnosed without signs of exacerbation. Although some experts deny this possibility, explaining that the pain arose in nearby organs. Although the fact remains: inflammation of the gallbladder and duodenal ulcer can affect the “well-being” of the appendix.
Therefore, supporters of the existence of chronic appendicitis classify it as follows:
- primary chronic appendicitis
- the disease is sluggish, abdominal pain occurs without exacerbation of the inflammatory process; - chronic recurrent
- develops after several attacks of acute appendicitis; - residual
- a residual phenomenon of acute attacks.
But it is quite difficult to correctly diagnose this form of the disease.
Why does it develop in women?
Why are women, especially pregnant women, at risk? This is explained by the structure of the female reproductive system, which is in close contact with the organs of the gastrointestinal tract. Inflammation from the uterus, ovaries and fallopian tubes quickly spreads to the appendix.
The appearance of inflammatory processes is facilitated by monthly menstruation, during which, under the influence of hormones, the mucous membranes swell and loosen. In pregnant women, the constantly increasing size of the uterus puts pressure on surrounding organs
, due to which their blood supply is disrupted - thus appendicitis is provoked, in acute or chronic form.
According to statistics, chronic appendicitis occurs in 1% of cases, most often in young women.
Causes and risk factors
The main reason for the development of chronic appendicitis is a slow-moving infectious inflammatory process in the appendix.
The development of primary chronic inflammation is facilitated by disturbances in the trophism and innervation of the appendix wall, which lead to a decrease in local immunity. As a result, microorganisms contained in the intestines provoke mild inflammation, which can last for many years, causing discomfort and pain in the right side of the abdomen. Under unfavorable conditions, a sluggish inflammatory process can be sharply activated, and then acute appendicitis develops.
The main cause of chronic appendicitis is a sluggish infectious process
Secondary chronic inflammation is the outcome of acute inflammation of the appendix. If, for one reason or another, surgical treatment of acute appendicitis has not been performed, very dense adhesions form in the appendix, reducing its lumen. This causes stagnation of intestinal contents in the appendix, which provokes a long-term inflammatory process of insignificant activity.
The recurrent form of chronic appendicitis can be caused by both primary and secondary chronic inflammation. Periods of exacerbation of the disease are provoked by various unfavorable factors (stress, hypothermia, acute infectious diseases), which reduce general immunity and thereby create the preconditions for increased activity of the inflammatory process in the appendix.
Recurrent chronic appendicitis in very rare cases develops after surgical removal of the appendix (appendectomy). This can happen if the surgeon left a portion of the appendix longer than 2 cm.
Symptoms
The clinical symptoms of the chronic stage of the inflammatory process in the appendix are similar to those of an acute attack, but have a sluggish appearance. Symptoms are not as active. The chronic stage is characterized by less severe attacks of pain and discomfort. The patient notes a rare, aching pain under the right rib, a feeling of heaviness that is constantly repeated after exercise in the form of sports, weight lifting, heavy physical labor, spicy or heavy food, and overeating.
Some patients note periodic bowel movements. Diarrhea can change into constipation and vice versa, the stomach often hurts from an increased level of gases, and the urge to nausea appears. But hyperthermia, a constant symptom of acute appendicitis, is not observed. In some cases, the temperature may rise in the evenings, but not always.
These sensations also occur after poor nutrition. A patient who does not follow a diet often experiences digestive disturbances, especially after eating rough food. At the same time, the chronic form of the disease is easily confused with intestinal inflammation. Differentiation in this disease is of great importance.
The malaise is also characterized by the presence of the following manifestations: frequent, sometimes painful urination; women experience pain in the gynecological part, this is especially evident when examined by a gynecologist through vaginal palpation. Patients experience discomfort during examination through the rectum, feel pain and unpleasant heaviness.
Diagnosing the disease in children is particularly difficult. Children, due to their age, cannot explain exactly the location of discomfort and pain in the abdomen. Moreover, the chronic form is more common in children than in adults, since sometimes in childhood, for a number of reasons, it is impossible to remove the appendix. Treatment is carried out with medication, as a result the disease becomes chronic. The inflammatory process may last for some time without symptoms, after which it manifests itself as pain, heaviness, diarrhea or constipation.
Symptoms of chronic appendicitis
The symptoms of chronic appendicitis are blurred, and sometimes may be completely absent (during periods of remission in the recurrent form). Typically, patients complain of periodically occurring aching dull pain in the right iliac region. The pain is of low intensity, but can intensify under the influence of gross errors in diet or intense physical activity.
The main symptom of chronic appendicitis is dull aching pain in the iliac region
Other symptoms of chronic appendicitis are:
- flatulence;
- constipation alternating with diarrhea;
- nausea;
- increase in body temperature in the evening to subfebrile values (37.1 – 37.9 °C).
In women, a symptom of chronic appendicitis is pain that occurs during mechanical action in the area of the uterine body, for example, during sexual intercourse or a gynecological examination using a vaginal speculum.
Pain that occurs during a rectal examination of the prostate gland may be a symptom of chronic appendicitis in men.
Chronic appendicitis may also be accompanied by the development of bladder manifestations - frequent and painful urination.
With exacerbation of chronic appendicitis, patients develop a clinical picture corresponding to acute appendicitis.
The first signs of appendicitis in adults, stages of disease development
Symptoms of appendicitis in adults, characteristic of the typical course of appendicitis, have a cyclical nature and manifestations corresponding to the progression of the pathological process. What are the first signs of appendicitis in adults?
Stage of catarrhal appendicitis (first twelve hours)
The typical picture of appendicitis begins with discomfort and pain in the stomach, often in the evening or at night. Very often, these pains resemble manifestations of gastritis and are not intense, dull in nature, so people do not attach much importance to them. During the same period, nausea sets in and vomiting occurs once. It is believed that nausea with appendicitis is of a reflex nature, and often in older people this symptom can be mild, which sometimes leads to a late diagnosis.
After a few hours, the pain moves to the lower right abdomen (if the appendix is located on the right side). The nature of the pain changes - it becomes pressing and pulsating with increasing intensity. Diarrhea may occur and urination may become more frequent. Low-grade fever occurs with a slight further increase in temperature above 37 C.
Gradually, within six to twelve hours from the onset of the disease, typical symptoms of general intoxication of the body develop - weakness, rapid heartbeat, dry mouth, malaise. The pain becomes unbearable and even more intense. The abdomen at this stage remains soft, but painful when pressed on the right side.
This stage is considered the most favorable for surgery, but most patients see a doctor later.
Stage of phlegmonous appendicitis (end of the first day)
During this period, the pain is clearly localized in the iliac region on the right, pulsating and intense in sensation. There is a constant feeling of nausea, tachycardia up to 90 beats per minute is observed. The temperature fluctuates around 38 C. When examining the abdomen, a lag on the right side in the process of breathing becomes noticeable. The abdomen becomes tense in the lower right part, which indicates the beginning of the transition of the inflammatory process to the peritoneum. At this stage, all diagnostic symptoms (slips, Shchetkin-Blumberg, Sitkovsky, Bartomier-Mikhelson, Rovzing) become positive and the diagnosis becomes obvious.
At this stage, the patient most often ends up on the operating table.
Stage of gangrenous appendicitis (second or third day)
At this stage, there is an imaginary pain relief - the nerve endings of the appendix die off, which leads to a decrease in sensitivity. At the same time, symptoms of general intoxication of the body increase - severe tachycardia appears, and vomiting is possible. The temperature drops, sometimes even below 36 C. The abdomen is swollen, there is no peristalsis. Palpation of the area where the appendix is located causes severe pain.
Stage of perforated appendicitis (end of the third day)
The moment of perforation of the appendix wall is accompanied by acute pain, localized in the right lower abdomen, with increasing intensity. There are no periods of relief, the pain is constant. Repeated vomiting occurs. The patient experiences severe tachycardia, the abdomen becomes swollen and tense, and peristalsis is completely absent. The white coating on the tongue turns brown. Body temperature rises to critical levels. The outcome of perforation of the appendix is purulent diffuse peritonitis or local abscess.
It is worth noting that the indicated timing and stages of progression of appendicitis are conditional - a latent or fulminant course of the disease is possible.
You can learn how to determine appendicitis in a child from our article Signs of appendicitis in children
Diagnosis of chronic appendicitis
Diagnosis of chronic appendicitis is quite difficult, since there are no objective clinical symptoms of the disease. Anamnesis data provide some assistance in diagnosis - the patient’s indication of one or more attacks of acute appendicitis.
Indirect signs of chronic appendicitis may be weakly positive (beyond exacerbation) symptoms of Sitkovsky, Rovzing, Obraztsov, as well as the presence of an area of local pain in the right iliac region.
Chronic appendicitis is more often detected in young women. It practically never occurs in children and older people.
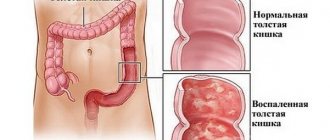
If chronic appendicitis is suspected, irrigoscopy (x-ray of the large intestine using contrast) is performed. The following changes are revealed:
- narrowing of the lumen and deformation of the appendix;
- incomplete filling of its lumen with contrast;
- delayed emptying (removal of contrast).
To exclude neoplasms in the colon and cecum, colonoscopy, as well as ultrasound scanning and plain radiography of the abdominal cavity are indicated.
Irrigoscopy and colonoscopy are used as a differential diagnosis of chronic appendicitis.
Laboratory diagnosis of chronic appendicitis is not very informative, since clinical tests of blood and urine usually do not reveal changes, or they are associated with some other pathology.
Differential diagnosis of chronic appendicitis is carried out with the following diseases:
- helminthic infestations;
- gynecological diseases;
- urinary tract diseases;
- colon tumors;
- ileotiphlitis and typhlitis;
- yersiniosis;
- abdominal ischemic disease;
- spastic colitis;
- chronic cholecystitis;
- irritable bowel syndrome;
- Crohn's disease;
- peptic ulcer of the stomach and duodenum.
Treatment of chronic appendicitis
If the diagnosis of chronic appendicitis is beyond doubt and the patient has persistent pain, an appendectomy is performed - an operation to remove the appendix using a laparoscopic or traditional (open) method.
If there is any doubt about the presence of chronic appendicitis, one should refrain from performing an appendectomy, since removal of the unchanged appendix in the future usually only aggravates the severity of the pain syndrome that served as the basis for surgical intervention.
An operation to remove the appendix is performed if the diagnosis of “chronic appendicitis” is beyond doubt
Treatment of chronic appendicitis with mild symptoms is conservative. Patients are prescribed antispasmodic and anti-inflammatory drugs, and physiotherapeutic procedures.
Treatment methods
Treatment of chronic appendicitis in a child or adult is based on medical history , patient complaints and the results of studies. Surgery is usually required.
Surgical intervention
With exacerbation of chronic appendicitis, they speak of an acute inflammatory process , which is why the only treatment method is surgery.
There are two ways to remove appendicitis:
- Open access . The surgery is performed by making an incision in the abdominal cavity. After the incision, the surgeon exposes the inflamed appendix, inspects nearby tissues, and excises pathologically altered areas. Then drainage tubes are installed into the incision, and the wound is sutured layer by layer. After 2-3 days it is sutured tightly. Complete rehabilitation takes several months; the patient is discharged from the hospital within 7-14 days.
- Laparoscopy . A minimally invasive, less traumatic method of surgical intervention, which allows for faster rehabilitation. After healing, only small punctures remain on the peritoneum. During the operation, several punctures or incisions are made in the peritoneum, through which trocars - special endoscopic equipment - are inserted. The surgeon removes appendicitis under computer control - everything that happens is displayed on the monitor. The only drawback is the possibility of incomplete removal of purulent exudate and recurrence of appendicitis.
After the operation, the patient is prescribed long-term antibiotic therapy with regular blood and urine tests to exclude leukocytosis and secondary infectious complications.
Recovery period
The early recovery period includes regular dressings, monitoring the condition of the suture, and antiseptics of drainage installations. If the patient feels adequate, he is discharged from the hospital on the 10th day.
Diet
Diet therapy is of key importance only in the early postoperative period . The diet consists of plenty of fluids and liquid food. On the first day, slimy porridges, soups with low-fat meat or vegetable broth, jelly, and ground main courses are suitable. The main indicator of the health of the intestinal tract is independent stool without pain and blood impurities.
Subsequently, the patient switches to a normal diet with a limit on gas-forming and fatty foods , coarse fiber, fresh bread (crackers, toast are suitable), alcohol and dishes that can provoke stool upset.
Important! No methods of traditional medicine, especially self-medication, can bring positive therapeutic results. Chronic appendicitis poses a serious threat to the life and health of the patient, especially with exacerbation of the pathological process.