What is tiflit
Typhlitis is one of the types of segmental colitis , in which the infectious-inflammatory process spreads to the cecum, and when it generalizes, to other parts of the intestine. The disease is accompanied by abdominal pain, compaction of the cecum, colic, severe dyspepsia, intoxication with vomiting and fever.
The disease occurs mainly in adults 24-55 years old who suffer from constipation of any nature . In pediatrics, typhlitis is rarely recorded; it usually complicates the course of oncology and leukemia, aggravates the side effects of certain medications over long-term use, and is secondary in nature.
ICD-10 code – K52 “Other non-infectious gastroenteritis and colitis”.
Pathogenesis
The development mechanism is due to the onset of the inflammatory process as a result of the pathogenic activity of microorganisms. At first, the infection occurs locally, accompanied by swelling of the intestinal walls, vasodilation, and poor circulation.
In most cases, the disease is diagnosed at the initial stage with exudative-catarrhal manifestations. The most dangerous is considered to be a long course of infection with necrotization, ulceration and perforation of the intestinal walls of the cecum.
Chronic typhlitis , characterized by severe autoimmune disorders, constipation, and prolonged infections, is characterized by a decrease in the volume of the exudative component. The changes are more due to necrotization, the appearance of ulcers, persistent coprostasis, and intestinal intoxication.
TYPHLITIS
Typhlitis
(Greek typhlos cecum + -itis) - inflammation of the cecum, segmental colitis.
The occurrence of Typhlitus is facilitated by stagnation of feces in the cecum (see), which favors the development of pathogenic intestinal flora. Typhlitis can develop as a result of hematogenous spread of infection during acute infectious diseases (typhoid fever, sepsis, measles, influenza, etc.). It is also possible for the inflammatory process to transfer to the cecum by lymphogenous route from neighboring organs. Typhlitis may accompany appendicitis (see). With Crohn's disease (see Crohn's disease), intestinal tuberculosis (see Intestines), abdominal actinomycosis (see), ileotiphlitis develops.
Clinical picture
characterized by dull pain in the right iliac region. Sometimes the pain is colic in nature and appears after 5-6 hours. after eating, worsen with movements, prolonged standing, lying on the left side, and can radiate to the lumbar region. There is a feeling of fullness in the abdomen, rumbling, flatulence, nausea, belching, loss of appetite, and sometimes diarrhea (in some cases, in the morning, patients wake up with the urge to defecate - the so-called alarm clock diarrhea). Alternating diarrhea and constipation are more common, but normal stools also occur. During an exacerbation, the abdomen is swollen (sometimes only in the right iliac region), the anterior abdominal wall is not tense, the cecum is compacted, painful, balloon-like inflated, mobile, a tympanic sound is detected by percussion. With ileotiphlitis, a pronounced splashing noise is detected.
Complications include the development of insufficiency of the ileocecal valve - the bauhinium valve (see Cecum), mesadenitis (see) and paratyphlitis - inflammation of the retroperitoneal tissue. Peritiphlitis - inflammation of the peritoneum covering the cecum, can be considered as a complication or as a manifestation of typhlitis. Clinically, it is difficult to distinguish between peri- and paratyphlitis. With peritiphlitis, the pain becomes persistent, the intestine does not move upon palpation.
Diagnosis
diagnosed on the basis of the clinical picture, as well as data from scatological and X-ray examinations. During a scatological examination, a slightly acidic reaction of feces, a large amount of digested fiber, intracellular starch, iodophilic flora, altered muscle fibers, and a small amount of broken down fat are determined. X-ray examination of Typhlitus includes irrigoscopy (see), fluoroscopy with antegrade filling of the ileocecal area, parietography (see). Frequently rentgenol. T.'s symptom is a change in the lumen (enlargement or narrowing) of the cecum. In cases of chyme retention (see) with atony, as well as with kinking of the ascending colon or with a mobile cecum, its lumen is expanded, the liquid and mucus contained in it create a picture of marbling. More often there is a narrowing of the lumen of the cecum, sometimes uneven. With a sharp narrowing, the affected section takes the form of a cord. The altered cecum, especially during the period of exacerbation of the disease, is not densely filled with barium. The structure of the barium column is porous or cellular. The haustra smooth out, take on an irregular shape, and disappear as the process progresses. The contours of the cecum are smooth and clear or finely and coarsely toothed. A characteristic sign of T. is shortening and deformation of the cecum; the edges can take a funnel-shaped or cylindrical shape. The relief of the mucous membrane in T. is changed, has a cellular appearance, folds are often smoothed or absent. In some cases, there are persistent barium stains on the inner surface of the cecum, indicating the presence of ulcers and erosions. An enlargement of the ileocecal valve and insufficient contraction of the cecum during bowel movements are often observed. With double contrast, the border between the cecum and the ascending colon, the narrowing of the cecum, uneven contours, rigidity of the walls, and the cellular or porous structure of the pneumorelief are more clearly determined. With an exacerbation of T., Stirlin's symptom can be detected (see Stirlin's symptom). Peritiphlitis is characterized by deformation, displacement, thickening of the wall of the cecum, its fusion with the abdominal wall and neighboring organs.
Differential diagnosis
carried out with appendicitis (see), secondary changes in the cecum during appendicitis, renal colic (see Kidney stone disease), hepatic colic (see Gallstone disease), gynecological diseases, with malignant neoplasms, right-sided diverticulitis of the colon (see Intestine).
Treatment
etiological and symptomatic. For typhlitis of infectious etiology, antibacterial agents are used. Patients are prescribed a diet, local thermal procedures, intestinal massage, and enzyme preparations for indigestion (see Colitis).
Forecast
favorable with timely treatment.
Prevention
comes down to the prevention of infectious intestinal diseases, timely treatment of constipation (see), sanitation of inflammatory foci in the body, compliance with diet (see).
Bibliography:
Berlin L. B. Chronic colitis, M., 1951; Levitan M.Kh., Fedorov V.D. and Kapuller L.L. Nonspecific colitis, M., 1980; Obraztsov V.P. Diseases of the stomach, intestines and peritoneum, p. 116, Kyiv, 1924; Sahakyan A.G. Postdysenteric colitis, M., 1970; Tashev T. et al. Diseases of the stomach, intestines and peritoneum, trans. from Bulgarian, p. 593, Sofia, 1964; Fanarjyan V. A. X-ray diagnosis of diseases of the digestive tract, vol. 2, Yerevan, 1964; Colenoff L. Rare ileocecal lesions, Amer. J. Roentgenol., v. 110, p. 343, 1970; Hill M. C. a. Goldberg HI Roentgen diagnosis of intestinal amebiasis, ibid., v. 99, p. 77, 1967; Teschendorf W., Anacker H. u. Thurn P. Rontgenologische Differentialdiagnostik, Bd 2, Stuttgart, 1978.
A. V. Frolkie; H. W. Schniger (rent.).
Classification of the disease
The classification includes morphological transformations, etiology, form of the disease , helps determine the diagnosis and draw up an adequate treatment regimen.
According to morphology
Doctors identify the following structural changes in the membranes of the cecum :
- Catarrhal. The cecum swells and swells, which contributes to the narrowing of the lumen. Laboratory tests indicate blood in the stool and changes in the structure of the stool.
- Ulcerative. The mucous membranes are destroyed, areas of ulceration and tissue necrosis are noted. Erosive typhlitis is a complication of the catarrhal form.
Important! The formation of ulcerative lesions increases the risk of perforation and perforation of the intestinal walls, which leads to generalized inflammation.
According to etiological factor
Based on its origin, typhlitis is divided into:
- Infectious (provokers of inflammation - dysenteric amoeba, shigella, tuberculosis bacillus, genital infections).
- Toxic (the cause is due to damage from medications, food, metabolic products of bacteria, fungi).
- Allergenic (occurs as a result of intolerance to certain foods, medications, inflammation begins with irritation of the mucous membranes of the cecum).
- Radiation (typhlitis develops as a complication of radiation therapy for oncogenic tumors).
There is unspecified typhlitis , when the true cause is difficult to establish. Idiopathic forms of typhlitis occur in severe autoimmune diseases.
According to the flow form
The disease is classified into:
- Acute typhlitis with lightning-fast development of a pronounced clinical picture and obvious signs of inflammation.
- Chronic typhlitis - the course is characterized by periods of exacerbation and remission.
Chronization of the infectious-inflammatory process is possible with a prolonged course of acute typhlitis, inadequate therapy, and the addition of serious complications.
Interesting things on the site:
Symptoms of non-ulcerative colitis and methods of its treatment
What is the dome of the cecum and what diseases can there be?
Causes and factors of occurrence
Typhlitis occurs when various agents act on the cells of the mucous membrane of the cecum. Increase the risk of its development:
- intestinal infections;
- dysbacteriosis;
- poor nutrition;
- medications (cytotoxins, antibiotics);
- autoimmune pathologies;
- ileocecal valve insufficiency;
- irritation of the mucous membrane of the cecum with bile;
- violation of intestinal evacuation function;
- chronic stress;
- violation of neurohumoral regulation of intestinal function;
- frequent trauma to the mucous membrane with feces during constipation;
- defect of local immunity of the mucous membrane of the cecum.
Typhlitis is a common condition that occurs against the background of immunodeficiency (including after chemotherapy, a long course of antibacterial therapy, and blood diseases). Occurs mainly in childhood and old age. It is rarely detected in people with intact immunity.
Based on clinical manifestations, it is impossible to accurately establish a diagnosis and determine the cause of the disease.
According to statistical data, such symptoms reveal:
- 60% of cases are tumor and inflammatory diseases of the ileocecal region;
- 10% – dysfunction of the colon;
- 5% – pathologies not related to the ileocecal region (inguinal hernia, adnexitis, etc.).
It is especially difficult to determine the disease only by the nature of the pain. The same pain as with typhlitis is characteristic of appendicitis. And if inflammation of the cecum, especially catarrhal inflammation, which occurs in a mild form, can be treated conservatively, then in case of appendicitis, severe ulcerative lesions of the cecum, urgent surgery is necessary. Therefore, it is imperative to undergo diagnostics.
Causes
The main reason is damage to the intestines by pathogenic microflora. Predisposing factors in the development of the infectious process :
- complications of appendicitis, peritonitis and other inflammatory processes in the peritoneal organs;
- chronic diseases of the gastrointestinal tract;
- side effects of certain medications (hormones, antibiotics);
- lack of food discipline, overeating, alcohol abuse.
Prolonged constipation, strength sports, and acute intoxication of any nature can contribute to the development of typhlitis Pathogenic microflora freely penetrates into the cecum not only from other intestinal sections, but also from nearby organs: the gallbladder, stomach, pancreas.
Typhlitis (inflammation of the cecum): symptoms and treatment methods
Commonly used medications include: Antibiotics. When choosing an antibacterial agent, take into account the sensitivity of the causative agent of typhlitis. As a trial therapy, until the results of bacteriological culture are obtained, broad-spectrum antibiotics are prescribed - cephalosporins, semisynthetic penicillins, aminoglycosides, etc.
Enzyme preparations. Enzyme replacement therapy is indicated for patients in whom the development of typhlitis is caused by malabsorption and maldigestion. In such situations, the administration of pancreatic enzymes improves the digestion of nutrients and normalizes the chemical composition of chyme. Products must be steamed. The main condition is that they should not irritate the intestines.
Jelly and porridge are useful, for constipation - boiled vegetables, compotes, and for diarrhea - white, slightly dried bread, broths made from lean meat. Fruits can irritate the intestinal mucosa, so their consumption is greatly limited. The diet for intestinal inflammation in an adult differs from the diet of a child, which is associated with a different course of the disease. Another inflammation in the cecum is the process in the appendix, which begins when the lumen of the appendix is blocked by foreign bodies, which causes the proliferation of pathogenic microflora in its cavity, swelling of tissues that provoke pain and spasms.
Treatment in this case can only be surgical, otherwise the appendix will burst and life-threatening peritonitis will occur. There is also a chronic form of appendicitis, in which conservative treatment and an appropriate diet are prescribed. Intestinal inflammation, the symptoms of which give a vague picture of the disease, can be mistaken for appendicitis.
The colon is a continuation of the cecum and itself has several subsections. Inflammation of the colon can be caused by an unhealthy diet and a sedentary lifestyle. Although some of the harmful substances are excreted from the body, the bulk of them are absorbed into the intestinal walls and lead to serious diseases such as colitis, sigmoiditis, diverticulosis and others. Treatment is carried out with antibacterial and antiviral drugs. Then the patient is prescribed bifidobacteria and other similar drugs.
If intestinal inflammation occurs, diet and drug treatment are in many cases supplemented by physiotherapeutic procedures.
The intestine is the general name for several sections of the gastrointestinal tract, each of which plays a critical role in the digestion of food. Its functions include the breakdown of food with the help of enzymes to the smallest particles. Therefore, any inflammation, regardless of the cause, is fraught with serious complications. Diet plays a vital role in intestinal inflammation. According to its functions, the intestine is divided into two sections - thick and thin, which are named according to their thickness.
Inflammation in the rectum is called proctitis. It occurs more often due to constipation. It can also be caused by infections, mechanical damage, or poor nutrition.
This disease is very dangerous; it can develop unnoticed and then suddenly manifest itself with acute pain.
Symptoms and signs
The first place with typhlitis is abdominal pain of varying intensity , distension in the abdomen, difficult and painful defecation.
Associated signs of typhlitis:
- rumbling in the stomach, flatulence, increased gas formation;
- hardening of the peritoneal walls, increasing the volume of the abdomen;
- weakness;
- intoxication;
- temperature increase.
At the beginning of the pathological process, patients experience sharp pain in the peritoneum on the right , especially worsening after eating. As it develops, the pain is constant, and you have to take a forced position of the body for relief.
Important! Symptoms of acute inflammation of the cecum resemble appendicitis (inflammation of the appendix), therefore, in case of atypical manifestations, it is important to consult a doctor for differential diagnosis.
Features of the course in children and adults
Inflammation of the cecum in children and adults occurs in the same way , the clinical picture is identical regardless of the gender of the patient.
The only difference is the intensity of the symptoms due to the high pain sensitivity in young children.
Spectrum of manifestations
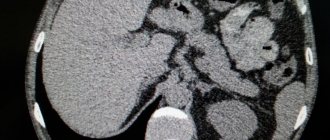
During the acute course of the disease, patients experience chills, repeated nausea and not always productive vomiting, as with appendicitis. Palpation examination of the patient is accompanied by a characteristic rumbling in the navel area. On an x-ray, the cecum is partially covered with contrasting spots and has thickened and slightly displaced walls.
Typhlitis causes the following symptoms:
- Dyspeptic disorders (nausea, frequent belching, heartburn even when following a diet).
- Decreased appetite or complete refusal to eat.
- Discomfort in the lower abdomen. The cecum is located in the right iliac fossa, but pain may be felt in the groin. Typically, cramps occur 2-4 hours after eating, intensifying when changing body position.
- Alternating constipation and diarrhea. Loose stools up to 15 times a day lead to dehydration, and intestinal “clogging” threatens toxemia.
- Nonspecific manifestations of typhlitis are apathy, excessive sweating, dizziness.
- Temperature rises from 38 C and above. Fever is observed during the period of exacerbation of the disease.
Symptoms of typhlitis are determined through scatological examination.
Obvious clinical symptoms of typhlitis are determined through scatological examination. The presence of intracellular starch, broken down fat and a large amount of digested fiber in the feces indicate that the cecum is severely inflamed. If typhlitis is suspected, women need additional examination by a gynecologist and ultrasound of the appendages to rule out ectopic pregnancy or the presence of adnexitis.
Diagnostics
Before treating the disease, a diagnosis is carried out. Its relevance is due to the possibility of serious complications arising as the infectious process develops .
To make a final diagnosis, the following studies are carried out :
- examination, palpation, study of complaints, medical history;
- analysis of stool, urine, blood for differential diagnosis;
- irrigoscopy - X-ray contrast study to assess the structure of the walls of the cecum;
- parietography - instrumental examination of hollow organs with the introduction of liquefied gas;
- Ultrasound of the abdominal organs;
- CT scan.
X-ray and CT signs of typhlitis are clearly defined . There is shortening and deformation of the membranes of the cecum, while its dimensions remain unchanged.
The disease must be differentiated from acute appendicitis, malignant tumors and benign neoplasms of any nature and morphostructure. Typhlitis in appendicitis complicates diagnosis, however, both pathologies are eliminated during surgery.
The diagnosis is made collectively after consultation with a surgeon, therapist, gastroenterologist, and proctologist.
Symptoms
Typhlitis has an acute and chronic course. In acute inflammation, the patient experiences severe pain in the iliac region on the right, radiating to the groin, thigh, lower back, usually an attack develops 1.5–2 hours after eating, fever with chills in case of infection, headache, weakness and sweating.
After some time, nausea, bloating, cramping pain throughout the abdomen, and diarrhea occur. There is usually no vomiting. As the infection develops, copious mucus and blood clots may appear in the stool.
In the chronic course, patients experience moderate cramping pain only when the process worsens. It is provoked by rough food, physical activity, and stress.
Possible complications
A long course of typhlitis leads to dangerous complications caused by the generalization of the inflammatory process and the development of :
- diffuse peritonitis;
- ulceration and perforation of the intestinal walls;
- tissue necrosis, gangrene;
- intraintestinal bleeding;
- abscess.
Associated complications are iron deficiency anemia, persistent disturbances of intestinal absorption and water-salt balance, dysbacteriosis. The high risk of mortality is due to peritonitis, inadequate therapy, and massive bleeding.
Possible consequences and prognosis for life
Untreated typhlitis for a long time is dangerous because the inflammatory process will affect the small intestine, other parts of the colon, and the peritoneum. In addition, other complications may arise:
- intestinal bleeding;
- abscess;
- peritonitis;
- perforation of the ulcer;
- sepsis.
Be sure to read:
Ileocecal valve (Bauhinian valve): concept, location, structure and functions Typhlitus leads to other equally serious consequences. So, with ulcerative hemorrhagic typhlitis, anemia will develop due to frequent bleeding. Inflammatory processes contribute to tissue necrosis and gangrenous changes. Due to the inflammatory process, absorption processes are disrupted, resulting in:
- Iron-deficiency anemia;
- hypo-, avitaminosis;
- hypocalcemia.
If typhlitis is accompanied by diarrhea, vomiting disrupts the water-salt balance.
Typhlitis, especially if it occurs in a mild form, can be treated with conservative therapy if treated in a timely manner. If you follow your doctor's recommendations, a quick recovery is possible. But if complications arise, the prognosis for life is somewhat worse. There is a high probability of death with peritonitis, massive intestinal bleeding, and perforation.
Treatment methods
Symptoms and treatment of typhlitis are interrelated . In mild cases, conservative therapy is limited. Severe cases require emergency surgery. An important aspect of recovery is nutritional correction and physical therapy.
Nutrition correction
Patients are advised to eat a healthy diet : dietary meat, fermented milk products - a source of protein and calcium, pureed vegetables, non-acidic fruits, cereals. It is imperative to maintain a plentiful drinking regime.
Patients should avoid overeating, fresh baked goods, fatty foods, smoked foods, alcohol, carbonated water, and sweets . Meals should be fractional (often and in small portions). Food should be prepared by steaming, boiling or stewing.
Conservative therapy
Medicines are prescribed for any form of typhlitis. A typical drug regimen includes the following :
- antibiotics (cephalosporins, fluoroquinolones);
- absorbents to accelerate the removal of toxins and pathogenic microorganisms;
- laxatives to speed up the excretion of feces and prevent their stagnation;
- anti-inflammatory.
Symptomatic therapy includes the prescription of non-steroidal anti-inflammatory drugs, enzymes, vitamins, astringents, and antispasmodics.
Conservative therapy is often complemented by physiotherapy : thermal procedures, UHF, electrophoresis, massage.
Surgery
Surgical intervention is indicated when conservative therapy is ineffective , as well as when life-threatening complications occur.
There are two main methods:
- Segmental resection with removal of part of the inflamed cecum.
- Extraperitonealization of the dome of the cecum.
The operation is also performed if there is a threat of perforation, perforation of ulcerative lesions, or intestinal obstruction. After this, a long-term rehabilitation program is prescribed.
Traditional methods
Alternative medicine for inflammation of the cecum is secondary in nature and is approved to speed up recovery after relieving life-threatening conditions and preventing constipation. Typically, steep decoctions of chamomile, St. John's wort, and rosehip infusion are used.
Thermal procedures, warming up, hot baths and baths during the period of acute typhlitis are strictly contraindicated , as they lead to an acceleration of the generalization of the infectious-inflammatory process.
What to do with typhlitis and how to distinguish it from other diseases
Pain in the abdominal area often indicates the presence of intestinal diseases. In particular, we are talking about colitis or a disease of the intestinal mucosa. In addition, unpleasant sensations of this nature can occur due to pathogenic microorganisms.
Subsequently, the intestinal mucosa is destroyed. One of the pathologies, characterized by destruction of the mucous membrane, is called typhlitis.
The symptoms of this disease are similar to inflammation of the appendix, so if the pathology is not properly diagnosed, it is easy to confuse it at first.
Typhlitis - inflammation of the cecum
A non-professional examination can lead to a doctor’s decision to perform an operation, confusing appendicitis with typhlitis.
It is necessary to promptly and correctly identify the symptoms of inflammation of the cecum and begin treatment immediately. Otherwise, typhlitis becomes chronic.
It is defined by milder symptoms of a non-acute nature, which are manifested by periodic abdominal pain. The temperature also rises and diarrhea is possible.
The concept of the disease and its causes
Inflammation of the cecum is preceded by problems with the intestines, when feces stagnate for a long time in the cecum. Pathology may appear due to the presence of other diseases, usually of an infectious nature.
There are also cases when typhlitis develops against the background of inflammation of other organs located near the intestines. This pathology can occur together with appendicitis and Crohn's disease.
The development of the disease occurs quite slowly.
The main manifestations resemble signs of poisoning: nausea, headache, deterioration of memory, performance, and weakness.
Identifying the disease is not difficult; the symptoms and treatment of typhlitis are not difficult to determine. The difficulty may lie only in distinguishing typhlitis from inflammation of the appendix.
It is much more problematic to determine the cause of the pathology and understand whether there are concomitant diseases. Treatment should be based on the factors that caused the disease.
Let's consider a number of causes of typhlitis in humans. Typhlitis is similar in symptoms to appendicitis
The main cause of the disease is poor nutrition. Typhlit may occur due to the consumption of large amounts of foods containing coarse fiber. Among them: legumes, nuts, some vegetables.
Food with preservatives and dyes, consumption of smoked, fried and fatty foods also leads to the appearance of typhlitis. In addition, the cause of pathology can be excessive physical activity. For example, when doing weightlifting, typhlitis often develops due to heavy lifting.
These are the main factors. The disease can also occur for the following reasons:
- consequences of appendicitis;
- blood poisoning, which led to damage to internal organs;
- protein intolerance;
- allergic reactions to any food products;
- diseases of the digestive system;
- imbalance of microflora.
Poor nutrition is one of the decisive factors in the development of the disease
Before starting treatment after identifying the disease, you need to get rid of the causes that cause typhlitis. This disease can be distinguished from appendicitis only in laboratory conditions. If symptoms occur, you should immediately consult a doctor. Under no circumstances should you treat typhlitis yourself.
Symptoms of typhlitis
The main symptom of the disease is a dull pain on the left side of the abdomen. May manifest as colic, usually several hours after eating. If you start moving, the unpleasant symptom intensifies. Prolonged position of the body in one state is also accompanied by lower back pain.
The patient feels heaviness and discomfort in the abdomen, and rumbling is possible. Most often you don’t really want to eat, there are problems with stool, constant nausea and weakness. Other symptoms of typhlitis: the abdomen becomes enlarged during attacks, the area of the cecum is especially inflamed, and it hurts to touch it.
In some types of typhlitis, there is a splashing noise in the stomach.
Some complications of typhlitis and symptoms of these diseases are reflected in the table.
DiseasesSymptoms
| Ileocecal valve insufficiency | Diarrhea, abdominal pain, intestinal upset |
| Inflammation of the retroperitoneal tissue | High temperature, rapid heartbeat, lower back and abdominal pain |
| Perityphlitis | Similar to typhlitis, the pain is more severe, the intestine does not move during palpation |
Peritiphlitis and paratyphlitis are often confused, but a specialist can distinguish them by the nature of the pain. These diseases can either accompany typhlitis or act as complications.
Abdominal colic is one of the symptoms of the disease
Diagnostic methods
A diagnosis can only be made after a thorough examination of the patient, as well as after a series of tests. The main ones are x-ray analysis and scatological examination. The latter determines the condition of feces, determines starch, fiber and iodine. An x-ray to detect typhlitis reveals the condition of the cecum.
If the lumen is narrow, then the presence of pathology can be diagnosed. If the intestine takes the shape of a cylinder or funnel, this is a clear sign of the disease. The surface of the mucous membrane also changes during typhlitis. In more advanced forms of the disease, there may be spots on the mucous membrane, indicating the presence of ulcers.
Complications can also be identified in this way: with peritiphlitis, the walls of the cecum are displaced and fused with neighboring organs. Symptoms and treatment of inflammation of the cecum are determined after a thorough examination.
Diagnosis is based on x-rays
Treatment methods
The direction of therapy for typhlitis can be of two types: etiological and symptomatic. The main goal of treating typhlitis is to relieve the main symptoms, usually with the help of medications. Depending on the cause of the pathology, various antibiotics are prescribed. The need to use antibiotics may occur if the following symptoms are present:
- heat;
- frequent gag reflexes requiring medication;
- severe headaches.
When determining infection during inflammation of the cecum, antibacterial drugs are used. Acute typhlitis is treated with Enterofuril and Metronidazole. You should first make sure that you are not allergic to medications. You should get rid of the signs of poisoning and reduce the urge to vomit.
If the disease is accompanied by a high temperature, then antibiotics are prescribed
In addition to antibiotics, for typhlitis a special diet is prescribed, without which treatment will not bring a positive result. Additionally, physiological procedures and abdominal massage are used.
The peculiarity of the chronic type of the disease is periodic attacks of pain during exacerbation. Chronic typhlitis develops with prolonged absence of treatment. In addition to exacerbation of the disease, complications may also appear.
Diet for pathology
A fundamental part of complex therapy is diet. Nutrition for typhlitis includes the use of foods in the diet that maintain a balance of proteins, fats and carbohydrates. It is necessary to refrain from plant fiber. Food should be fresh, not expired and only warm.
Meals should be divided into small portions, but eaten often. It is not recommended to eat nuts, legumes, flour and sweets. The diet is also determined by the patient’s condition and the progress of treatment. Fermented milk products are effective for constipation.
The video shows the identification and treatment of Crohn's disease (another type of intestinal inflammation):
Treatment with folk remedies
Timely diagnosis and treatment usually quickly lead to a positive result.
The use of folk remedies is optional and is not the main part of therapy, however, these methods will help get rid of the disease more quickly and reliably.
The essence of folk treatment is the use of decoctions and infusions from plants: chamomile, sage and others. In case of heavy fecal output, drink onion juice.
Source: https://kishechnik.guru/zabolevaniya/tolstyj-kishechnik/tiflit.html
Prevention and prognosis
The outcome of typhlitis depends on timely diagnosis and treatment . Mild forms of inflammation usually stop quickly, the passage (movement) of feces is restored, and the prognosis is favorable.
A complicated course with generalization of infection throughout the peritoneal organs requires immediate surgical intervention.
Prevention consists of following hygiene rules, monitoring the quality and regularity of stool, creating an adequate diet and maintaining a healthy lifestyle.
Typhlit: treatment and symptoms
Typhlitis is a disease of the cecum, accompanied by progression of the inflammatory process. The pathology is one of the rare ones.
The danger of the problem lies in the possibility of developing complications of the disease with adjacent organs of the abdominal cavity being drawn into the process.
Timely diagnosis and selection of adequate therapy helps to stabilize the patient’s condition while minimizing the clinical picture. The main thing is not to self-medicate and seek help from a doctor.
Symptoms
Symptoms of typhlitis are due to the peculiarity of the pathological process developing in the cecum. Due to inflammation, the function of the epithelium is disrupted, which leads to a deterioration in the absorption of nutrients.
Typical symptoms of typhlitis:
- Loss of appetite.
- Nausea, vomiting.
- Dull pain in the right iliac region with possible migration to the lower back.
- Weakness.
- Emotional lability.
- Headache.
The symptoms of typhlitis are nonspecific, which makes the pathology difficult to diagnose. It is necessary to differentiate the disease with acute appendicitis, cholecystitis and liver dysfunction.
The occurrence of corresponding signs is a reason to consult a doctor for help.