Classification of the disease
Gastroduodenitis (symptoms and treatment in adults directly depend on the area of the inflammatory focus, the level of acidity in the stomach, as well as the etiological factor, which is fundamental in the development of the disease) has several varieties. Based on this, pathology of the digestive tract is divided into the following categories.
| Classification | Characteristics of the clinical picture |
| According to the concentration of gastric juice acidity |
|
| According to the area of prevalence of the focus of the inflammatory process |
|
| According to the etiological factor that predominates in the clinical picture |
|
All these classification characteristics are taken into account during the examination of the patient, and are also indicated by the attending physician when making a diagnosis. The most common type is gastroduodenitis of the primary type with increased secretory function of the stomach.
Symptoms
In the chronic course of the inflammatory process, the manifestations of the disease are wave-like and are observed in the spring and autumn. Exacerbation can be observed under the influence of unfavorable factors, regardless of the time of year, which also requires treatment with medications. If a patient has chronic gastroduodenitis, the symptoms and their severity are determined by several factors. The intensity of the manifestation depends on the degree of damage to the mucous membrane, the level of acidity, and the nature of the involvement of adjacent organs and systems in the pathological process.
Symptoms of duodenitis
Exacerbation of chronic gastroduodenitis
The appearance of unpleasant signs indicates the activation of the inflammatory process. The cause may be a violation of the diet, taking medications, or exposure to harmful substances. Often the occurrence of complaints is associated with the patient’s refusal of anti-relapse treatment. Symptoms of exacerbation of chronic gastroduodenitis in such cases are presented:
- Painful sensations in the upper half of the abdomen, where the stomach and the initial parts of the duodenum are projected. Discomfort is observed after eating 1-3 hours or on an empty stomach, including at night.
- Dyspeptic syndrome in the form of vomiting, nausea, belching, heartburn, a feeling of fullness in the stomach, a feeling of bitterness in the mouth, bad breath, bloating.
- Changes in bowel movements, characterized by diarrhea or constipation. Some patients complain of the symptom of slipping, when there is an urge to defecate during or immediately after eating.
- Asthenovegetative changes - there is weakness, fatigue, low blood pressure, drowsiness.
- Loss of body weight.
With unstable remission, exacerbations are a constant concern, and the seasonality of the disease is erased. In such patients, dyspeptic syndrome is constantly observed, but pain occurs only against the background of provoking factors. The clinical stage is confirmed by endoscopic data.
Brief characteristics of various forms of gastroduodenitis
Each form of gastroduodenitis has its own characteristic clinical picture, characterized by intense or moderate symptoms, acute or chronic course. Below is detailed information about each form of this disease.
Superficial gastroduodenitis
The most common pathology, which is mainly diagnosed in people who violate their diet and abuse fast food. The first symptoms of the disease are nagging pain in the stomach area, which worsens after eating spicy, sour or too salty foods.
Without proper treatment, the disease can develop into an ulcerative formation. Children aged 7 to 12 years and students are at risk. It is considered the mildest form of gastroduodenitis.
Erosive gastroduodenitis
Gastroduodenitis (symptoms and treatment of the erosive form of the disease in adults require a longer period of time) is a fairly common disease.
The course of this pathology is characterized not only by the formation of an inflammatory process, but also by the destruction of the mucous membrane of the stomach, as well as the duodenum. If the foci of erosion are not stopped in time, then under the influence of the aggressive environment of gastric juice they may transform into an ulcer.
Hypertrophic (nodular) gastroduodenitis
It is characterized by the appearance of anatomical changes on the surface of the mucous membrane. The functional abilities of the affected organ decrease, digestion and absorption of food worsen.
The main reason for the development of hypertrophic gastroduodenitis is associated with prolonged inflammation of the mucous membrane, which has not been subjected to proper drug treatment. A distinctive feature of this form of the disease is that the stomach tissue thickens and grows.
Hemorrhagic gastroduodenitis
Gastroduodenitis (symptoms and treatment of the hemorrhagic form of the disease in adults requires determining the causative factors of the disease) negatively affects the mucous membrane of the digestive organs.
This type of disease is always characterized by acute symptoms and in 75% of cases is accompanied by capillary bleeding. The patient needs emergency drug therapy.
Atrophic gastroduodenitis
Under conditions of constant inflammation, the gastric mucosa becomes thinner to such an extent that the glands responsible for acid synthesis reduce their efficiency.
In this regard, the level of secretory activity decreases. Food entering the stomach takes 2 times longer to digest, and overall health worsens. Advanced forms of atrophic gastroduodenitis provoke irreversible changes in the tissues of the digestive organs.
Mixed gastroduodenitis
Gastroduodenitis (symptoms and treatment in adults of the mixed form of the disease is the most difficult task for the doctor and the patient himself) is difficult to treat with medication. This is due to the fact that the mucous membrane of the duodenum and pyloric segment of the stomach suffers simultaneously from several types of disease.
In this regard, it is necessary to use several therapeutic techniques aimed at relieving the inflammatory process, preventing capillary bleeding and atrophic changes in tissues.
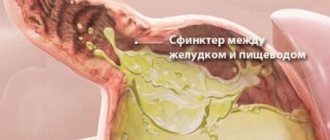
Reflux gastroduodenitis (type C gastritis)
Inflammatory pathology of the stomach, namely its mucous membrane, provoked by the fact that due to the contraction of the duodenum and the opening of the sphincter, a reflex reflux of bile into the stomach occurs from its cavity.
In this regard, the digestive function of the organ is disrupted, and symptoms appear, expressed in a constant feeling of bitterness in the mouth, nausea, and vomiting, although the liver tissue is normal.
Catarrhal gastroduodenitis
One of the most dangerous types of this disease, since it occurs suddenly, has an acute clinical picture with dynamic damage to the mucous membrane of the organ and deeper tissues. Most often it manifests itself under the influence of bacterial infection, viral microorganisms, chemicals, and liquids with high thermal parameters.
The patient requires urgent medical attention. Otherwise, internal bleeding may occur, resulting in death.
Varieties
When are antibiotics prescribed?
If the cause of the disease is Helicobacter pylori, then antibiotics will be needed for treatment.
It is necessary to take drugs with antibacterial effects only if the pathology is caused by the bacteria Helicobacter pylori. Otherwise, taking medications negatively affects the condition of the mucous membrane. Antibiotics for gastroduodenitis are prescribed by the doctor on an individual basis. For pathology, the following antibiotics are used, presented in the table:
| Component | Name |
| Clarithromycin | "Klacid" |
| "Claricide" | |
| "Binocular" | |
| "Clarexide" | |
| Omeprazole | "Omez" |
| "Omefez" | |
| "Promez" | |
| Amoxicillin | "Amoxicar" |
| "Amoxicillin" | |
| "Amosin" |
The main disadvantage of antibacterial therapy for gastroduodenitis is the many adverse reactions.
How to cope with pain?
Odeston will relieve a person from severe pain.
With pancreatitis, gastritis, gastroduodenitis, the patient is often bothered by a painful attack. Two types of painkillers help cope with unpleasant symptoms:
- Antispasmodics. Their action is aimed at relaxing the smooth muscles of the gastrointestinal tract, resulting in a decrease in pain. The group of antispasmodic drugs includes: “No-Shpa”;
- "Drotaverine";
- "Odeston";
- "Duspatalin."
- "Platifillin";
Antisecretory drugs
Patients can take Nolpaza at home on their own.
Drugs in this group are aimed at reducing secretory function. Nolpaza and many other antisecretory medications are approved for home use. But there are drugs that are used exclusively for inpatient treatment. The table shows the main groups of antisecretory drugs for gastroduodenitis:
| Types of drugs | Name |
| H2-histamine receptor antagonists | "Famotidine" |
| "Ranitidine" | |
| M-anticholinergic drugs | "Methacin" |
| "Gastrotsepin" | |
| "Atropine" | |
| Proton pump blockers | "Omeprazole" |
| "Pariet" | |
| "Rabeprazole" |
For what purpose are enzyme medications used?
With gastroduodenitis, the function of the duodenum, pancreas, and stomach is impaired. To normalize it, enzymatic medications are prescribed that improve the digestion process and include digestive enzymes. It is possible to normalize liver function by consuming Allohol. Drugs such as:
Festal will help food to be properly digested and absorbed.
- "Ganaton";
- "Pancreatin";
- "Hilak forte";
- "Trimedat";
- "Festal";
- "Mezim forte";
- "Panzinorm";
- "Enzistal".
Prescribing sedatives
Sedatives are often included in complex drug treatment. Such tablets for gastroduodenitis improve the patient’s general condition, calm the nervous system, and dampen pain. Effective means of this group:
- "Eleutherococcus";
- "Valerian";
- "Elecampane P."
Almost all sedative pharmaceuticals consist of natural products, so when used for gastroduodenitis there is no adverse reaction and the mucous membrane is not damaged.
Antacid drugs
Rennie quickly copes with high stomach acidity, which helps relieve unpleasant symptoms.
“Almagel” for gastroduodenitis and other antacids have been used in medicine for a long time. Their action is based on a rapid decrease in acid levels, eliminating pathological symptoms of inflammation of the mucous membrane. Drugs of this group are divided into 2 types. The first includes absorption antacids, which act quickly, but in the future can aggravate the course of gastroduodenitis. Popular drugs in this group:
- "Renny";
- "Vikalin";
- "Magnesium oxide."
The second type of antacids is non-absorbable, which have a milder effect on the mucous membrane of the gastrointestinal tract. After use, the acidity level is reduced and the release of carbon dioxide is prevented. The following medications are often used:
- "Maalox";
- "Phosphalugel";
- "Gastracid";
- "Riofast";
- Gaviscon.
Causes
The development of any form of gastroduodenitis is possible only under the influence of a number of factors that negatively affect the functioning of the digestive system. The following are the most common causes of gastroduodenitis in adults:
- abuse of strong alcoholic drinks, smoking;
- improperly organized nutrition, the presence in the diet of an excess amount of fried, fatty, smoked food containing an increased concentration of carcinogens;
- hereditary predisposition to inflammatory diseases of the stomach, intestines, duodenum, gall bladder, and liver;
- the predominance of confectionery and bakery products in the patient’s menu, refusal to eat liquid dishes (soup, borscht, broths);
- the presence of concomitant gastrointestinal diseases in the form of ulcers, dyskinesia of the bile ducts;
- use of chemicals of toxic etiology (poisoning with acids, alkalis and other aggressive compounds);
- infection of the digestive system by a bacterial microorganism - Helicobacter pylori.
Each of the above causative factors can cause pathological damage to the mucous membrane of the digestive organs, provoking the development of acute or chronic forms of gastroduodenitis.
Causes of gastroduodenitis
There are endogenous and exogenous causes of the development of gastroduodenitis. With increased acid formation and low mucus production, and disruption of hormonal regulation of secretion, endogenous gastroduodenitis develops. Diseases of the liver and biliary tract, and disruptions in the endocrine system can also cause the development of gastroduodenitis.
Exogenous development factors include physical ones - for example, eating spicy, cold or hot foods, exposure to chemicals (pesticides). The penetration of the bacterium Helicobacter pylori into the digestive tract is also important.
The main causes of gastroduodenitis include:
- Poor or very fatty and spicy food;
- Non-compliance with food intake, dry food;
- Various stresses, psychological pressure;
- Helicobacter pylori infection;
- Infections that developed in the oral cavity and pharynx;
- Recently, it has been noticed that the causes of superficial gastroduodenitis may be a genetic predisposition to such diseases.
In addition, there are acute and chronic forms of gastroduodenitis, when periods of remission alternate with exacerbations.
Reasons for the development of acute gastroduodenitis:
- Toxic effects of chemicals and spoiled food, irritating the mucous membrane of the stomach and intestines;
- Consumption of hot spices and seasonings;
- High concentration of residual pesticides in food;
- Complications of intestinal infections and chronic somatic diseases;
- Increased production of hydrochloric acid in the stomach in combination with a decrease in the protective properties of the mucous membrane, occurring against the background of stress and poor diet.
Approximately 65-70% of cases of gastroduodenitis are a chronic form of the pathology.
Causes of chronic gastroduodenitis:
- Heredity;
- Helicobacter pylori infection;
- Complication of acute gastroduodenitis;
- Staying in constant stress mode;
- Poor nutrition with a deficiency of protein, vitamins and microelements;
- Dietary disorder;
- Diseases of other gastrointestinal organs (intestines, pancreas, gall bladder);
- Complications of somatic diseases (autoimmune and endocrine pathologies, blood diseases, liver and kidney failure);
- Side effects of drugs (NSAIDs, glucocorticosteroids) during long-term use;
- Smoking and alcoholism.
Each case of gastroduodenitis may have more than one reason for its occurrence. Several decades ago, after the discovery of the bacterium Helicobacter pylori in 1983, approaches to determining the etiology of this disease changed dramatically.
The flagella of active strains of pathogenic bacteria are able to penetrate through the epithelium of the gastric and intestinal mucosa damaged by it, and its enzymes break down the membrane proteins. Urease secreted by Helicobacter pylori disrupts microcirculation in the tissues of the gastrointestinal tract; hydrochloric acid ions damage the capillaries of the blood vessels of the stomach and intestines. All of these aspects contribute to the development of inflammation.
Normally, the bacterium is found in the gastrointestinal tract of almost every person, getting there in childhood.
Helicobacter pylori exhibits its destructive function due to a combination of the following factors:
- Violation of the nervous and endocrine regulation of gastrointestinal tract functions;
- Increased acidity of gastric juice and impaired production of its protection in the form of mucus;
- Imbalance of the ACUD system, which produces biologically active substances and hormones;
- Violation of the regenerative functions of the gastric and intestinal mucosa.
Symptoms of gastroduodenitis in adults
The specificity of the manifestation of signs of a painful condition of the lining of the duodenum, as well as the pyloric part of the stomach, depends on the form in which the disease develops.
Symptoms of an acute type of disease are as follows:
- severe pain in the central part of the abdominal cavity, which resembles a burning sensation;
- nausea associated with periodic vomiting;
- refusal to eat;
- acute intestinal disorder manifested in the form of diarrhea;
- heartburn that occurs after eating all types of foods;
- in especially severe cases, body temperature may rise to 37-38 degrees Celsius.
The chronic form of gastroduodenitis is no less dangerous than the acute form, and is also expressed in the form of the following symptoms:
- aching pain localized in the center of the abdomen, occurring periodically (especially often manifested after eating hot, sour, salty, pickled, fatty, fried, rough foods);
- a sudden feeling of nausea, which also disappears;
- decreased appetite;
- loss of physical strength, weakness, drowsiness;
- poor absorption of consumed food.
Over time, chronic gastroduodenitis leads to atrophic processes in the mucous membrane of the digestive organs, disrupts metabolic processes in the body, and reduces the secretory function of the gastric glands.
Prevention
There are primary and secondary prevention. The primary one comes down to measures that contribute to the normalization of the function of the gastrointestinal tract and the body as a whole: giving up bad habits, working and resting hours, rational nutrition in accordance with age, gender, energy costs, sanitation of the oral cavity, and undergoing periodic preventive examinations.
Secondary prevention comes down to the correction of risk factors, anti-relapse therapy and includes dietary nutrition corresponding to the clinical-endoscopic stage of the inflammatory-dystrophic process in the coolant/duodenum with sufficient sleep, increased physical activity, physical therapy, and hardening.
Diagnostics
To undergo an initial examination and receive a referral for a more thorough examination, you must seek medical help from a general practitioner or gastroenterologist.
In order for a specialist to be able to confirm or refute the presence of gastroduodenitis in a patient, it is necessary to undergo the following types of diagnostics:
- endoscopy – allows you to detect single or multiple foci of diffuse changes in the mucous membrane, and also reflects the hypertrophic state of tissues;
- histology - using special equipment, the doctor selects a piece of biological material from the surface of the digestive organ being examined in order to establish the severity of mucosal dystrophy, the presence or absence of altered cells;
- intragastric pH-metry - shows the secretory activity of the stomach glands responsible for acid synthesis (this diagnostic method allows you to examine each section of the digestive organ, establishing dysfunction in a specific segment);
- measuring the acidity of the duodenum - confirms or refutes the acidification of this part of the gastrointestinal tract;
- antroduodenal manometry - carried out to check the motor function of the gastrointestinal tract;
- Ultrasound of the stomach - the organ is completely filled with water, so that during diagnosis only its walls and tissues without dense content are displayed;
- fluoroscopy with filling the stomach with a barium solution is not a direct indication in the diagnosis of gastroduodenitis, but allows one to identify pathologies such as tumors, duodenal obstruction of food, stenosis of the turn, which provoke inflammatory processes of the mucous membrane.
In addition, a mandatory condition for a diagnostic examination is to check the microflora of the stomach and duodenum. This is necessary to exclude the bacterial nature of the origin of the disease and to formulate the most effective treatment regimen.
Forms of superficial gastroduodenitis
When superficial gastroduodenitis (superficial gastroduodenopathy) develops against the background of other pathologies of the digestive tract, it is secondary (endogenous); when a disease occurs against a background of relative health, it is considered primary (exogenous).
According to the level of inflammation, the pathology is regarded as the mildest. If at the initial stage of the pathology the disease is not recognized and treatment is not started, the inflammation can go first into an erosive and then into an atrophic or hyperplastic phase. In addition, the disease can occur against a background of low, normal or high acidity.
There are also several phases that replace each other: exacerbation, remission - complete or incomplete.
Depending on the severity of symptoms, the following is determined:
- Acute gastroduodenitis, in which there is severe pain, nausea, often with vomiting.
- Chronic. With it, the pain is not so intense, but almost constant, the symptoms are moderate.
Depending on the development of the disease and the type of course, pathology is divided into the following types:
- focal. This is the earliest and mildest form of pathology. The clinical picture of the disease is mild, pain is moderate, nausea and vomiting practically do not occur. Possible heartburn. One or more foci of inflammation appear on the mucous membrane. With proper therapy, the pathology can be completely eliminated. The consequences of the disease if left untreated can be serious: ulcers, erosions, cancer;
- diffuse (widespread). This form affects almost the entire mucous membrane at once, the symptoms are pronounced, treatment is more difficult and longer. This form often appears in adults;
- cardia failure. In this case, there is a closure of the valve responsible for separating the stomach from the esophagus, which is connected to it. As a result, a burn to the esophagus may occur;
- duodenogastric reflux. With this pathology, food is thrown back into the stomach from the intestines.
Treatment of gastroduodenitis
Therapy for gastroduodenitis is a long and consistent process, consisting of a set of methods aimed at restoring stable gastrointestinal function and relieving inflammation of the mucous membrane.
Treatment of the disease includes the following actions on the part of the doctor and the patient himself:
- taking medications that are indicated in a specific clinical case (antibacterial, antacid, enzyme, vitamin and mineral complexes);
- compliance with the drinking regime;
- eating food according to the prescribed diet;
- physical activity.
If there are concomitant gastrointestinal diseases that prevent the elimination of signs of gastroduodenitis, therapy for these pathologies will be required.
After completion of the course of treatment, the patient continued to continue for the next 6 months. adheres to the prescribed diet, not consuming foods that irritate the gastric mucosa (sour, spicy, salty, fatty, fried).
What is gastroduodenitis
Inflammation of the mucous membrane of the digestive tract is rarely isolated. In most cases, the process begins in one department and gradually spreads to nearby areas. Gastroduodenitis is a lesion of the epithelium of the stomach (in the area of the pylorus) and duodenum.
Pathological changes lead to functional disorders, which affects the functioning of the gastrointestinal tract. The disease can be suspected by indirect signs, which are confirmed by instrumental examination.
In some patients, gastrointestinal sphincter insufficiency may develop with the development of duodenogastric reflux. If left untreated, refluxate (stomach contents mixed with bile) regularly enters the esophagus and provokes inflammation - reflux esophagitis.
Medications
Effective therapy for gastroduodenitis is impossible without the use of medications.
The following medications are used for these purposes:
- antacids – necessary to reduce the level of acidity if the patient has increased secretory activity of the gastric glands (Vikalin, Almagel);
- antispasmodic - to relieve pain and organ spasms that occur under the influence of an acute inflammatory process (Spazmalgon, Drotoverine hydrochloride, Spasmol);
- antibacterial - used to suppress pathogenic microflora parasitizing in the pyloric part of the stomach and duodenum, provoking their painful state (Amoxicillin, Clarithromycin, Esomeprazole, Lansoprazole);
- antioxidant - required to prevent atrophic processes in the mucous membrane, rapid restoration of damaged tissues (Tocopherol, Ascorbic acid, Retinol, Ubiquinone, Beta-carotene).
The above medications are used both for the chronic type of the disease and in the case of the development of an acute form of gastroduodenitis. The difference lies only in the dosage and duration of the therapeutic course, which is always determined exclusively by the attending physician.
Kinds
Gastroduodenitis is divided into two types according to the predominant etiological factor:
- Primary (exogenous).
- Secondary (endogenous).
When infected with the bacterium Helicobacter pylori, gastroduodenitis occurs:
- HP-positive (Helicobacter pylori infection was detected in the stomach);
- HP-negative (no Helicobacter pylori infection).
According to the clinical picture and duration of the course, gastroduodenitis is divided into two forms:
- Acute, the duration of which is approximately three months. The inflammatory process affects the mucous membranes of the stomach and duodenum, the motor functions of the digestive organs are disrupted, and the passage of food becomes difficult. Acute gastroduodenitis is considered a consequence of gastritis and often becomes chronic.
- Chronic, which develops in the absence of treatment for the acute form of the disease. In some cases, primary chronic gastroduodenitis occurs, which is characterized by alternating periods of remission and exacerbation. The disease lasts more than 6 months.
According to the level of acidity, gastroduodenitis can be:
- with high acidity (the most common type of disease);
- with normal acidity;
- with low acidity (with this type of pathology there is a high probability of developing stomach cancer).
According to the characteristics of the pathological process in the mucous tissues of the stomach and duodenum, determined by endoscopic examination, gastroduodenitis is classified into several types:
| Type of gastroduodenitis | Description |
| Surface | The inflammatory process develops in the mucous tissues of the stomach and duodenum, there are no erosions, the functions of the glands are not impaired |
| Hypertrophic (nodular) | The pathological process is manifested by thickening of mucous tissues, the formation of folds and outgrowths. Erythematous syndrome develops (affected areas of the mucous membrane become red) |
| Erosive | On the mucous membrane of the stomach and duodenum, multiple small wounds form, metaplasia develops (atypical cells characteristic of the intestine appear in the stomach) |
| Atrophic | The mucous tissues of the stomach and duodenum become thinner and atrophy |
| Mixed | Mucous tissues look like a hypertrophic form of the disease, however, signs of atrophy are also observed |
According to the degree of tissue damage, which is determined by histological indicators, gastroduodenitis is:
- With mild damage.
- With moderate or severe damage.
- With atrophy.
- With metaplasia.
According to the localization of the pathological process, gastroduodenitis is classified into:
- ulcer-like (the most common variant of the pathology). May be combined with gastric ulcer;
- Gastritis-like. With this type of pathology, the absorption of nutrients and digestive functions is impaired;
- pancreatitis-like. Characterized by pain under the ribs on the right (after eating fatty foods).
Diet and nutrition
The acute form of the disease involves the consumption of grated and pureed foods. First, the products are steamed, or they are boiled, and then turned into a paste using kitchen tools. They are eaten lightly salted and slightly warm.
The diet should be dominated by cereal porridges and lean chicken, but not more than 150 g per day. You are allowed to drink not very strong tea (only warm), herbal decoctions with an anti-inflammatory spectrum of action, and jelly. The main task is to provide the body with nutrition and minimize the load on the stomach.
Symptoms of gastroduodenitis depend on the form of the disease. The success of treatment depends on diet
Chronic gastroduodenitis also requires compliance with dietary standards, but they are less stringent. Chicken cutlets and chops cooked in a steam bath are allowed into the diet.
Table salt consumption increases to 8 g per day. It is allowed to include bakery products in the menu. As in the case of the acute form of the disease, it is forbidden to eat spicy, spicy, too hot, salty, sour, pickled, fried, fatty foods.
Causes of the disease
The main reason for the development of the disease is irregular nutrition or consumption of junk food. Severe superficial gastroduodenitis can also be caused by the microbe Helicobacter pylori, which is a powerful irritant for the intestinal mucosa. There are other reasons for the appearance of pathology:
- regular physical and mental overload, depression;
- smoking, alcohol abuse;
- poisoning with poisons and toxic substances;
- genetic predisposition;
- radiation exposure;
- frequent consumption of salty, spicy, pickled and smoked foods;
- long-term use of antibacterial drugs;
- increased secretion of hydrochloric acid in the stomach;
- starvation diets.
In some cases, gastroduodenitis develops against the background of diseases of the liver, urinary and biliary tract.
Menu for gastroduodenitis
A patient with gastroduodenitis must adhere to dietary norms daily in order to speed up the process of his recovery.
Below is a sample menu for diet No. 1:
- Breakfast: steamed omelet, chamomile tea with herb honey;
- Snack: red apple baked in the oven in its own juice;
- Lunch: pureed cauliflower soup, to which rye crackers are added (make sure they are well liquefied and not hard), mashed potatoes and steamed fish cutlets;
- Afternoon snack: curd mass;
- Dinner: pureed vegetables and chicken breast, boiled beets, grated on a fine grater.
Also, at all stages of treatment the following menu of dietary table No. 5 can be used:
- Breakfast: cream soup based on oatmeal, a piece of rye bread, cottage cheese;
- Snack: fresh pear puree;
- Lunch: steamed fish meatballs, rice, dried fruit compote;
- Afternoon snack: a glass of milk with a minimum level of fat;
- Dinner: vinaigrette with as finely chopped vegetables as possible, dressed with olive oil, boiled egg yolk.
If a persistent feeling of hunger appears between meals, it is recommended to drink a glass of milk or fresh kefir to prevent the product from becoming acidic. Diet menu No. 1 is more suitable for patients with an acute form of the disease, and table No. 5 is indicated for chronic gastroduodenitis.
Folk remedies
Alternative medicine offers its alternative methods of treating gastroduodenitis, which are suitable for relieving acute and chronic inflammation in the mucous membrane of the duodenum, as well as the pyloric part of the stomach.
It is recommended to use the following recipes:
- take 100 g of flax seeds, boil them for 10 minutes. in 500 ml of water, leave to brew for 2 hours, and then take 2 tbsp. l. 4 times a day on an empty stomach (course of therapy from 20 to 30 days);
- select 5 potato tubers that have no signs of rot or other defects, use a juicer to squeeze the juice out of them and take it 3 times a day for 30 minutes. before meals (single dosage is 1 tbsp, and the duration of therapy is 10 days);
- collect the leaves of the aloe flower, squeeze out the maximum amount of juice from them, mix it in equal proportions with honey from herbs and take 1 tbsp. l. 2 times a day for 20 minutes. before meals (terms of therapy from 15 to 20 days);
- take 1 tbsp. l. dried chamomile, pour 1 liter of running water, boil for 10 minutes, and take the resulting decoction warm, 250 ml 4 times a day and always on an empty stomach;
- pour 2 tbsp into a thermos. l. dried and crushed plantain leaves, pour 1.5 liters of boiling water over them, leave for 2 hours to infuse, and after the specified time, take 200 ml 3 times a day for 15 minutes. before meals.
Before starting treatment for gastroduodenitis with folk remedies, it is necessary to undergo a comprehensive examination of the gastrointestinal tract, consult with a general practitioner or gastroenterologist, and only take home medications with his permission.
Treatment
For the treatment of acute gastroduodenitis, complex therapy is used, including:
- drug treatment;
- diet;
- traditional medicine methods.
Drug therapy
In case of a severe attack of acute gastroduodenitis, the patient is hospitalized in a hospital, where, first of all, his stomach is washed. If the patient’s condition is not severe, bed rest is prescribed for 6-7 days and medications that alleviate the manifestations of the disease.
If acute gastroduodenitis is caused by Helicobacter pylori bacteria or other infections and parasites, antibacterial or antiparasitic treatment is prescribed. According to the clinical recommendations of the Russian Gastroenterological Association, triple therapy (De-nol, Amoxicillin, Clarithromycin) or proton pump inhibitors (Rabeprazole, Omeprazole, Esomeprazole) in combination with antibiotics are used to suppress Helicobacter pylori infection.
In addition, the following drugs are used to treat acute gastroduodenitis:
- Receptor blockers. Regulate secretory functions (Famotidine, Ranitidine).
- Antacids (Almagel, Sinaflan).
- Cytoprotectors. Protect mucosal cells (Venter).
- Prokinetics (Cerucal, Motilium).
- Antispasmodics (No-shpa, Papaverine).
- Enzymes (Acidin-pepsin, Betacid).
- Motility modulators (Metoclopramide, Drotaverine).
- Antidiarrheal drugs.
- Vitamin complexes.
Diet
In acute gastroduodenitis, as in any disease of the digestive system, it is necessary to select proper nutrition. A therapeutic diet in combination with drug therapy helps relieve pain and other unpleasant manifestations of the disease, and prevents the progression of the inflammatory process. It is necessary to follow several rules of healthy eating:
- eat food every 3 hours in small portions (250–300 g);
- follow a diet, eat at the same time;
- the diet should be nutritious, balanced and varied;
- You should not eat too hot or cold food, the food should be warm;
- food should be boiled, stewed or steamed;
- it is necessary to exclude salted, fried, spicy, fatty, pickled, smoked foods, as well as coffee, alcoholic and carbonated drinks;
- limit salt intake, minimize spices and herbs.
List of basic foods that can and cannot be included in the diet for acute gastroduodenitis:
| Can | It is forbidden |
| Dried wheat bread, dry biscuits, sponge cake without cream | Fresh and rye bread, butter and puff pastries |
| Vegetable and milk soups with boiled cereals (rice or oatmeal), noodles | Fatty, smoked, salted fish, canned fish |
| Lean meat and chicken (without skin, fat and tendons), steamed cutlets | Fatty meat, sausage products, smoked meats, canned meat |
| Dairy products (not sour or fatty) | Sour and fatty dairy products, spicy and salty cheeses |
| Soft-boiled eggs (2 pieces per day), steamed omelet | Wheat and pearl barley, durum wheat pasta |
| Porridge from buckwheat, oatmeal, rice, semolina | Sour fruits and berries |
| Boiled vegetables (potatoes, beets, carrots), fresh tomatoes (up to 100 g per day) | Chocolate, confectionery, ice cream |
| Fruit compotes and jelly, still mineral water | Sorrel, white cabbage, onion |
Folk remedies
In acute gastroduodenitis, traditional medicine is widely used as an adjuvant:
- 2–3 tbsp. lie mint (fresh or dry) are placed in a thermos and filled with ½ liter. boiling water, infuse for a day. Drink 50 ml of infusion before meals.
- 1 tbsp. lie Pour celandine with a glass of medical alcohol and leave for 2 weeks. It is recommended to start treatment with five drops of tincture per day. Gradually the dose should be increased (1 drop per day) to 50 drops. After this, reduce in reverse progression to 5 drops. After this, the course of treatment is stopped. The tincture can be reused after six months.
- 1 tbsp. lie flax seeds are poured with warm water, brought to a boil and cooked over low heat for 10–15 minutes. Take 50 ml before meals (1 month).
- To prepare decoctions, medicinal herbs are used, both in collections and independently: St. John's wort, chamomile inflorescences;
- Yarrow, centaury;
- Calamus root, wormwood, bearberry;
- Gentian rhizomes;
- Caraway seeds, knotweed, dried grass;
- Plantain, dill seeds, valerian root;
- Hop cones, rose hips.
To prepare a decoction, the herbs are crushed. 1 tbsp is poured into a thermos. lie raw materials and pour ½ liter of boiling water. Leave for 8 hours. The decoction should be consumed ½ cup before meals. You need to drink any decoction for three months, then take a break for 2 weeks. After this, you can begin a course of treatment with another remedy. For maximum effect, herbal medicine courses can be repeated 3-4 times a year, even if the condition improves.
Treatment of the chronic form
In order for the treatment of the disease to bring a positive effect, the following actions must be performed daily:
- take medications indicated in the drug therapy section (as prescribed by a doctor);
- drink at least 1 liter of still mineral water daily, which contains magnesium ions;
- do not eat fried, sour, too salty, hot, spicy, rough foods;
- follow the dietary rules recommended by your doctor;
- give up alcoholic beverages, smoking and other harmful addictions.
Treatment of chronic gastroduodenitis, elimination of symptoms and restoration of normal digestive function in adults, requires the patient to comply with all of the above rules. Otherwise, the disease will periodically enter the acute phase of development.
Article design: Mila Friedan
When is treatment needed?
Usually, in the acute development of the disease, bed rest is required. The selection of medications is made depending on the cause of gastroduodenitis, the depth of damage to the walls of the stomach, as well as the duodenum and the level of secretion of gastric juice. The treatment uses choleretic agents, anticholinergics, histamine blockers, prokinetics or antacids. The choice of medications always remains with the attending physician.
However, after the acute manifestations have stopped, therapeutic measures do not end there. Treatment for a chronic disease is also necessary during the period of remission. There are many drugs recommended for long-term use. Duspatalin is often used to relieve spasms. It is prescribed not only for acute gastroduodenitis, but also for the treatment of chronic forms.