More about pathology
There are many dangerous diseases that can lead to death, and one of these pathologies is destructive pancreatitis, or, as it is otherwise called, pancreatic necrosis. This disease is characteristic of the pancreas, it is difficult to treat and, as a rule, is the result of a long-term lack of necessary therapy for the inflammatory process of this organ.
According to statistics, a quarter of the hundred known cases ended in death. That is why it is so important to pay attention to your health, seek medical help on time and, in general, know the very important information that concerns the etiology, clinical picture and methods of treating destructive pancreatitis.
Inflammation of the pancreas (PG), which is characterized by the death of organ tissue without the possibility of their regeneration, is pancreatic necrosis, or pancreatitis of the destructive type. The pathological process is accompanied by the destruction of cellular structures, which inevitably leads to the entry of their contents into the intercellular space and thereby provokes severe swelling and self-digestion of the organ. This phenomenon is commonly referred to in medicine as destruction.
Pancreatic necrosis, in addition to global changes in the pancreas and its dysfunction, in parallel causes disruption of the activity of other organs of the digestive system. Most often, destructive pancreatitis is a logical consequence of inflammation of the pancreas: improper or untimely treatment of one disease in almost all cases leads to the development of another.
This circumstance is accompanied by rapid progression of the pathology, as a result of which changes in cellular structures become simply irreversible - this is the main danger of pancreatic necrosis. A worsening situation is usually indicated by a number of specific signs, the most serious of which is coma.
Destructive type pancreatitis (or pancreatic necrosis) is an inflammation of the pancreas in which there is death of its tissues without the possibility of recovery. Due to a serious disturbance in metabolic processes, the iron swells and begins to digest itself. The result of destruction is not only necrosis of pancreatic tissue, but also disruption of the functioning of other organs - primarily those related to the gastrointestinal tract.
As a rule, destructive pancreatitis is preceded by ordinary pancreatitis. Specific symptoms may indicate that the situation has worsened. With pancreatic necrosis, the human nervous system suffers greatly, even to the point of coma.
Lack of timely treatment leads to rapid progression of the disease. And at some point, pathological changes become irreversible. According to some statistics, 25% of those suffering from pancreatic necrosis die from this disease. Other researchers cite an even more threatening figure - 40%.
ICD-10 code
Just like any other disease, destructive pancreatitis is recorded in a special medical reference book called the “International Classification of Diseases”. In the class “Diseases of the digestive organs” (K00-K93) there is a special section “Diseases of the gallbladder, biliary tract and pancreas” (K80-K87), in which there is a record of acute pancreatitis. The scope of this disease includes pancreatic abscess, as well as necrosis of an acute and infectious nature. The code for this pathology is K85.
Destructive pancreatitis - what is it?
Inflammation of the pancreas (PG), which is characterized by the death of organ tissue without the possibility of their regeneration, is pancreatic necrosis, or pancreatitis of the destructive type. The pathological process is accompanied by the destruction of cellular structures, which inevitably leads to the entry of their contents into the intercellular space and thereby provokes severe swelling and self-digestion of the organ. This phenomenon is commonly referred to in medicine as destruction. Pancreatic necrosis, in addition to global changes in the pancreas and its dysfunction, in parallel causes disruption of the activity of other organs of the digestive system.
Most often, destructive pancreatitis is a logical consequence of inflammation of the pancreas: improper or untimely treatment of one disease in almost all cases leads to the development of another. This circumstance is accompanied by rapid progression of the pathology, as a result of which changes in cellular structures become simply irreversible - this is the main danger of pancreatic necrosis. A worsening situation is usually indicated by a number of specific signs, the most serious of which is coma.
Causes of the occurrence and development of the disease
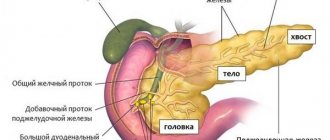
The pancreas is an important and irreplaceable organ involved in digestive processes. It produces three main enzymes:
- Lipase - responsible for the digestion of fats from food;
- Trypsin – responsible for the digestion of proteins;
- Amylase is responsible for the processing of carbohydrates.
In addition, the organ produces hormones that are responsible for human blood sugar levels.
Inflammation of the pancreatic tissue, narrowing or blockage of the pancreatic ducts leads to the fact that digestive enzymes do not enter the intestines, as they should, but begin their digestive activity in the pancreas. As a result of this, the process of digesting one’s own tissues begins. In addition, this “digestive” process extends beyond the pancreas itself and affects surrounding tissues and organs. These same enzymes enter the bloodstream, resulting in damage to the heart, liver, kidneys, brain, and lungs.
Classification of pancreatitis
According to the nature and duration of the inflammatory process, acute and chronic pancreatitis are distinguished. In turn, acute pancreatitis is divided into:
- edematous (intrestial) acute pancreatitis;
- reactive pancreatitis;
- sterile acute pancreatitis, which in turn is divided into:
- capitate; tail,
- mixed.
The most common types of pancreatitis are:
- finely focal;
- large-focal;
- and subtotal.
According to the form of necrotic lesion, pancreatitis is divided into:
- fatty;
- hemorrhagic;
- mixed;
- infectious.
Chronic pancreatitis is divided by etiological reason into:
- alcoholic;
- calculous;
- hereditary;
- drug;
- idiopathic (unknown etiology).
Based on morphological characteristics, they are distinguished:
- obstructive;
- purulent;
- calcifying;
- infiltrative-inflammatory;
- fibrosclerotic chronic pancreatitis.
Against the background of the intensity of the manifestation of symptomatic signs of pathology and the degree of its development, the following forms of pancreatic necrosis are distinguished:
- The development of toxemia, characterized by the entry into the blood of toxic substances that have a bacterial environment.
- The formation of an abscess that forms not only in the pancreas area, but also in nearby abdominal organs.
- The development of purulent changes that form both in the parenchymal organ itself and beyond the boundaries of the retroperitoneal tissue.
The disease is characterized by a severe course and, under unfavorable circumstances, the patient's death may occur. This can happen either in the first days after the onset of the attack as a result of the failure of vital organs and systems of the body (“early death”), or in the third or fourth week (“late death”) as a result of the occurrence of purulent-septic complications.
The following phases of disease development are distinguished:
- enzymatic;
- reactive;
- sequestration.
Each of them is characterized by specific changes in tissues and clinical symptoms.
The first is enzymatic
At this stage, necrotic changes in pancreatic tissue begin. This process occurs within three days and is called the enzymatic phase of the disease. Pancreatic enzymes leave the acinar cells and, under the action of the phospholipase A enzyme, cell membranes are destroyed, followed by penetration of the lipase enzyme into the gland cells.
When lipase is activated, necrosis of fat cells is observed, and with increased production of elastase, blood vessels are affected. This phase of pancreatitis lasts about 3 days, after which a light interval begins. The enzymatic stage becomes reactive
The second stage is reactive
This phase (intermediate) is characterized by the entry of enzymes and cell breakdown products into the bloodstream, signs of damage to other organs, and the formation of an infiltrate around the pancreas. The reactive phase begins from the 2nd week of development of acute pancreatitis.
The further development of the disease depends on the body’s response to foci of necrotic lesions. At this stage, the outcome depends on whether the peripancreatic infiltrate is reabsorbed, or whether cysts form and further suppuration occurs.
The third stage is sequestration
This phase begins in the third week after the onset of the attack and lasts up to several months. At this stage, fistulas and cysts form without further complications (sterile pancreatic necrosis), or the situation further worsens, that is, an infected form of pancreatic necrosis develops.
This is an extremely dangerous situation where abscesses, gastrointestinal bleeding, peritonitis and sepsis occur. At this stage, the likelihood of death is very high.
Typically, sequestration develops according to one of three events:
- The peripancreatic infiltrate resolves, after which the patient recovers - such a favorable outcome is possible only if the patient seeks help in a timely manner (this is 35%);
- Aseptic sequestration continues to progress: the necrotic area is torn away from the pancreas tissue, and the formation of a cyst is also possible, but without suppuration (this situation is observed in a third of patients diagnosed with destructive pancreatitis);
- Accumulation of purulent contents in the organ, which is fraught with the most disastrous consequences (this happens in 30-35% of patients).
Causes and symptoms of the development of acute forms of destructive pancreatitis
In accordance with data obtained as a result of scientific research conducted recently, the main factors of acute destructive pancreatitis are:
- alcoholic drinks;
- ailments associated with disorders of the biliary tract;
- infection with worms;
- peritoneal injuries;
- intoxication of various origins.
At the first suspicion of pancreatitis, the patient should be hospitalized immediately
With appropriate experience, any physician can easily identify the progression of acute destructive pancreatitis in a patient. The disease is easily determined by the presence of a triad of signs:
- Severe pain in the epigastric region.
- The occurrence of regular vomiting.
- Severe flatulence.
Painful sensations most often occur suddenly and are of high intensity and strength; they are very often observed when consuming fatty foods or alcohol in acute destructive pancreatitis. Painful sensations may be accompanied by shock, loss of consciousness and frequent vomiting. Frequent and debilitating vomiting leads to progression of dehydration.
In addition to these signs, a person experiences symptoms characteristic of general intoxication - this is an increase in body temperature, the occurrence of chills, tachycardia, shortness of breath and cyanosis of the mucous membranes of the patient’s body.
The characteristics of the pain felt are completely dependent on the form of the disease and the causes of its occurrence. The main features of the manifestations of pain are the following:
- the occurrence of discomfort;
- the patient falls into a state of collapse;
- development of acute pain in the epigastric region;
- the appearance of unbearable pain.
Vomiting that occurs as the disease progresses does not bring relief to the patient. At the same time, the skin of the face acquires a red tint, and when a person falls into collapse, the skin becomes pale.
A progressive disease leads to an increase in the concentration of elastase, which triggers the process of destruction of blood vessels in the circulatory system, which leads to bleeding in the organs of the digestive system.
Causes of the disease
The emergence and development of this deadly disease is due to a number of reasons, the main of which are excessive consumption of strong alcoholic drinks and gallbladder pathology.
Alcohol abuse. This is the most common cause of acute pancreatitis. As a rule, it occurs in people who have been drinking alcohol for 5-15 years, but cases of an attack cannot be excluded after a single incident of drinking alcoholic beverages, especially in combination with fatty fried foods.
Cholelithiasis. In this case, pancreatitis develops due to blockage of the sphincter of Oddi by a gallstone, resulting in bile entering the pancreas through the pancreatic ducts. Or there is a blockage of the pancreatic ducts with a gallstone and pancreatic enzymes, unable to enter the intestines, are activated in the gland itself.
In addition, a number of other causes of destructive pancreatitis are known:
- Uncontrolled use of medications;
- Infectious and viral diseases;
- Congenital defects of the pancreas;
- Pancreas injuries;
- Unsuccessful operations and postoperative complications;
- The presence of parasites in the body;
- Chemical poisoning and poisonous insect bites.
Most often, pancreatic necrosis becomes a consequence of advanced pancreatitis, but there are two more factors that significantly influence the development of this disease - pathologies of the bile ducts, accompanied by impaired outflow of bile, as well as systematic abuse of alcoholic beverages. Other circumstances can provoke the disease:
- Cholecystitis;
- Tumor formations of the gallbladder;
- Stomach or small intestinal ulcer;
- Helminthiasis;
- Serious viral or bacterial diseases affecting the abdominal organs;
- Unsuccessfully performed surgical interventions on the abdominal organs or gastrointestinal tract;
- Long-term or unnecessary use of certain groups of medications.
In some cases, the development of destructive pancreatitis is facilitated by excessive consumption of fatty, fried and too spicy foods - a diet consisting of such dishes does not benefit the body, but only disables it, which, of course, does not happen immediately, but over time.
Causes of the disease
Recent statistical studies indicate the following causes of acute destructive pancreatitis:
- drinking alcoholic beverages,
- helminthic infestations,
- biliary tract diseases,
- intoxication of the body with medications,
- infections and their complications,
- intestinal infarction,
- injuries of the peritoneal organs.
Acute destructive pancreatitis
According to observational data, acute pancreatitis in 15-20% has a severe destructive nature (destructive pancreatitis). There is also a high mortality rate from acute destructive pancreatitis - more than 30%. With severe complications, mortality reaches 100%.
The mortality rate for acute destructive pancreatitis has maximums in the 1st and 3rd-4th weeks from the onset of the disease. Fatal outcomes in the second week from the onset of the disease are rarely recorded and are observed in elderly patients or in weakened people.
Acute destructive pancreatitis has certain phases during the course of the disease, which are caused by pathological processes occurring in the pancreas and tissues surrounding the diseased organ and the body's response to these processes.
- Phase I is the enzymatic phase (early stage) of acute destructive pancreatitis. Duration - 3 days. from the onset of the disease. During this period, necrosis forms in the pancreas.
- "Lucid interval". Starting from 4-5 days. There is some subsidence of symptoms and stabilization of the condition. The “bright gap” gradually moves into the reactive phase.
- Phase II - reactive phase, 2nd week of the disease. Intermediate phase or stage of peripancreatic infiltrate.
- Phase III - sequestration phase, 3 weeks of illness or more. The sequestration phase has three directions: 35% of the number of observations - resorption of the peripancreatic infiltrate occurs. Recovery is coming.
- 35-40% of the number of observations - aseptic sequestration occurs (rejection of the necrotic area from tissues that have retained viability without suppuration), the formation of a parapancreatic cyst.
- 25-30% of the number of observations is septic sequestration, i.e. stage of purulent-septic complications, the latest and most dangerous stage of acute destructive pancreatitis.
Life forecast
The outcome of destructive pancreatitis is influenced by the following factors:
- the degree of destructive action of enzymes on tissue;
- size of the necrosis focus;
- the presence of local and systemic complications;
- age of patients;
- presence of concomitant pathology;
- timeliness of the operation.
The worst prognosis is observed with the following factors:
- a person over 50 years old;
- increase in the level of leukocytes in the blood more than 16*109/l;
- high concentration of urea;
- increased activity of liver enzymes;
- hyperglycemia (development of diabetes mellitus);
- dehydration.
In severe cases, the probability of death exceeds 50%. Early treatment can reduce the risk and improve the prognosis.
Symptoms
Symptoms of acute destructive pancreatitis appear soon after a heavy feast with large amounts of alcohol and fatty fried meat foods, or at night.
The occurrence of an attack of acute pancreatitis is characterized by:
- The appearance of acute and unbearable pain in the upper abdomen. It can be localized on the right side of the abdomen if the head of the pancreas is affected, on the left if the tail is affected, and in the center if the lesion affects the body of the pancreas. With total-subtotal damage, the pain is girdling in nature. Painful sensations are not relieved by painkillers.
- The occurrence of nausea and vomiting. Attacks of vomiting are protracted and painful. First is the previously eaten food, then bile. After an attack of vomiting, there is no relief.
- The presence of signs of flatulence and the appearance of diarrhea, which is due to a lack of enzymes that do not enter the intestines to ensure digestion processes.
As a result of intoxication, dehydration occurs. The patient feels dry mouth. Further, as the disease progresses, the following may occur:
- Facial redness;
- Temperature increase;
- Increased heart rate;
- Dyspnea;
- The appearance of bluish spots on the abdomen and buttocks as a result of vascular damage;
- Yellowing of the sclera of the eyes and icteric complexion as a result of impaired bile outflow;
- The emergence of a feeling of fear;
- Loss of consciousness.
Destructive pancreatitis does not immediately strike the patient: as a rule, a person suffering from inflammation of the pancreas is already familiar with some of the symptoms of this disease. That is why at the initial stage it is not so easy to determine what is the cause of concern: pancreatitis or a complicated form of this disease - pancreatic necrosis. However, there are a number of specific signs that indicate that the disease has become more serious.
Experts identify a triad of clinical manifestations that usually accompany the process of pancreatic cell death: severe pain, vomiting and diarrhea. It is a mistake to believe that pain during pancreatitis and its more complex forms is localized only in the right hypochondrium. Disturbances in the functioning of the pancreas may be accompanied by pain on the right if the head of the organ is affected, on the left if the lesions are located in the tail, and also in the center if the inflammatory process affects mainly the body of the pancreas.
Often the pain is radiating in nature: its impact can be felt in the area of the heart, back and even shoulder. Most often they occur in the evening or at night, and intense pain can persist for quite a long time; it subsides slightly if the patient takes a lying position and bends his knees to his stomach and chest. In general, with pancreatic necrosis, pain in its severity can be different:
- in 6% of cases it is moderate pain,
- 40% - acute,
- 45% - strong and unbearable,
- and in 10% it causes shock.
The second striking symptom of the onset of destruction of the pancreas is vomiting, which does not bring relief, and at the same time poses a particular danger to the body, because it can cause dehydration. In some patients, not only general exhaustion is observed, but also facial redness, which is explained by an increase in the concentration of vasoactive components. And vice versa, with the onset of a state of collapse, the skin begins to noticeably turn pale.
An increase in the level of elastase, which is accompanied by destructive pancreatitis, provokes massive destruction of blood vessels, resulting in bleeding of the digestive organs. Evidence of this is often blue-violet spots that appear on the surface of the skin of the buttocks, the anterior abdominal wall or in the umbilical area.
The third sign of an aggravated course of the disease is diarrhea; with pancreatic necrosis it is more pronounced, unstable stools become common, the patient suffers from bloating, as well as pain that accompanies this process.
Symptoms of the disease
Destructive pancreatitis does not immediately strike the patient: as a rule, a person suffering from inflammation of the pancreas is already familiar with some of the symptoms of this disease. That is why at the initial stage it is not so easy to determine what is the cause of concern: pancreatitis or a complicated form of this disease - pancreatic necrosis.
However, there are a number of specific signs that indicate that the disease has become more serious. Experts identify a triad of clinical manifestations that usually accompany the process of pancreatic cell death: severe pain, vomiting and diarrhea.
- It is a mistake to believe that pain during pancreatitis and its more complex forms is localized only in the right hypochondrium. Disturbances in the functioning of the pancreas may be accompanied by pain on the right if the head of the organ is affected, on the left if the lesions are located in the tail, and also in the center if the inflammatory process affects mainly the body of the pancreas. Often the pain is radiating in nature: its impact can be felt in the area of the heart, back and even shoulder. Most often they occur in the evening or at night, and intense pain can persist for quite a long time; it subsides slightly if the patient takes a lying position and bends his knees to his stomach and chest. In general, with pancreatic necrosis, pain can vary in severity: in 6% of cases it is moderate pain, in 40% it is acute, in 45% it is severe and unbearable, and in 10% it causes shock.
- The second striking symptom of the onset of destruction of the pancreas is vomiting, which does not bring relief, and at the same time poses a particular danger to the body, because it can cause dehydration. In some patients, not only general exhaustion is observed, but also facial redness, which is explained by an increase in the concentration of vasoactive components. And vice versa, with the onset of a state of collapse, the skin begins to noticeably turn pale. An increase in the level of elastase, which is accompanied by destructive pancreatitis, provokes massive destruction of blood vessels, resulting in bleeding of the digestive organs. Evidence of this is often blue-violet spots that appear on the surface of the skin of the buttocks, the anterior abdominal wall or in the umbilical area.
- The third sign of an aggravated course of the disease is diarrhea; with pancreatic necrosis it is more pronounced, unstable stools become common, the patient suffers from bloating, as well as pain that accompanies this process.
In addition, the disease destructive pancreatitis is characterized by some general symptoms:
- Fever;
- Dyspnea;
- Tachycardia;
- Increased heart rate;
- Yellow complexion and yellowing of the sclera;
- Loss of consciousness.
Diagnostics
Acute destructive pancreatitis does not have a clear clinical picture; its symptoms are similar to those of other forms. As a result, a thorough examination and diagnosis is necessary. If acute pancreatitis is suspected, the patient is taken to the hospital for examination and emergency care.
The purpose of diagnosis is:
- Determination of the phase of the disease and the degree of damage to the body;
- Timely detection of complications;
- Identifying the causes of the disease.
For this purpose, the following is carried out:
- Laboratory tests of blood and urine;
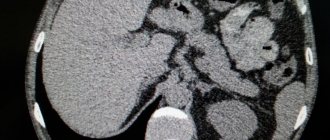
- Ultrasound - to determine the size of the pancreas, study its shape and contours, detect the presence of fluid in the retroperitoneal space;
- X-ray examination - reveals the degree of intestinal bloating;
- Diagnostic laparoscopy - to determine the presence of blood accumulations in the cavity and hemorrhages on the sides of the peritoneum;
- Computed tomography and magnetic resonance imaging help to identify areas of necrosis and determine the condition of other internal organs.
Even a highly qualified doctor will not be able to make an accurate diagnosis only based on the results of a conversation with the patient or an assessment of the existing clinical picture. Any disease requires certain medical studies that will help to accurately determine the nature of the pathological phenomenon.
If the corresponding symptoms are present, one can only assume that the patient has pancreatitis, which is destructive in nature, however, in order to confirm these suspicions, the following diagnostic methods will be needed:
- General blood and urine tests, as well as determination of the level of diastase in the urine;
- Biochemical blood test necessary to determine the levels of amylase, total protein, lipase, creatinine, electrolytes and bilirubin;
- Hemostasiogram - determination of blood clotting, levels of fibrinogen, prothrombin and APTT;
- Ultrasound of the abdominal cavity, in which increased attention is paid to the pancreas, as well as the tissues surrounding it: the presence of swelling and necrotic foci is established, the contours, structure, shape and size of the organ are examined;
- Fibrogastroduodenoscopy - an endoscopic method that allows you to assess the condition of the esophagus, stomach and small intestine - is necessary to exclude diseases of this organ, because the symptoms of pancreatic disorders are very similar to the manifestations of pathologies of other organs of the digestive system;
- Computed tomography is a research method that involves the additional use of X-rays; during this procedure, the image is not planar, as with a regular x-ray, but three-dimensional, which allows you to find out the details and get more information about the pathology;
- Laparoscopy is a minimally invasive operation that is performed using a laparoscope attached to a video camera; during execution, the abdominal cavity is inflated, filling with carbon dioxide, due to which surgeons gain access through a small incision to all necessary organs; Such a diagnosis makes sense to clarify the nuances that, for some reason, remained unclear during the study of the pancreas.
Methods for diagnosing acute destructive pancreatitis in a patient
Important! In order for treatment to be as effective as possible, it is necessary to make a prompt and accurate diagnosis.
When diagnosing the disease, special attention should be paid to patients who have functional disorders of the pancreas.
At the first suspicion of pancreatitis, the patient should be hospitalized immediately.
Attention! The complexity of the disease lies in the fact that disorders that occur in the body can very quickly provoke the development of a coma and other conditions dangerous to the body.
To identify pathological changes, an ultrasound examination of the patient is used, which allows us to identify:
- presence of pancreatic edema;
- progression of necrotic processes;
- uneven structure of organ tissues.
Ultrasound of the abdominal cavity can detect changes in the tissues of the pancreas.
In addition to ultrasound, computed tomography and ciliacography are used.
The most informative examination method is laparoscopy. The use of this method makes it possible to differentiate the diagnosis, to distinguish pancreatic necrosis from cholecystitis, perforated ulcers and some other acute conditions of the body associated with disturbances in the functioning of the abdominal organs.
Treatment
Treatment is carried out in a hospital setting and is aimed at the following goals:
- Elimination of pain;
- Relieving pancreatic duct spasms and inflammation;
- Ensuring stable heart function;
- Removing the effects of intoxication;
- Prevention of inflammatory processes.
Surgical intervention is undertaken if there is no effect from conservative treatment.
Destructive pancreatitis is a serious disease. It is characterized by a high percentage of mortality and disability. To avoid trouble, it is necessary to reconsider your attitude towards alcohol, and also undergo timely examination for other diseases of the internal organs that can provoke an attack of acute pancreatitis.
Treatment of patients diagnosed with destructive pancreatitis is carried out only in a hospital setting. Most often, the patient is admitted to the hospital when the disease is at the first stage, that is, in the presence of toxemia of the body. The first thing the patient faces is washing the stomach with cold water, followed by fasting, which takes at least 3 days, as well as undergoing all tests: both laboratory and instrumental - this is extremely necessary to confirm the etiology of the disease.
When faced with pancreatic necrosis, doctors are always prepared for the most varied developments of events and the first thing they do is direct a set of therapeutic measures to inactivate pancreatic enzymes. If the outflow of bile in the pancreas is disrupted, cleansing is carried out, in addition, painkillers are administered. It is very important to remove cytotoxins and excess enzymes from the body; for this purpose, detoxification is carried out using forced diuresis - intra-arterial and intravenous administration of medications that provoke constant urination.
This is a repeated procedure, in some cases it can last about a week. If the patient’s abdominal cavity contains fluid with bloody impurities, the question of performing laparoscopic dialysis is raised. This method involves installing a drainage through which the pathological contents are drained out. In addition, thanks to such a system, it becomes possible to administer a special solution consisting of the anesthetic drug novocaine, antibiotics and sodium chloride.
The procedure is relevant until the liquid becomes transparent and the concentration of amylase in it decreases significantly. If the intoxication of the body is aggressive and rapidly increases, hemosorption is carried out, that is, blood purification. Provided that the treatment is carried out correctly and the expected results are not achieved, the only possible option is surgery.
Taking medications
In case of destructive processes against the background of pancreatitis, the following medications are prescribed:
- proteinase inhibitors (Aprotex);
- antibiotics (carbapenems, cephalosporins);
- narcotic and non-narcotic painkillers (Baralgin, Analgin, Tramadol);
- antispasmodics (No-Shpa, Spazmalgon, Drotaverine, Papaverine Hydrochloride MS, Sparex, Duspatalin);
- antihistamines (Diphenhydramine-Vial);
- antiemetics (Cerukal, Perinorm);
- detoxification, protein and saline solutions.
Additionally, symptomatic drugs (antipyretics, tranquilizers, dopamine receptor blockers), hepatoprotectors and choleretic drugs can be used.
In acute pancreatitis, any enzymes (Panzinorm, Creon, Pangrol) are contraindicated due to the risk of a dangerous pathological process.
Surgical intervention involves excision of necrotic foci of the pancreas; after its implementation, the patient is prescribed a course of antibacterial drugs, the main role of which is to prevent infection with various types of infections. One of the main components of the rehabilitation period is a therapeutic diet. Non-compliance with dietary nutrition usually does not give positive results in improving health, even if you take medications prescribed by specialists.
In most cases, this pathology requires surgery. It helps restore the outflow of pancreatic juice and eliminate the necrotic area of the organ. The most effective is puncture-drainage treatment.
The operation is also indicated in case of detection of stones, abscesses or cysts.
The patient is given a drainage and undergoes a necrectomy (removal of dead tissue). Resection is rarely required. The method of performing the operation can be puncture, laparotomy (with opening of the abdominal cavity) and laparoscopic (through a puncture). Surgical intervention is carried out no earlier than 5 days from the onset of pancreatitis.
Diet for destructive pancreatitis
Maintaining proper nutrition during inflammation of the pancreas of a destructive nature is one of the components of the treatment process aimed at the recovery of the patient. The diet and what the patient can eat is determined by a gastroenterologist or nutritionist; the emphasis is on foods rich in micro- and macroelements, as well as vitamins - this is necessary for the speedy recovery of the body.
In addition, it is imperative to include in the diet only those foods that are easily digested by the intestines and at the same time do not increase the production of pancreatic enzymes. Preference is given to liquid and pureed dishes. To begin with, it is necessary to exclude from the diet those foods that are strictly prohibited to be consumed during pancreatic necrosis. These include:
- Fatty meats;
- Rich broths;
- Smoked products, sausages;
- Fresh bakery;
- High fat dairy products;
- Fruits and vegetables with a high content of coarse fiber;
- Hot, spicy, fried foods;
- Corn, barley, wheat groats;
- Coffee and strong tea, cocoa;
- Carbonated and alcoholic drinks.
Now let's talk about those dishes and products that, in case of destructive pancreatitis, should form the basis of the diet. These are:
- Oatmeal, buckwheat, rice cereals, from which non-crumbly slimy porridges are prepared;
- Vegetables: carrots, zucchini, potatoes - served only boiled or stewed;
- Lenten baked goods, preferably stale, slightly stale;
- Well-ripened sweet fruits (apricots and peaches, for example);
- Apples of non-acidic varieties, which are preferable to bake or make mousse, jelly, souffle from them;
- Unsweetened and weak tea, jelly, rosehip decoction, dried fruit compote, Borjomi.
There is another group of products that are allowed to be consumed, but in moderate, limited quantities. This category includes:
- Low-fat fermented milk products (cottage cheese, fermented baked milk, sour cream, kefir);
- Dietary meat and low-fat fish - you can use this to make purees, steamed cutlets, etc.;
- Butter, which can be added in small quantities to porridge, or vegetable oil - for adding to first courses;
- Milk soups, which need to be prepared in a 1:1 ratio with water;
- Chicken and quail eggs, boiled soft-boiled; They can also be used to prepare a protein omelet.
Folk remedies
The use of folk remedies in acute destructive processes is prohibited. Any self-medication aggravates destructive processes in the pancreas, increasing the risk of an unfavorable outcome.
Complications of destructive pancreatitis
Untimely therapy and self-medication lead to serious consequences. Complications of destructive pancreatitis are:
- intra-abdominal bleeding;
- transition of the disease to a chronic form with enzymatic deficiency;
- shock;
- hypovolemia (decreased blood volume);
- peritonitis (inflammation of the peritoneum);
- anemia;
- formation of a cavity with a capsule;
- abscess (cavity with pus);
- fibrosis (overgrowth of connective tissue);
- phlegmon (spread purulent inflammation of tissues);
- blockage of blood vessels (portal vein) by a thrombus;
- stress ulcer formation;
- sepsis (blood poisoning).
The most common are purulent complications. They can develop in parallel with tissue necrosis or after 1-2 weeks.