Infiltration after surgery is one of the most common complications after surgery. It can develop after any operation - if you had your appendix removed, a hernia removed, or even just given an injection.
Therefore, it is important to monitor your condition very carefully after surgery. It is quite simple to cure such a complication if it is diagnosed in time. But if you delay it, it can develop into an abscess, and this is already fraught with a breakthrough of the abscess and blood poisoning.
Symptoms of appendiceal infiltrate
The infiltrate develops 2-3 days after the onset of appendicitis, while the clinical picture of acute appendicitis itself is erased - there is no severe pain, general health does not suffer.
Upon examination, a dense, voluminous, painful formation is determined in the right iliac region. Body temperature rises to 38.5 degrees.
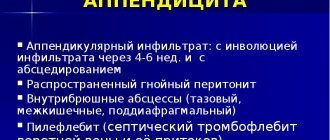
Appendiceal infiltrate has two development paths - abscess formation (suppuration of the infiltrate) and reverse development with “resorption” of the inflammatory tumor.
Abscess formation of the appendicular infiltrate is manifested by an increase in the inflammatory reaction: body temperature rises to 39-40 degrees, symptoms of general intoxication appear, pain in the right iliac region intensifies.
Causes and forms of infiltrates
In order to understand the causes of infiltration, it is necessary to become more familiar with the forms of the condition, of which there are four. The first of them is inflammatory, which forms quite often and may turn out to be purulent, consisting of leukocytes, erythrocytes and other components, forming a tumor. The reasons for the development of this condition are biological fluids that provoke pathogens of infectious conditions, for example, streptococci or staphylococci and others. Also, an inflammatory infiltrate can occur as a consequence of trauma, surgery on the peritoneum, or acute destructive appendicitis.
The next form of infiltration is tumor, which is characterized by the most specific symptoms. Speaking of this, it is strongly recommended to pay attention to the following:
- a change in shade, volume, and density of the tissue cover is formed;
- This infiltrate consists mainly of cells of tumor origin, namely fibroids, sarcomas;
- the development of the presented pathology will be facilitated by factors such as a worsening of the general immune condition, allergic and chronic diseases;
- In this case, it is recommended to start treatment as early as possible because abdominal cancer and other serious complications, such as a tumor, may develop.
Another form that fully explains the reasons is postoperative infiltration. It can form as a result of incorrect drainage or poor hemostasis. The following factors can also influence this and the fact that negative symptoms appear: mechanical damage to tissues, leaving foreign objects and some others. In this case, treatment is also very important to carry out as early as possible.
Causes and treatment of abdominal ascites - why does fluid accumulate?
And finally, the last form of infiltration of the abdominal cavity is appendicular, which is formed as a result of the reaction of the peritoneum to acute inflammatory processes. This provokes such a specific condition as limited peritonitis, which will develop within three days and will be associated with many complications, involving not only the appendix in the process, but also the dome of the intestine, some other areas, even causing a tumor. Speaking about what infiltration is, it will be impossible not to tell in more detail what exactly its symptoms are.
Treatment of appendiceal infiltrate
Abscess formation of the infiltrate is an indication for emergency surgery. In the absence of abscess formation, conservative therapy is carried out in a hospital setting, followed (after 2-3 months) by a planned appendectomy.
Essential drugs
There are contraindications. Specialist consultation is required.
- Ceftriaxone (an antibiotic of the third generation cephalosporin group). Dosage regimen: IM, IV, adults and children over 12 years of age, the average daily dose is 1-2 g of ceftriaxone once a day or 0.5-1 g every 12 hours. In severe cases or in cases of infections caused by moderately sensitive pathogens, the daily dose can be increased to 4 g.
- Cefepime (IV generation cephalosporin antibiotic). Dosage regimen: adults and children weighing more than 40 kg with normal renal function 0.5-1 g intravenously (for severe infections up to 2 g) or deep intramuscularly at intervals of 12 hours (for severe infections - after 8 hours ).
- Metronidazole (antiprotozoal, antibacterial agent). Dosage regimen: IV for adults and children over 12 years of age, a single dose is 0.5 g. The rate of IV jet or drip administration is 5 ml/min. The interval between injections is 8 hours.
- Amoxiclav (broad-spectrum bactericidal antibacterial agent). Dosage regimen: intravenously, adults and children over 12 years of age or weighing more than 40 kg - 1.2 g of the drug (1000 + 200 mg) with an interval of 8 hours, in case of severe infection - with an interval of 6 hours.
- Tienam (antimicrobial, bactericidal, antibacterial agent). Dosage regimen: IV, by infusion: ≤ 500 mg - over 20-30 minutes, > 500 mg over 40-60 minutes. The average daily dose is 2000 mg (4 injections). The maximum daily dose is 4000 mg (50 mg/kg). The dose is adjusted taking into account the severity of the condition, body weight and renal function of the patient.
- Vancomycin (antibacterial, bactericidal agent). Dosage regimen: adults, 0.5 g intravenously every 6 hours or 1.0 g every 12 hours. Infusion duration is at least 60 minutes, rate is 10 mg/min.
Principles of treatment
Treatment of abdominal infiltration is carried out by combining physiotherapeutic and anti-inflammatory drugs. In cases where the purulent type of infiltrate forms phlegmon, surgical intervention is mandatory. And if there is no pus in the infiltration or is present in small quantities, then a physiotherapeutic method of treatment is used, which promotes the resorption of the seal, and an anti-inflammatory and analgesic method to eliminate pain.
Anti-inflammatory therapy is effective in cases of infiltration without pus and promotes normal blood circulation in the compacted area and eliminates congestion.
When it comes to the purulent form, methods with a thermal effect are prescribed only on the fifth day after UHF therapy or SUF irradiation. In this case, antibiotic electrophoresis plays an antibacterial role, and calcium electrophoresis is prescribed to delineate the source of inflammation. Tumor or purulent formations require surgery and the use of a conservative treatment method, including:
- physiotherapy;
- local hypothermia;
- taking antibiotics;
- compliance with bed rest.
Therapy of appendiceal infiltrate is carried out only under inpatient clinical conditions. Antibacterial drugs are usually used, it is important to follow the diet prescribed by the doctor and limit physical activity. This treatment usually requires 2 weeks. To prevent the subsequent occurrence of such symptoms, the doctor recommends surgery to remove the appendix after 3 months.
When the cavity around the appendix is filled with purulent fluid, an operation is performed to extract the pus, but the appendix is not removed. The patient recovers after the appendix is removed several months after surgery to drain the pus.
Incidence (per 100,000 people)
| Men | Women | |||||||||||||
| Age, years | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + | 0-1 | 1-3 | 3-14 | 14-25 | 25-40 | 40-60 | 60 + |
| Number of sick people | 0.01 | 2 | 2 | 2 | 2 | 2 | 2 | 0.01 | 2 | 2 | 2 | 2 | 2 | 2 |
Symptoms
Postoperative complication does not develop immediately - usually on the 4-6th day after hour X (surgical intervention). Sometimes later - after one and a half to two weeks. The main signs of incipient inflammation in a wound are:
- low-grade fever (increases by only a few notches, but it is impossible to bring it down);
- when pressing on the inflamed area, pain is felt;
- if you press very hard, a small pit appears, which gradually straightens;
- the skin in the affected area swells and turns red.
If the tumor occurs after surgery to remove an inguinal hernia, other symptoms may also appear. About a pathological accumulation of cells in the abdominal cavity they will say:
- aching pain in the peritoneum;
- intestinal problems (constipation);
- hyperemia (strong blood flow to sore spots).
With hyperemia, swelling occurs and boils pop up, the heartbeat quickens, and the patient suffers from headaches.
Diagnostic measures
Diagnosis of abdominal infiltration involves identifying the cause, conditions, as well as the period of limitation for the onset of the disease. The following factors can indicate the veracity of the diagnosis: the patient’s body temperature, clear contours of the infiltrate, severe pain when examined with hands, the absence of pus in the compacted part of the body.
During the examination, you should pay attention to the following symptoms:
- mild intoxication;
- the appearance of unexpressed dents when pressed, such signs may well signal the presence of a disease.
Often, purulent foci in the places where the seals are located prevent the diagnosis of infiltration. Using histological examination, the nature and type of the disease can be detected. Infiltration due to appendicitis is determined during examination by a doctor, which does not require special examination. If there is a suspicion of abscess formation, then an echographic examination is mandatory, which can accurately determine the structure of the infiltrate, as well as cystic formations in the form of capsules containing purulent fluid.
Etiology of the phenomenon
Infiltration in the abdominal cavity is mainly a consequence of certain diseases caused by the inflammatory process. Due to the excess content of blood or lymph in the internal organs of a person, the process of accumulation of biological fluids occurs. This kind of fluid may contain blood elements, proteins, minerals, dead cells, and painful microorganisms that cause inflammation in humans. Based on the composition of the liquid, there is the following division:
- serous, fluid from blood serum;
- hemorrhagic, that is, bloody fluid;
- fibrinous, from leukocytes;
- purulent fluid.
There are cases when, if appendicitis is not removed in a timely manner, a tumor with internal inflammation appears, as well as cases where postoperative infiltration of the abdominal cavity is detected several weeks after surgery. In these cases, the cause of the formation of seals is the use of anesthetics, the use of antibiotics, alcohol, etc. Infiltration of the scar can be facilitated by the use of low-quality threads for sutures after operations, even after a couple of years. In cases of spread of malignant tumors, tissues grow and increase in volume, forming a painful tumor infiltrate. Various infectious diseases, characterized by a decrease in the human immune system, can lead to lymphoid compactions of the abdominal organs.
Treatment of the disease
The main goal is to eliminate infiltration. Often this is achieved using only conservative treatment methods. The general principles of treatment for this pathology are as follows:
- bed rest;
- local hypothermia;
- taking antibiotics;
- physiotherapy.
Local hypothermia - cold applied to the peritoneal area - constricts blood vessels, inhibits metabolic processes, reduces the production of enzymes and thus helps stabilize the inflammatory process, preventing its further spread. A course of antibacterial treatment is usually prescribed for a period of 5-7 days. The most commonly used antibiotics are Amoxicillin, Ampicillin, Ceftriaxone, Metronidazole, etc. They are taken simultaneously with drugs that restore beneficial intestinal microflora, for example Linex or Bifiform.
Sanitation of the abdominal cavity in the absence of suppuration and tumors using physiotherapy is very effective. Thanks to electrophoresis with antibiotics, calcium chloride, sessions of laser, electromagnetic or ultraviolet irradiation, pain goes away, swelling subsides, local blood circulation improves and the seal gradually resolves. However, if conservative treatment fails, abscess formation or signs of peritonitis, surgical intervention is required. The abscess is removed using laparoscopic surgery under ultrasound guidance, during which the purulent focus is drained. In case of peritonitis, extensive abdominal surgery cannot be avoided.
After removal of the purulent focus, the abdominal cavity is sanitized with antiseptic solutions of sodium hypochlorite and chlorhexidine. One of the most important conditions for successful treatment is drainage of the abdominal cavity. To do this, several tubes are installed in the latter, through which the exudate flows out (on average 100-300 ml per day). Drains reduce the degree of intoxication of the body and provide early diagnosis of possible postoperative complications: dehiscence of surgical sutures, perforation of organs, bleeding.
Timely drainage of the abdominal cavity, drug and physiotherapeutic treatment of the infiltrate, used in combination, lead to rapid resorption of the formation and provide a favorable prognosis for the patient.
Infiltration of the abdominal cavity is characterized by an unnatural compaction of accumulated blood, lymph, and human cells. This is a section of living tissue, characterized by the existence of cellular elements usually unusual for it, increased in size and with strong density; and sometimes a tissue area infiltrated with some substance introduced artificially: antibiotics, alcohol, anesthetic solutions. Often, the infiltrate appears after a subcutaneous or intramuscular injection, when the main factors for its formation are the following:
- incorrectly chosen injection site;
- administering an injection using a blunt needle;
- performing several injections in the same place;
- using the wrong needle to perform injections, that is, for subcutaneous or intramuscular injections you need to select short needles;
- neglect of the rules of asepsis.
Infiltration is the accumulation of cellular elements mixed with lymph and blood in the tissues of the body. In many cases, an infiltrate in the form of a tumor and inflammation is observed.
The tumor infiltrate is structured from tumor cells of different types and is a manifestation of infiltrating tumor enlargement. When an infiltration seal forms, the tissue changes color, expands in volume, becomes denser, and can become painful.
The inflammatory infiltrate consists of many morphonuclear leukocytes, erythrocytes, lymphoid cells, histiocytes and plasma cells. These types of infiltrates can melt and disappear, but only with the formation of a cavity, abscess or scar. Infiltrate in the abdominal cavity can be of the following types: lymphoid, inflammatory, post-infectious, tumor, postoperative infiltrate.
Causes of lymphocytic colitis
Lymphocytic colitis is a rare form of pathology. The causes of the disease are not precisely known.
Most often, the occurrence of the disease is associated with immunological disorders in the colon mucosa.
It is known that this type of colitis is observed, as a rule, in patients with Sjögren's syndrome, rheumatoid arthritis and celiac enteropathy, i.e. diseases associated with HLA A1 and HLA AZ antigens. A pathogenic effect on the differentiation and formation of fibroblasts of the intestinal microbial flora is also suspected.
The development of microscopic colitis can be provoked by:
- medications that the patient takes in large quantities;
- bacteria that actively multiply in the large intestine;
- excess nutrients.
As a result, the intestinal mucosa becomes inflamed and its basic functions are disrupted. Some sources indicate that lymphocytic colitis is the first stage of microscopic colitis, and collagenous colitis is the second. The disease does not develop into cancer, and neoplasms do not arise.
A genetic predisposition to the disease, as with Crohn's disease, has not been proven.
The function of colonocytes is significantly impaired due to the presence of a large amount of connective tissue. As a result, the absorption of electrolytes and water in the colon is disrupted, which leads to chronic, predominantly secretory diarrhea. The depth of the haustra and the height of the semilunar folds decrease, and the motor-evacuation function of the intestine also decreases. The large intestine takes on the appearance of a tube with smooth walls in collagenous colitis.
- Stage I of the disease (lymphocytic or microscopic colitis) is characterized by a nonspecific inflammatory reaction, which can be manifested by pronounced infiltration of the intestinal wall with lymphoid cells.
- Stage II of the disease (collagenous colitis) differs from the previous one in that a collagen layer is found under the basement membrane of epithelial cells.
Forms of postoperative infiltration
Doctors usually divide infiltration into two forms - inflammatory and tumor. In the first case, lymph and blood particles accumulate in the tissues. This is the most common complication after surgery. However, another form is much more dangerous - tumor, in which not harmless blood and lymph accumulate in the tissues, but actual tumor cells, often malignant. However, sometimes infiltration refers to swelling that occurs at the site of administration of an antibiotic, anesthetic or other drug in liquid form. This infiltration is usually called post-injection or “surgical”.
Diagnostics
The peculiarities of the diagnosis are that the specialist will first listen to the patient’s complaints, perform a palpation examination, examine the skin and mucous membranes, and send for a blood test.
When examining the oral cavity during infiltration, you can notice a white coating on the tongue, indicating intoxication of the body. A person’s breathing becomes unpleasant, the patient complains of digestive upset, he is tormented by vomiting, nausea, and flatulence.
If you press on the abdomen (the area where the appendix is located), mild pain occurs. An elastic, compacted inflammatory tumor is also found here. If the pathological disorders have a stage of purulent softening, then in the infiltrate, in the very middle of the compaction, an area of soft consistency is established.
To clarify and eliminate possible errors in the diagnosis of appendiceal infiltrate, the patient may be prescribed additional examinations:
- Ultrasound of the abdomen and abdominal wall will help determine the diagnosis of acute appendicitis;
- radiography.
It is difficult to detect infiltration if the tumor is located in a non-standard location, as well as if the patient is overweight. When establishing the disease, differential diagnosis is important, which makes it possible to distinguish the tumor from other pathologies with similar symptoms.
Why is infiltration dangerous?
Inflammatory postoperative infiltrate has become almost a common occurrence, because it appears in every 5th operated person. Perhaps this is why to many ordinary people such a complication seems frivolous and harmless. However, this impression is deceptive. With early detection and timely measures taken, it is indeed very simple to eliminate the problem, but if you waste time and do not consult a doctor, the infiltrate can develop into an abscess, which can result in a breakthrough of the abscess and blood poisoning. And this is an extremely dangerous condition that threatens the patient’s life! What can we say about the tumor form of the infiltrate, which can even threaten the patient with cancer. Thus, any symptoms of a developing infiltrate should be immediately reported to the attending physician, who will take all necessary measures to eliminate this dangerous condition and prevent complications.
Treatment of postoperative infiltration
The main task of a doctor faced with an infiltrate is to relieve the inflammatory process and prevent the development of an abscess. In this regard, it is necessary to relieve swelling, restore blood flow in the affected area and eliminate pain.
If the infection is caused by bacteria, specialists prescribe antibiotics, and in addition to them, painkillers and anti-inflammatory drugs. In some cases, physiotherapeutic procedures and local hypothermia (artificial temperature reduction) cannot be avoided. Laser therapy, ultraviolet irradiation of the wound, and even mud therapy are well suited to eliminate infiltration. Such procedures are contraindicated only in one case, when a purulent process has begun to develop in the compaction. In such a situation, heating will only accelerate the spread of infection and lead to an abscess.
As soon as the first signs of an abscess appear, doctors drain the exudate or simply open the abscess using laparotomy or laparoscopy. If the postoperative suture itself is inflamed, the doctors' actions are exactly the same - treatment with antibiotics, the use of painkillers and physiotherapy. If such measures do not help, the suture is opened, cleaned of pus, disinfected and sewn back up.
Symptoms of the disease
The clinical picture of appendiceal infiltrate is less pronounced than the symptoms of appendicitis. The condition is preceded by manifestations of a destructive type of inflammation of the appendix.
Symptoms appear 3-5 days from the onset of the inflammatory process. Typical and atypical clinical course is possible. The patient has the following clinical symptoms:
- Pain syndrome . There is a decrease in pain in the lower right quadrant of the abdomen. The pain does not go away completely. The pain subsides at rest, but reappears with movement. The nature of the pain is dull, aching.
- Dyspepsia . Intestinal paralysis is possible, which is manifested by mild bloating and constipation.
- Intoxication syndrome . Patients report weakness and poor health. A distinctive feature of the pathology is low-grade fever (not higher than 37.4ᵒC). Patients complain of body aches, chills, and dry mouth.
Low-grade fever is of diagnostic value. Appendiceal infiltrate is not manifested by fever. This is explained by the fact that the source of inflammation is held by a conglomerate that has developed around the appendix.
High temperature is not typical for appendiceal infiltration
During diagnosis, it is important to find out the type of pathology (complete, incomplete). Complete appendicular infiltrate, patient reviews:
- Patients note increased heart rate and temperature up to 37.5ᵒC.
- After an exacerbation of appendicitis and its transition to AI, the state of health improves.
- The intensity of pain decreases.
During the examination, with complete AI, the patient’s condition is satisfactory, there is a dry and coated tongue, bloating of the intestines, which is evenly distributed throughout the abdomen. With this type of infiltration of the appendix, there is no muscle tension during superficial palpation of the abdomen. There are also no specific manifestations of appendicitis and peritonitis.
Palpation is an important part of the initial examination for appendicitis
During deep palpation examination of the right iliac region, a dense formation is revealed. It is slightly painful and practically does not move. During a digital examination of the rectum, the lower pole of the conglomerate can be felt. The formation has a dense structure, without signs of liquid.
Incomplete AI is characterized by the following symptoms:
- There are signs of unrestricted peritonitis. The patient's condition is moderate.
- Intestinal bloating, constipation, and lag of the right iliac region in the act of breathing are detected.
- Signs of muscle tension and pain on superficial palpation. The localization of pain does not coincide with the area where the conglomerate is located.
- One or 2-3 symptoms of peritoneal irritation are detected, such as Shchetkin-Blumberg, Mendel; other signs of appendicitis: symptoms of Voskresensky, Sitkovsky, etc.
When diagnosing, all clinical manifestations are taken into account in order to correctly diagnose and prescribe the correct therapy. Errors in the treatment of pathology lead to the development of peritonitis, abscess and other conditions that complicate patient management and worsen the prognosis.
Symptoms: first signs of complications
In the classical course, the onset of the disease coincides with the clinical presentation of appendicitis. From the moment of the first pain in the abdominal area until the formation of an infiltrate, it usually takes 2-4 days. Patients may complain of:
- pain in the right iliac region;
- increased body temperature;
- nausea turning into vomiting;
- difficulty stool.
After the formation of a delimited zone of inflammation, the pain may decrease significantly, but the fever only increases: even with the use of medications, the body temperature rarely drops below 37.8 °C.
Immediately after its formation, the infiltrate is mobile and loose, and its diagnosis is difficult due to significant tension in the abdominal wall. On the 3rd-4th day from the onset of the disease, its main symptom is a palpable, dense, painful formation measuring approximately 8*10 cm.
Without timely treatment, the infiltrate suppurates, and in its place a delimited cavity filled with pus is formed - an appendiceal abscess. In this case, the patient’s condition quickly deteriorates, and the following symptoms appear:
- a sharp increase in temperature;
- chills;
- increased pain;
- severe weakness;
- lack of appetite;
- tachycardia;
- pallor of the skin.
On palpation, an uneven consistency of the infiltrate and local fluctuation are observed - the main signs of limited purulent inflammation.
Post-injection infiltrate
Separately, it is worth mentioning the infiltrate that occurs as a result of the injection, which externally resembles a small lump that appears at the site of drug administration. The reason for this condition is often the lack of professionalism of the medical staff. That is, post-injection infiltrate can occur:
- with improper antiseptic treatment before injection;
- when administering the medicine constantly in the same place;
- when using a needle that is too short or too blunt;
- if the injection site is chosen incorrectly;
- if the medicine is administered too quickly.
Finally, we cannot exclude the fact that some people are predisposed to such mini-complications. In some people, infiltration occurs after each insertion of a needle under the skin, while other people never encounter such a condition in their entire lives.
Causes of postoperative infiltration
The complication in question can develop in any person, regardless of gender and age, for example, in a child after a banal tooth extraction, in an adult man who has had his appendix removed, or in a woman who has had genital surgery. The main reasons for this complication include:
- infection that has entered the wound;
- injuries to the operated area;
- damage to the subcutaneous tissue layer during surgery;
- improper installation of drainage (in overweight patients);
- rejection of suture tissue by body tissues (if the inflammatory process appears several months after the operation, the suture material is to blame).
Other reasons for the appearance of infiltration include allergic reactions of the body, too weakened immunity, as well as chronic or congenital diseases that the person being operated on suffered from.