Reactive changes in the pancreas in a child: what is it?
The disease develops according to the following scenario. The pancreas produces enzymes that are used to carry out digestion. They must combine with bile in the bile ducts and then enter the intestines. This is how the digestion process takes place. In case of illness, this system fails. The juice does not pass further and a destructive effect begins inside the gastrointestinal tract. If no measures are taken, diabetes develops or you may end up on the surgical table.
What can lead to illness
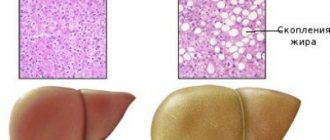
With pancreatitis, a reactive change in the pancreas develops. Reactive pancreatitis is based on inflammation, when swelling occurs and the pancreas increases in size many times over. Changes begin to occur in the parenchymal tissue. In children, the chronic form of the disease is more common. The acute phase may occur if the diet is violated. If a child has diseases of the gastrointestinal tract from birth, an acute form of the disease may immediately develop.
Among the prerequisites for the course of the disease are:
- Infections and colds. It is enough for a child to catch a cold for the pancreas to begin to swell and become inflamed.
- Malfunction of the gland. Difficult release of enzymes. This is facilitated by congenital pathologies, as well as improper formation of the organ itself.
- Genetic predisposition.
- Bruises or injured abdominal organs.
- Allergic reactions.
- Food poisoning.
- Taking strong antibiotics.
In older children, reactive changes are caused by:
- Pathological disorders in the functioning of the esophagus.
- Intestinal ulcers and colitis.
- Acute and chronic forms of hepatitis.
- Chronic cholecystitis.
Diagnostic measures and treatment of changes
In the diagnosis of reactive changes in the pancreas, a survey of patients is used, which helps to detect nutritional disorders, as well as collecting an anamnesis about past and hereditary diseases in order to more accurately establish a diagnosis.
The examination makes it possible to identify the specific localization of pain in the abdominal region, the presence or absence of signs of irritation of the mucous membrane of the organ, as well as detect signs of poisoning or an allergic reaction.
Diffuse changes in the pancreatic parenchyma are certainly diagnosed using a general blood test.
This study can help find signs characteristic of the presence of an inflammatory process: an increase in white blood cells, an increase in the erythrocyte sedimentation rate, a decrease in the number of lymphocytes and hemoglobin.
A coprogram or stool analysis is also often performed: the presence of undigested starch, protein fibers, and an increase in fat particles is noted.
A biochemical type of blood test is aimed at detecting increases in enzyme levels. A urine test reveals an increase in diastase.
Ultrasound examination reveals heterogeneous echogenicity of pancreatic tissue.
Treatment of reactive diffuse changes in severe parenchyma is necessary only in stationary conditions.
The doctor must prescribe strict bed rest. Treatment includes the use of medications and a special diet, as well as eliminating the cause of the disease.
Treatment of reactive changes in the gland parenchyma generally has the following scheme:
- Antispasmodics are used to eliminate abdominal pain. Such medications not only eliminate pain, but also reduce contractions of the gland ducts, thereby facilitating the outflow of digestive juice and beneficial microelements;
- detoxification treatment using intravenously administered solutions;
- taking protease inhibitors;
- treatment of allergies with antihistamines: Tavegil, Suprastin, Allergodil, etc.;
- use of enzyme preparations: Pancreatin, Mezima forte, Festal;
- the use of vitamins and multivitamin complexes: ascorbic acid, Ascorutin, vitamin B.
Treatment of changes in children and adults using this scheme has proven its effectiveness and was awarded a silver medal at an international exhibition for its versatility.
To eliminate diffuse changes in the pancreas, treatment must certainly be accompanied by a diet.
For two days or more, as determined by the doctor, you should not eat any food to ensure complete rest for the inflamed gland.
Video:
On such days, you should only drink highly alkaline, non-carbonated warm mineral water. These waters include Borjomi, Luzhanskaya, Polyana Kvasova, Essentuki, Sairme, Polyana Kupel, etc. The doctor prescribes the required daily dose of mineral water.
It should be remembered that self-treatment of reactive changes in the gland can greatly harm your health.
Signs of the onset of reactive changes in a child
Indirect signs are similar in symptoms to many other diseases. If you are concerned about something in the functioning of your own body, it is recommended to consult a doctor. You can notice that the child has an unstable moral state, a sharp change in mood. Your child is experiencing pain in the abdominal area. Blood sugar levels change dramatically. The baby often swears.
We also recommend viewing: Signs of pancreatic disease in women
In adolescents, the symptoms are clear:
- bloating;
- severe pain in the upper abdomen;
- vomiting or feeling sick. There is no relief after vomiting;
- yellowness of the skin;
- dark shade of urine;
- light-colored feces;
- increased body temperature;
- white or yellow root of the tongue.
Important. In infants, changes are more difficult to determine. There are no obvious symptoms. There is lethargy and loss of appetite.
Causes of changes and symptoms
The causes of reactive changes in the pancreatic parenchyma mainly include infectious diseases accompanied by an inflammatory process (pharyngitis, pneumonia, influenza and others), acute inflammation of the tissues of the gastrointestinal tract (catarrh, gastritis, ulcers), abdominal trauma and various stresses.
Also, the reasons for changes may be irregular or unhealthy diet (frequent consumption of dishes and products containing preservatives and flavor enhancers, carbonated drinks, fast food, chips, etc.), the use of certain medications (these include Trichopolum, Furosemide, antibiotics and other medications).
Separately, it is worth highlighting congenital pathologies of the digestive system: cystic fibrosis, disruption of the bile ducts, reduced levels of lactose and hormones.
Diffuse reactive changes in the parenchyma mainly have the following symptoms:
- pronounced pain in the stomach area of a long-term nature. As a rule, the pain decreases when taking a sitting position with a slight forward bend. When pain appears, the child begins to cry and become restless. Diffuse changes in a child can be diagnosed by the following position: the baby lies on his side, from time to time pressing his legs to his chest;
- periodic attacks of vomiting food and gastric juice, which do not bring relief. With reactive changes, the child may not vomit;
- in the first hours of the disease, body temperature can increase to 38 degrees, in rare cases it can even increase to 40 degrees;
- frequent watery diarrhea. With a long course of the disease, instability of the stool is observed, when diarrhea gives way to constipation;
- the mucous membrane of the tongue is dry with a white or yellowish coating;
- dry mouth;
- decreased or complete lack of appetite;
- frequent belching and bloating;
- increased fatigue, general weakness in the body.
If there are reactive changes in a child, the signs may not be too pronounced. In such cases, making a diagnosis is difficult even for a qualified doctor.
If parents notice several of the above signs in their child or themselves, they should consult a doctor as soon as possible.
Attempts to self-medicate a child without the help of doctors can have negative consequences.
Ways to detect changes
In order to accurately determine the presence of changes that occur in the body, use ultrasound examination (ultrasound). A CT scan is performed to obtain additional information. It is recommended to conduct an examination of the entire abdominal cavity: examine the liver and pancreas.
Additional studies that are recommended:
- Donate blood for a general analysis (this is done to determine the presence of inflammatory processes in the body).
- To determine the amount of enzymes, conduct a biochemical blood test.
- It is recommended to examine the intestinal mucosa near the inlet of the duct.
- Laparoscopy - to more accurately determine the type of deviation.
Important. The doctor, after conducting a comprehensive analysis of the information, will be able to accurately establish a diagnosis and prescribe competent treatment.
Pancreatitis in children
Pancreatitis in children is an inflammation of the tissue and ducts of the pancreas, caused by increased activity of its own pancreatic enzymes.
Pancreatitis in children is manifested by acute pain in the epigastrium, dyspeptic disorders, and fever; in case of chronicity – loss of appetite, unstable stool, weight loss, asthenovegetative syndrome.
The diagnosis of pancreatitis in children is based on the results of a study of blood and urine enzymes, coprograms, ultrasound, radiography, and CT scan of the abdominal cavity. For pancreatitis in children, a gentle diet, antispasmodic and antisecretory therapy, enzyme preparations, and antibiotics are indicated; if necessary, surgical intervention.
Pancreatitis in children is an autocatalytic enzymatic inflammatory-dystrophic lesion of the pancreas. The prevalence of pancreatitis among children with pathologies of the digestive tract is 5-25%.
The course of pancreatitis in a child, unlike an adult, has its own characteristics: the disease can be caused by a wide range of exogenous and endogenous factors, be asymptomatic, and be masked by other diseases of the digestive tract: gastritis, gastroduodenitis, intestinal dysbiosis, etc.
The search for methods for early detection and timely treatment of pancreatitis in children is a pressing task in pediatrics and pediatric gastroenterology.
Pancreatitis in children
The development of pancreatitis in children is caused by the pathological effect on the pancreas of its own activated enzymes (primarily proteases), damaging tissues, excretory ducts and vessels of the gland. Self-destruction of an organ leads to the development of an inflammatory reaction in it, and the release of enzymes and toxic products of tissue breakdown into the blood and lymph leads to severe general intoxication.
Chronic inflammation in most cases is secondary and may be a consequence of acute pancreatitis in children. Manifestation of pancreatitis in children occurs under the influence of various etiological factors of a mechanical, neurohumoral and toxic-allergic nature.
The cause of pancreatitis in children may be a violation of the outflow of pancreatic secretions, which occurs due to developmental anomalies or obstruction of the excretory ducts of the pancreas, duodenum and gall bladder; blunt abdominal injuries; helminthiasis (ascariasis); against the background of gastrointestinal diseases (peptic ulcer, gastroduodenitis, cholecystitis, hepatitis, cholelithiasis); malignant pathology (pancreatic cancer).
Excessive stimulation of the pancreas with an increase in the activity of pancreatic enzymes can develop if the child is malnourished - a violation of the eating schedule; overeating, eating fatty, spicy foods, chips, carbonated drinks, fast food, etc. Severe toxic-allergic reactions to foods and medications (corticosteroids, sulfonamides, cytostatics, furosemide, metronidazole, NSAIDs) lead to the development of pancreatitis in children.
Pancreatitis in children may be associated with connective tissue diseases, endocrinopathies, metabolic disorders (obesity, hemochromatosis), hypothyroidism, cystic fibrosis, chronic renal failure; suffered acute viral and bacterial infections (mumps, chicken pox, herpes virus infection, dysentery, salmonellosis, sepsis).
According to the nature of the course, pancreatitis in children can be acute or chronic. Acute pancreatitis in children is characterized by catarrhal inflammation and swelling of the pancreas; in severe cases - hemorrhages, tissue necrosis and toxemia.
In chronic pancreatitis in children, the inflammatory process progresses against the background of degenerative changes - sclerosis, fibrosis and atrophy of the pancreatic parenchyma and gradual impairment of its function.
For school-age children, a chronic, often latent course of pancreatitis is more common; the acute form is rare in all age groups.
Depending on the clinical and morphological changes in the pancreas, acute edematous (interstitial), hemorrhagic, purulent pancreatitis in children and fatty pancreatic necrosis are distinguished.
Chronic pancreatitis in children can vary in origin (primary and secondary); along the flow (recurrent and latent); according to the severity of the course (mild, moderate and severe forms). Recurrent pancreatitis in children goes through the stages of exacerbation, subsiding exacerbation and remission; latent – not accompanied by pronounced clinical symptoms.
Reactive pancreatitis in children, which develops as a response of the pancreas to various inflammatory diseases of the gastrointestinal tract, can be reversible with adequate treatment of the underlying pathology or turn into “true” pancreatitis, accompanied by destruction of the gland. There is hereditary pancreatitis in children, transmitted in an autosomal dominant manner.
Pancreatitis in children is usually mild; severe (for example, purulent-necrotic) forms are extremely rare. In younger children, the clinical manifestations of pancreatitis are usually less pronounced.
Acute pancreatitis in older children is manifested by sharp paroxysmal pain in the epigastric region, often of a girdling nature, radiating to the right hypochondrium and back. Pancreatitis in children is accompanied by dyspeptic disorders - loss of appetite, nausea, flatulence, diarrhea, and repeated vomiting.
There is an increase in body temperature up to 37 ° C, pallor and subicteric skin, sometimes cyanosis and marbling of the skin of the face and limbs; dry mouth, white coating on the tongue.
With pancreatic necrosis and purulent pancreatitis, children develop febrile temperature, increasing intoxication, intestinal paresis and symptoms of peritoneal irritation, and the development of a collaptoid state is possible.
Symptoms of chronic pancreatitis in children are determined by the duration, stage and form of the disease, the degree of dysfunction of the pancreas and other gastrointestinal organs.
A child with chronic pancreatitis may be bothered by constant or periodic aching pain in the epigastric region, aggravated by errors in nutrition, after significant physical activity or emotional stress. Painful attacks can last from 1-2 hours to several days.
With chronic pancreatitis in children, there is a decrease in appetite, heartburn, periodically - nausea, vomiting, constipation, alternating with diarrhea, accompanied by weight loss; asthenovegetative syndrome.
Complications of pancreatitis in children can include false cyst, pancreolithiasis, peritonitis, pleurisy, and diabetes mellitus.
Diagnosis of pancreatitis in children is based on the clinical picture, results of laboratory and instrumental studies. On palpation of the pancreas, positive symptoms of local pain are noted (Kerte, Kach, Mayo-Robson).
In acute pancreatitis in children, a general blood test shows moderate or severe neutrophilic leukocytosis and an increase in ESR; in a biochemical blood test - increased activity of pancreatic enzymes (lipase, trypsin, amylase), hyperglycemia.
To assess the exocrine secretion of the pancreas, a coprogram and stool lipid profile and determination of elastase-1 activity in the stool are prescribed. The presence of steatorrhea and creatorrhoea in a child is a pathognomonic sign of chronic pancreatitis.
Ultrasound of the pancreas and abdominal cavity can detect an increase in the volume of the organ, the presence of areas of necrosis, as well as compaction and heterogeneity of the parenchyma. Survey radiography of the abdominal organs reveals changes in the organs of the digestive tract and the presence of stones. If necessary, CT and MRI of the abdominal cavity are performed.
Differential diagnosis of pancreatitis in children is carried out with peptic ulcer of the stomach and duodenum, acute cholecystitis, biliary or renal colic, acute intestinal obstruction, acute appendicitis.
Therapy for pancreatitis in children usually includes conservative tactics aimed at functional rest of the pancreas, relief of symptoms, and elimination of etiological factors.
Treatment of the acute phase of pancreatitis in children is carried out in a hospital with mandatory bed rest and a “food break” - fasting for 1-2 days.
Alkaline mineral water, parenteral administration of glucose solution are indicated, according to indications - hemodez, plasma, rheopolyglucin, proteolytic enzyme inhibitors.
After food adaptation, a diet is prescribed that does not stimulate pancreatic secretion and provides mechanical and chemical sparing of the digestive tract.
Drug therapy for pancreatitis in children includes analgesics and antispasmodics; antisecretory drugs (pirenzepine, famotidine), pancreatic enzyme drugs (pancreatin); in severe cases - protease inhibitors (pentoxyl). Comprehensive treatment of pancreatitis in children may include corticosteroids, antibiotics, and antihistamines; drugs that improve microcirculation (dipyridamole, pentoxifylline).
Surgical treatment is performed in case of progression of pancreatic destruction, development of pancreatic necrosis and ineffectiveness of conservative therapy for pancreatitis in children. In this case, the operation of choice may be pancreatic resection, necrectomy, cholecystectomy, or drainage of a pancreatic abscess.
Mild forms of acute pancreatitis in children have a favorable prognosis; with hemorrhagic and purulent forms, as well as pancreatic necrosis, there is a high risk of death. The prognosis of chronic pancreatitis in children depends on the frequency of exacerbations.
Prevention of pancreatitis in children includes rational, age-appropriate nutrition, prevention of gastrointestinal diseases, infectious, systemic, helminthic diseases, and taking medications strictly as prescribed by the doctor. Children with chronic pancreatitis are subject to dispensary observation by a pediatrician and pediatric gastroenterologist, a course of anti-relapse and sanatorium-resort treatment.
Source: https://www.KrasotaiMedicina.ru/diseases/children/pancreatitis
Treatment methods
Treatment consists of several areas:
- elimination of the underlying disease;
- elimination of symptoms (diarrhea, pain, vomiting);
- dieting.
If studies show the presence of pancreatitis and, as a consequence, reactive enlargement of the pancreas, the child is immediately hospitalized.
Types of drugs to treat the disease:
- medications aimed at reducing the production of gastric juice and suppressing the activity of the gland;
- enzyme production agents;
- antispasmodics to relieve pain and promote the outflow of pancreatic juice;
- glucose in the form of a solution to maintain water-salt balance.
Causes
Poor nutrition is a condition for the occurrence of reactive pancreatitis.
Reactive changes in the pancreas are secondary symptoms based on primary factors, such as alcohol, gastritis, cholelithiasis, etc. Reactive pancreatitis occurs for the following reasons:
- long-term use of antibiotics, which was not accompanied by medications intended to restore microflora;
- use of antimicrobial agents;
- abdominal trauma;
- poor nutrition;
- congenital anomalies of the pancreas;
- infectious diseases;
- the presence of pathology in the gastrointestinal tract;
- stressful situations that entail changes in the parenchyma.
Diffuse changes in the parenchyma can occur in obesity, diabetes, and in elderly people. Changes in the parenchyma are mainly affected by poor nutrition and alcohol consumption.
Reactive changes in the parenchyma are formed due to the inflammatory process of the pancreas, which is affected by the liver and gall bladder. As a result, pain appears and blood sugar levels rise.
Return to contents
Diet
An important factor for recovery is diet. Parents must strictly ensure that the child consumes only those foods that the doctor allows. Any deviation will invalidate all treatment and lead to an exacerbation of the disease.
Do not eat:
- fat;
- flour;
- spicy;
- salty;
- smoked meats;
- ice cream;
- soda;
- mushrooms;
- cabbage;
- canned food
We also recommend viewing: Severe pain in the pancreas: what to do and how to treat correctly
What products and in what form are allowed to be eaten:
- eat all steamed dishes;
- food should be warm;
- all food must be ground;
- Divide meals into 5-6 parts in small portions with an interval of no more than 4 hours;
- tea without sugar, pureed cereals, purees, vegetable soups;
- fish, dairy products, lean meat (chicken), steamed cutlets;
- vegetables and fruits should be introduced a week after the end of the acute phase.
Diet in complex therapy of disorders
During the treatment process, you must adhere to the prescribed diet. During the first two to three days, as prescribed by the doctor, any food is prohibited: this creates functional rest for the pancreas. You are allowed to drink alkaline mineral water without gas, weakly brewed tea, compote, jelly. The volume of fluid these days is also determined by the doctor, taking into account the child’s condition.
For the next six days, the diet expands: grated warm food is added in small portions 5-6 times a day.
Prohibited:
- sweets,
- rich meat broths and soups prepared from them,
- canned food,
- fresh fruits and vegetables.
In the future, the list of permitted products increases, but they still need to be thermally processed.
Preventive actions
In the periods between acute attacks, it is recommended to follow a strict diet. Eliminate all harmful foods from your diet. Warn teachers, kindergarten teachers, and doctors that your child should not eat certain foods. It is advisable to provide a list of what is allowed to be eaten or a menu. Warn medical staff in kindergartens and schools that your child has this disease. Be sure to check for diagnosis and dietary information in your child's medical record.
The famous children's doctor E. Komarovsky advises to remember that it is important not to overfeed the baby. Many problems with the pancreas occur due to excess food intake. The child should still have a slight feeling of hunger. It is better to increase the number of feedings to six per day, while reducing the portions proportionally. Overeating is your child's main enemy. Try not to overuse sweet and flour products. In addition to the fact that they are harmful to the figure, they also have a detrimental effect on the functioning of the pancreas.
Treatment is the sure path to recovery
If your child has acquired such a disease, be sure to undergo a full range of studies. Never start therapy on your own. This can harm the baby and worsen the course of the disease. Perhaps the appearance of a disease indicates the presence of a complex problem in the body. A reactive enlargement of the pancreas is a consequence of a malfunction of the whole organism. Eliminating the source of the failure will lead to a speedy recovery. Do not stop treatment under any circumstances if the child feels the first signs of relief. Don't just fight the symptoms. Treatment abandoned halfway will not bring any results and the disease will soon return. If a child does not receive proper treatment and does not take preventive measures, this will lead to dangerous consequences. Reactive changes contribute to tissue destruction due to enzyme stagnation. Over time, diabetes will begin. In the worst case, it will lead to surgery, during which the organ is partially removed.
We also recommend viewing: Options for damage to the pancreas and its treatment
Doctors who repeatedly encounter diseases of this kind note that ensuring a routine and proper nutrition is the key to a child’s good health. By excluding prohibited foods, do not think that you are depriving your child. On the contrary, by doing so you alleviate his condition and protect him from the harm that they will cause to the child. Of course, healthy food is often tasteless, but this is a matter of habit. In the future, the child will be happy to eat all the dishes you prepare.
Psychological aspect
It is important to learn to communicate with your child. Do not exclude him from participation in matters concerning his health. Your task is to educate him on this matter. There is no need to assume that he is too small and will not understand anything, unless he is a baby. Talk to him, explain what is happening to him and how to deal with it. What should he do to always feel good? To avoid scandals due to refusal to buy sweets, explain to your child what the diet is for. Don't follow your child's lead. Strictly adhere to the regime and diet and follow all doctor’s orders. Have explanatory conversations with your child.
Important. He must realize all the consequences of his condition. However, do not cultivate in him the feeling of an eternally sick person. He should live life to the fullest, like other children.
To prevent the development of the disease, undergo annual medical examinations. If you feel any changes in your child’s behavior or well-being, be sure to show him to the doctor. Pay attention to the complaints your child tells you about. By adhering to the recommendations described above, you can achieve a long-term positive effect and not remember reactive changes in the child’s pancreas for a long time. You will be able to provide him with first aid yourself.
Liver pathologies
Changes of this kind in children are observed much less frequently than in adults, but they can pose a greater degree of risk due to the functional immaturity of the organ before a certain age. As in the case of the pancreas, pathological transformations are the result of factors located outside the gland itself, but having a direct impact on its condition.
Aseptic inflammation can be a consequence of variable diseases or disturbances of normal functionality, including a consequence of an infection located in another segment. Therefore, by reactive hepatitis we mean the result of the destructive action of inflammation occurring outside the liver, affecting its structural segments.
Depending on the main provocateur, reactive changes in the liver can affect its vascular network and parenchyma. In this case, more significant damage is possible. In a child, reactive changes can progress quickly and lead to serious consequences. The reason for this will be the immaturity of the exocrine gland. But there are much fewer reasons for the development of pathology in a child than in an adult - such statistics are explained by more careful monitoring of the baby’s condition and the absence of chronic diseases.
In this case, jaundice appears slightly or is absent altogether. Pain symptoms and dyspeptic symptoms are not much different from other liver pathologies. The course of changes can also be asymptomatic, and laboratory tests reveal only subtle deviations - the presence of bilirubin fractions and liver transaminases. No structural changes were found in the parenchyma.