Briefly about the rectum
The rectum is the final organ of the intestinal tract. It is located in the pelvic cavity, its length is 15 - 20 cm. Its wall consists of several layers: internal (mucous membrane), middle (muscular layer) and external (connective tissue membrane). Outside the rectum there is pararectal tissue (adipose tissue). In the place where the rectum passes into the anal canal, there are depressions in the form of sacs (crypts), at the bottom of which the ducts of the anal glands that produce mucus open. They play an important role in the development of paraproctitis.
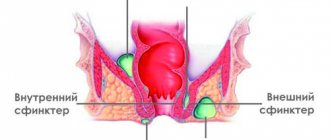
Rice. 2. Anatomy of the rectum. Pararectal tissue is indicated in yellow.
Causes of the disease
The root cause of the development of paraproctitis is infection. In most cases, a polymicrobial flora is recorded with the obligatory presence of Escherichia coli and other intestinal pathogens. Streptococci, staphylococci and Proteus are often found in the microbial flora.
Paraproctitis, caused by anaerobic flora (exists in oxygen-free conditions), is extremely difficult. In this case, putrefactive paraproctitis, gas phlegmon of the pelvis and anaerobic sepsis develop.
Of the specific infections, the most common are syphilis, tuberculosis and actinomycosis, accounting for 1 - 3% of the total disease.
Chronic paraproctitis: causes of disease development
The development of paraproctitis begins with an acute inflammatory process, the causative agents of which are bacteria: staphylococcus, enterococcus, Escherichia coli and anaerobic bacteria. Microorganisms that enter the fatty tissue through cracks or damaged areas of the rectal mucosa cause a pathological process, as a result of which the excretory ducts are blocked.
The process of secretion production by the rectal glands does not stop, so in their place cysts with pus are formed, the contents of which come out of the fatty tissue. The causative agents of the disease can be transported through the bloodstream into fatty tissue from another source of inflammation. The development of chronic paraproctitis may be due to the following factors:
- regular constipation and anal fissures;
- formation of hemorrhoids;
- diabetes mellitus;
- decreased immune response of the body;
- vascular atherosclerosis.
Chronic paraproctitis, surgery for which is one of the effective methods of treatment, is often diagnosed in patients who self-medicated during an exacerbation of the disease and did not seek help from a coloproctologist. Doctors of the highest category, doctors and candidates of medical sciences working at the Yusupov Hospital use the achievements of modern medicine to restore the health of patients and improve their quality of life.
When contacting coloproctologists at the Yusupov Hospital, patients receive high-quality medical care on conditions of anonymity, professional care, and also have the opportunity to stay in a comfortable hospital and undergo rehabilitation under the supervision of experienced specialists.
Predisposing factors
Acute paraproctitis always develops against the background of weakening of the body's immune system, which is facilitated by diabetes mellitus, the presence of foci of chronic infection, including the anorectal area, systemic diseases, including leukemia, neurological pathology, alcoholism, Crohn's disease, ulcerative colitis, etc.
- In most cases of paraproctitis, the entry points for infection are the anal crypts and glands.
- The infection penetrates into the perirectal tissue through the lymphatic vessels during proctitis, hemorrhoids, ulcers and anal fissures.
- The disease can develop with osteomyelitis of the pelvic bones, phlegmon of the gluteal regions, perineum and scrotum, paraurethral abscesses, parametritis, bartholinitis, inflammation of the Cooper glands.
- Microtraumas of the rectal mucosa that occur during the use of instrumental examination methods, hemorrhoids, anal fissures, ulcers and strictures contribute to the development of paraproctitis. The mucous membrane can be injured when inedible objects pass through the rectum - fruit seeds, cereal awns, fish and beef bones.
- Paraproctitis occurs with gunshot wounds and puncture wounds in the anus.
- Tears in the mucous membrane that occur during repeated violent attempts to throw out feces contribute to the development of the disease.
Rice. 3 and 4. Rectal fissures and hemorrhoids are common causes of paraproctitis.
Etiology edit edit code
E. coli is predominant
. In the etiology of paraproctitis, the introduction of infection into the pararectal tissue is of leading importance.
Ways of introduction of infection into pararectal tissue
The infection can penetrate through the anal glands, damaged rectal mucosa, hematogenously and lymphogenously, from neighboring organs affected by the inflammatory process.
A number of researchers consider paraproctitis to be a fairly common complication of nonspecific ulcerative colitis and Crohn's disease.
Purulent processes in the cellular spaces around the rectum are observed in diseases of the prostate gland, urethra, paraurethral, Cooper's glands, female genital organs (perimetritis, bartholinitis), sometimes with osteomyelitis of the pelvic bones, tuberculosis of the spine.
Ways of spread of the inflammatory process
The spread of infection during paraproctitis comes from the rectum. The entrance gates are the anal crypts, where the ducts of the anal glands open, or (much less often) the damaged mucous membrane of the anal canal. First, a crypt becomes inflamed, where the internal opening of the fistula is formed. Then the infection penetrates through the ducts of the anal glands into their branches, which are localized in the submucosal or intermuscular layers. When an infection penetrates through a damaged intestinal mucosa, its further spread is possible through interstitial crevices, as well as through lymphogenous and hematogenous routes. Due to the looseness of the submucosal layer of the intestine, ulcers in this localization easily and quickly spread upward, peeling off the mucous membrane. Streaks of pus, spreading along the vascular branches, penetrate into the intermuscular spaces between the circular and longitudinal layers of the muscles of the intestinal wall.
Spreading along the branches of the anal glands and destroying them, pus penetrates into the pararectal tissue spaces (submucosal, subcutaneous, ileoprectal, pelvic-rectal and retrorectal). Depending on the degree of virulence of the flora and the reactivity of the organism, the process can be limited to one area or spread throughout the tissue of neighboring anatomical areas.
When the purulent process spreads, the conditions of outflow also matter. If the abscess drains well through a wide connection with the intestine or has access to the skin, one can expect minimal damage to the cellular spaces of the pelvis. If there are no such conditions, many purulent passages may form around the rectum with leakage into various cellular spaces. Breakthroughs of the abscess onto the skin in various areas (external fistula openings) are possible. With paraproctitis, fistulous openings on the scrotum, thigh, and anterior abdominal wall are described. In addition, the possibility of an abscess breaking into the intestinal lumen at the level of the ampullary section and even into the abdominal cavity cannot be ruled out.
Causes of chronic disease
Modern researchers consider acute and chronic paraproctitis as stages of one disease. In previous years, the question of why a rectal fistula (chronic paraproctitis) so often forms after opening acute paraproctitis was widely discussed.
Chronic factors
- The internal opening of the fistula (the mouth of the infected one or more anal glands, covered with an epithelial lining, opening in the Morganian crypt) is a source of constant or periodic infection of the perirectal tissue.
- The presence of a formed fistula tract, single or branched, located superficially or deep in the pelvic tissues. Healing is hampered by epithelization of the walls of the fistula tract, which prevents their collapse and leaves the lumen open to reinfection. The inner surface of the fistula tract is lined with granulation tissue or glandular epithelium.
- Activation of a dormant surgical infection. The infection can remain in the tissues of the body for a more or less long time without causing disease (latent phase), but then, under the influence of various factors, it manifests itself in the form of acute paraproctitis (active phase). With paraproctitis, the focus of a dormant infection may have a morphological substrate. They are either scars at the site of an opened abscess, or a remnant of a fistula tract, or an unlaced, unopened leak.
How the disease develops
The infection penetrates into the perirectal tissue through the anal glands and crypts, damaged mucous membrane, through the lymphatic tract and hematogenously. The spread of infection is controlled by a strong immune system. So, the infection does not always penetrate through the damaged mucous membrane into the perirectal tissue, but is stopped in the submucosal layer, where a submucosal abscess develops.
Penetration of infection most often occurs through the anal glands and crypts. The posterior crypts are most often involved in the development of the infectious process, where in most cases the openings of pararectal fistulas open.
The inflammatory process develops like phlegmon. Under the influence of adequate and timely treatment and with sufficient body resistance, the inflammatory process is stopped and turns into an abscess, which is opened either independently or surgically. The inflammatory process in the perirectal tissue develops slowly with tuberculosis, actinomycosis, coccidioidomycosis, syphilis and with suppuration of dermoid cysts.
Rice. 5. In the photo there is acute paraproctitis.
What is paraproctitis
The pathology is an inflammatory process in the perirectal tissue (it surrounds the rectum). The main causes of the disease are failure to comply with the rules of personal hygiene, injuries in the anal area, leading to infection of this area. The presence of diseases of the rectum (hemorrhoids, anal fissures) is important; they can provoke chronic paraproctitis, which leads to the formation of fistulas.
The cause of the pathology can be any source of chronic infection in the body, especially in cases of weakening of a person’s defenses (observed in the presence of severe concomitant diseases).
Paraproctitis is manifested by severe pain in the perineal area, which intensifies when trying to perform an act of defecation . This leads to constipation.
When palpating the area of inflammation, patients notice sharp pain; the boundaries of the accumulation of purulent contents can be determined.
The general condition of patients also worsens - body temperature rises, there will be complaints of weakness, apathy, and dizziness. Such patients experience dyspeptic symptoms - nausea, vomiting, lack of appetite.
As the disease progresses, it may result in the formation of a fistula. A channel with purulent contents is formed, which connects the intestinal cavity with the environment. In such situations, treatment requires more serious and extensive surgery.
Classification
According to the nature of the course, paraproctitis is divided into:
- Spicy.
- Chronic (including recurrent).
According to etiology:
- Non-specific (banal).
- Specific.
By type of pathogen:
- Aerobic.
- Anaerobic, including clostridial and non-clostridial.
According to the localization of foci of suppuration:
- Superficial abscesses: subcutaneous (56%), submucosal (2 - 6%), subcutaneous-submucosal.
- Deep abscesses: ischiorectal or ischiorectal (34 - 39%), pelvic-rectal or subperitoneal (8%), retrorectal (1 - 2%).
According to the location of the internal opening of the fistula tract:
- Front.
- Rear.
- Lateral.
In relation to the fistula tract and the sphincter fibers:
- Intrasphincteral (subcutaneous-submucosal).
- Transsphincteral (transsphincteric).
- Extrasphincteral (I - IV degrees of complexity).
According to the nature of the fistula tract:
- Complete (have internal and external fistula openings connected to each other by a purulent tract).
- Incomplete internal (do not have an exit to the outside - on the skin).
- Incomplete external (do not have an outlet in the rectal wall).
Rice. 6. Types of paraproctitis. The location of the abscess is important during surgical treatment.
Signs and symptoms of acute paraproctitis
Of all the localizations of paraproctitis, the most common are subcutaneous. Their share is about 56%. The infection process develops rapidly.
The most characteristic symptoms of the disease:
- Increasing pain in the rectum and anus, worsens when walking and coughing.
- Body temperature rises, headache, malaise, apathy, and weakness appear and increase. The general condition of patients especially worsens with deep abscesses - pelvic-rectal and ischiorectal abscesses.
- There is retention of stool, but at the same time gases pass unhindered, sometimes diarrhea.
- In some cases, urinary retention.
Signs and symptoms for superficial ulcers:
- Redness and hyperthermia of the skin over the abscess.
- Local swelling.
- The appearance of pain during examination of the rectum and palpation of the perianal area. The pain is jerking and worsens with straining, defecation, coughing and walking.
- Violation of the act of defecation.
- Body temperature is very high with chills.
Signs and symptoms for deep ulcers:
- Weak expression of local signs.
- The pain is diffuse.
- The localization of the abscess is difficult to identify. Skin redness and fluctuation are often absent.
- Severe symptoms of intoxication, high body temperature - reaches 38 - 390C.
- Difficulty in defecation and urination.
Rice. 7 and 8. In the photo, superficial paraproctitis.
Signs and symptoms of submucosal ulcers:
- The pain is mild, intensifying with defecation.
- The general condition remains satisfactory. Body temperature rises slightly.
Rice. 9. In the photo there is submucosal paraproctitis.
Signs and symptoms of ischiorectal ulcers:
- The general condition of the patient is serious. Body temperature rises significantly. Signs of intoxication are pronounced.
- The pain is severe, localized deep in the pelvis, pulsating, aggravated by straining, defecation, coughing and walking.
- If the abscess is located in front of the rectum, urination disturbance is observed.
- Asymmetry of the buttocks, skin hyperemia and infiltration appear on the 5th - 6th day of the disease.
Signs and symptoms of pelviorectal ulcers:
- The course of the disease is the most severe of all types of paraproctitis. The disease develops gradually over 10 to 12 days. Then the patient's condition begins to deteriorate sharply. The focus of suppuration is formed on the 7th - 20th day. Body temperature rises to 40 - 410C. Symptoms of intoxication are significantly expressed.
- The abscess is located deep in the pelvis, which is why patients complain of pain in the lower abdomen.
- Painful tenesmus appears.
- Urination is impaired.
- When the tissue melts, redness and swelling of the tissue in the perineal area occurs.
Signs and symptoms of rectal ulcers:
- The pain is severe in the rectum and sacrum, intensifies during defecation, when pressing on the tailbone, in a sitting position, and radiates to the thighs.
Subcutaneous paraproctitis
This form of the disease is characterized by the location of a purulent focus in the fatty tissue directly under the skin.
Upon visual inspection, a swelling of a characteristic red color is noticeable around the anal canal. Any touch, as well as an attempt to sit down or defecate, causes a sharp, throbbing pain. In addition, the patient complains of symptoms of general intoxication, namely:
- Temperature reaching 39 °C.
- Chills.
- Bad feeling.
- Decreased appetite.
- Pain in muscles, joints and bones.
Since this problem causes severe discomfort and literally interferes with normal life, most men immediately consult a doctor. Making a diagnosis is not difficult - a survey, visual examination and palpation are enough.
Outcome and complications of acute paraproctitis
- Breakthrough of the abscess outward, cleansing of the suppuration cavity and healing.
- In cases where the fistula has not formed and the source of inflammation remains in the area of the intersphincteric space and anal glands, relapses of the disease occur.
- Penetration of bacteria into the abscess cavity through fistulous tracts, which supports the inflammatory process - transition to the chronic fistulous form.
- Breakthrough of an abscess into the fatty tissue of the pelvis, followed by purulent melting of the wall of the rectum and/or ureter in men, vagina - in women. When purulent masses break into the abdominal cavity, peritonitis develops.
Rice. 10. The photo shows chronic paraproctitis in a child under 1 year of age
Possible complications
Delayed consultation with a doctor, as well as irrational treatment of acute paraproctitis can lead to a number of complications, including:
- necrotic lesion of the rectal wall;
- spread of purulent masses to neighboring organs, leading to their melting;
- entry of feces into the fistula passage and the wall of the rectum with the occurrence of infectious inflammation;
- spread of purulent inflammation to the pelvic area and abdominal cavity (peritonitis).
Prolonged course of paraproctitis can lead to such undesirable consequences as insufficiency of the anal sphincter, scar formation, deformation of the walls of the rectum.
Signs and symptoms of chronic paraproctitis
Chronic paraproctitis often occurs due to spontaneous opening of an abscess or improper treatment (opening) of acute paraproctitis.
The disease progresses in waves: periods of well-being are followed by periods of exacerbation. When the fistula tract closes, pus again accumulates in large quantities. The patient's condition worsens. After another opening and discharge of pus, the patient’s general condition improves. Gradually the fistula begins to close, but the disease continues to exist.
During periods of exacerbation, the following signs and symptoms are recorded:
- Discharge from the fistula tract (pus, mucus, gases, feces) is scanty.
- The pain syndrome is not clearly expressed.
- The general condition suffers. The patient develops insomnia, irritability, headache, and decreased performance.
With chronic paraproctitis, the following types of fistulas are formed:
- Full. They have two outlets: on the skin and the rectal mucosa.
- Incomplete. They have two holes: one ends blindly in the form of a “bag”, and the other is functioning.
- External. The hole goes out and is located on the skin.
- Internal. The hole comes out inside the rectum on the mucous membrane.
There are complex fistulas that connect the rectum to nearby organs - the vagina (rectovaginal fistulas) and the bladder (entero-urinary).
Rectal fistulas
Rectal fistula is a chronic inflammation in the anal crypt, pararectal tissue or intersphincteric space with the formation of a fistula tract. Fistulas, as a rule, form against the background of improper treatment or spontaneous opening of an abscess during acute paraproctitis.
How the disease develops
A fistula that spontaneously opens inside the rectum often heals on its own, but with a fragile scar, which can reopen due to injury - cycling, constipation, etc. During the next healing, pus accumulates again, and an abscess can form in another place. The same thing happens when an abscess is opened incorrectly, when the fistula opening, which is constantly infected with intestinal flora, is not eliminated. Over time, connective tissue forms around the fistula tract, and in the fatty tissue, with insufficient drainage, purulent infiltrates and cavities form.
Only 1/3 of patients seek medical help in a timely manner, another third of patients turn to doctors only after self-opening of the abscess, the remaining third - after opening of the abscess and the formation of chronic paraproctitis.
Rice. 11. Breakthrough of the abscess outward during paraproctitis.
Signs and symptoms of the disease
- Discharge from the rectum of ichor, pus and particles of feces, which is why patients have to use pads and wash frequently.
- When the fistula tract is blocked by granulation tissue or purulent-necrotic masses, pus again accumulates in the perirectal tissue or intersphincteric space. The appearance of new abscesses occurs against the background of a deterioration in the general condition of the patient. Patients are worried about headaches, weakness, decreased performance and potency, and mental health problems. Pain appears in the perineal area. There is stool retention and difficulty urinating, and tenesmus occurs.
Complications
- With the long-term existence of chronic paraproctitis, against the background of the development of scar tissue, severe local changes are formed in the form of deformation of the lumen of the rectum and perineum, which causes insufficient retention of feces and gases.
- Malignancy of fistula tracts.
- Development of amyloidosis of internal organs.
Diagnostics
Diagnosis of the disease is not difficult. First of all, the internal opening of the fistula tract and its direction to the fibers of the anal sphincter are identified. However, with unsuccessful operations in the past, this procedure turns out to be complex and requires qualified diagnostics.
Rice. 12. Fistulas in chronic paraproctitis.
Rice. 13 and 14. In the photo on the left is an external fistula opening in chronic paraproctitis, on the right is deformation of the anal canal and multiple fistulas.
Classification of paraproctitis according to ICD 10
The following sections are distinguished in the international classification of diseases.
ICD 10 code for acute paraproctitis is K 61.0. Name: anal abscess . Depending on the location of the pathological formation in a given zone, it is divided into rectal (K 61.1), anorectal (K 61.2), ischiorectal (K 61.3) and intrasphincteric (K 61.4).
The first subtype is characterized by the fact that the abscess is located in the rectum, the second - around the anus. If an abscess forms in the ischiorectal fossa, this is an ischiorectal form of the disease.
If a pathological formation is found directly on the anus, an intrasphincteric abscess is exposed.
The clinical picture of acute paraproctitis is described above. General intoxication phenomena are more pronounced than in the chronic form of the disease.
Some clinicians use the name purulent paraproctitis. With any acute inflammation of this area, a pathological secretion is formed. Therefore, the ICD 10 code for purulent paraproctitis is K 61.0. Patients should know that these forms of the disease are identical to each other.
In cases where the disease is not treated, the inflammatory process drags on and becomes chronic . Such situations are characterized by the formation of a fistula between the rectum and the external environment.
Patients will complain of purulent discharge that constantly stains their underwear, causing discomfort. The pain syndrome is not pronounced, it is disturbing during periods of exacerbation. The general condition of the patients is better than in the acute form of the disease; no significant intoxication is observed . But gradually patients become irritable, it is difficult for such patients to concentrate, and their performance decreases.
ICD 10 code for chronic paraproctitis is K 60.3. It is called an anal fistula and belongs to the heading K 60.0 - fissure and fistula of the anus and rectum.
Other codes related to chronic paraproctitis in the international classification are as follows: K 60.4 (rectal fistula) and K 60.5 (anorectal fistula). The first implies the formation of a pathological canal only within the anus, the second - between the intestinal cavity and the anus.
Diagnosis of the disease
Diagnosis of paraproctitis is carried out on the basis of patient complaints, medical history, and objective examination data. You should consult a gynecologist (women) and a urologist (men) to exclude complications of acute paraproctitis.
External inspection
Due to their pain, rectal abscesses are easily detected by external examination and palpation. An external examination is carried out to identify hyperemia, edema and detect a painful infiltrate or fluctuation in the area of the abscess.
Rectal examination
This type of examination is the main one if acute paraproctitis is suspected. With its help, the functional state of the anal canal and rectum is assessed, the presence of infiltrates, leaks and concomitant diseases is determined. A digital examination reveals areas of pain, and sometimes pus is discharged during the examination.
Rice. 15 and 16. Carrying out a digital examination of the rectum.
Anoscopy and sigmoidoscopy
Anoscopy and sigmoidoscopy examination is carried out using a special instrument.
- Using anoscopy, the lower ampullary section of the rectum and the anal canal are examined - to a depth of 8 to 10 cm from the edge of the anus.
- Using sigmoidoscopy, it is possible to examine the rectum and the distal sigmoid colon - to a depth of 15 to 20 cm from the edge of the anus.
Rice. 17 and 18. Disposable anoscopes and sigmoidoscope.
Rice. 19 and 20. The photo shows the process of sigmoidoscopy.
Probing the fistula
Probing of the fistula and aspiration staining of its cavity with a mixture of methylene blue and hydrogen peroxide is carried out to determine the position in relation to the wall of the rectum, the nature of the internal relief, and the detection of additional branches and cavities.
Rice. 21 and 22. Probing the fistula and dye test.
Fistulography
Fistulography is an x-ray examination. With its help, the location and size of the purulent cavity, the direction of the fistula tract and purulent pockets are determined.
Rice. 23. When performing fistulography, a radiopaque substance is injected into the fistulous tract.
Endorectal ultrasound examination
The effectiveness of this research method is 80 - 89%. With its help, the localization and structure of the source of inflammation, additional fistula tracts, and the degree of involvement of the rectal wall and muscle fibers of the external sphincter in the pathological process are determined.
Bacteriological research
Using the bacteriological research method, the nature of the microflora and its sensitivity to antibiotics are determined. This technique is used for delayed surgery and to determine the type of immunostimulating therapy.
Differential diagnosis
Acute paraproctitis should be distinguished from an abscess of the pouch of Douglas, a suppurating keratoma and a disintegrating tumor.
Diagnostics
For a preliminary diagnosis, the proctologist only needs data from a survey, examination and physical examination. Characteristic clinical signs: fever, local soreness, symptoms of purulent inflammation. Due to the extreme pain of the procedures, digital examination of the anus and methods of instrumental diagnosis of proctological diseases (anoscopy, sigmoidoscopy) are not performed. A blood test reveals signs of purulent inflammation: leukocytosis with neutrophilia, increased ESR. Acute paraproctitis mainly has to be differentiated from suppurating teratoma of the peri-rectal tissue, tumors of the rectum and surrounding tissues, and abscess of the pouch of Douglas. The need to carry out additional research to differentiate paraproctitis from other diseases usually arises in the case of a high location of the abscess (in the pelvis or ileorectal fossa). Chronic paraproctitis is diagnosed by examining the perineum, anus, and performing a digital examination of the anal canal. If a fistula is detected, its course is probed. As instrumental diagnostics, sigmoidoscopy, anoscopy, fistulography are used - if the fistula is located high, there is copious discharge and voting (oscillation) of the probe occurs in the canal. Ultrasonography is also used. A formed pararectal fistula must be differentiated from a perirectal tissue cyst, osteomyelitis of the terminal parts of the spine, tuberculous fistula, epithelial coccygeal tract and fistulas in patients with Crohn's disease. For the differential diagnosis, anamnesis data, laboratory tests, and pelvic radiography are significant.
Treatment of acute paraproctitis
Treatment of acute paraproctitis is mainly surgical. Conservative treatment is used in the earliest stages of the disease, when surgical treatment is contraindicated in elderly patients and during preparation for surgery.
Surgical treatment
The main method of treating acute paraproctitis is surgical. Its goal is to open the abscess as early as possible and remove purulent masses; otherwise, the purulent process can quickly spread throughout the pelvic tissue, destroy the muscular structures of the pelvic floor and sphincter, as well as the walls of the rectum.
Before surgery, it is necessary to determine the exact location of the abscess, purulent tract and the affected crypt.
Contraindications to radical surgery are the inability to identify the affected crypt, severe inflammation of the surrounding tissues and the patient’s severe somatic condition.
During the operation, a wide opening of the abscess, revision and sanitation of the postoperative wound are performed.
There are 2 types of surgical treatment:
- Radical instantaneous.
- Multi-stage. Is the most appropriate. At the first stage, the abscess is opened and an adequate outflow of purulent masses is created, the second stage (subsequent radical surgery) is carried out 5 - 7 days after the severity of inflammation has subsided.
Conservative treatment
Sometimes acute paraproctitis in the stage of beginning infiltration can be cured only with the use of conservative therapy, the basis of which is antibacterial treatment. Conservative treatment is used in elderly people who have contraindications to surgery, as well as in preparation for surgery.
In addition to the administration of antibiotics, lumbar novocaine blockades and a local novocaine-streptomycin block are used. For deeply located foci of suppuration, medications are administered from the rectum, and for subcutaneous abscesses - from the skin.
At an early stage of development of inflammation with deeply located ulcers without tissue softening, the following are indicated:
- During the day - sitz baths once a day for 15 minutes for 2 weeks, a heating pad and medicinal enemas 2 - 3 times a day using a solution of Colimycin, Protargol or Collargon, Ichthyol or Rivanol.
- At night - warming compresses for the perineum.
Treatment
The main treatment method for acute paraproctitis is surgery. Conservative therapy can reduce inflammation and stop the proliferation of pathogenic microorganisms, but does not radically eliminate the cause.
Operational
The main surgical method for eliminating acute paraproctitis is excision of the abscess, washing the purulent cavity with an antiseptic solution and then draining it.
Acute purulent paraproctitis, which opened spontaneously with the formation of a fistula tract, is eliminated in the following ways:
- excision of the fistula: after a thorough diagnosis and determination of the exact localization, the pathological tract is completely excised from the tissues surrounding it;
- ligature method, in which the fistula is gradually tied up with a special thread until it is completely dissected;
- laser coagulation, which involves exposing the fistula to an infrared ray until it is completely scarred;
- the use of fibrin glue, which is injected into the pathological tract, completely blocking its lumen; This method is the least traumatic.
Conservative
Drug treatment of paraproctitis is aimed at eliminating the unpleasant symptoms of the disease, as well as preventing repeated suppuration in the wound.
Medicines
In the postoperative period, patients are prescribed the following medications:
- analgesics;
- anti-inflammatory drugs;
- antibacterial drugs locally (for washing the postoperative wound) or systemically (if indicated);
- sitz baths with the addition of herbs that have anti-inflammatory, bactericidal effects (calendula, chamomile, etc.); such procedures must be performed after the wound has healed once a day for two weeks;
- ointments with an antibacterial effect for topical use (Levomekol).
An important point of conservative treatment is daily dressings, which are carried out after treating the wound with antiseptic solutions, such as furatsilin, potassium permanganate.
Physiotherapy
Physiotherapeutic treatment methods are most often used in the postoperative period. This method helps reduce inflammation, accelerates tissue regeneration, and also has some bactericidal effect.
The main physical therapy treatment options are:
- irradiation with infrared rays;
- Ural Federal District;
- magnetic therapy;
- exposure to ultra-high frequencies;
- electrophoresis.
Important! It is necessary to treat paraproctitis using physiotherapeutic methods only after the acute inflammatory process has subsided.
Treatment of chronic paraproctitis
In chronic paraproctitis, a fistula is formed between the rectum and surrounding tissues, which occurs when an abscess spontaneously opens or improper treatment (opening) of acute paraproctitis. Treatment of fistulas is only surgical. Its goal is to eliminate the primary fistula tract and purulent pockets. Radical surgery with preservation of normal function of the anal sphincter muscles leads to a complete cure. In complex cases, when excision affects a small group of anal sphincter muscles, control over bowel retention is lost. During the operation, concomitant diseases such as hemorrhoids, anal fissures, etc. are also removed.
There are several surgical techniques:
- Excision of the fistula along its entire length, followed by suturing of the wound.
- Excision of the outlet (fistula) followed by plastic surgery.
- Closing the hole using biomaterials.
- Cauterization with laser.
- Ligature application.
- If the sphincter muscle fibers are deeply damaged, they are sutured.
During the rehabilitation period the following is carried out:
- In the postoperative period of radical surgical treatment and after the first stage of multi-stage treatment, patients undergo daily dressings using hydrogen peroxide and alcohol- or iodine-based antiseptics.
- Ointments that accelerate tissue repair (Methyluracil) and have an antimicrobial and anti-inflammatory effect (Methyluracil + Chloramphenicol) are used locally until the wound heals.
- Physiotherapeutic treatment (Ural irradiation + microwave therapy).
Conservative treatment methods include:
- Microclysters with collargol and sea buckthorn oil.
- Washing fistulas with antiseptic solutions.
- Introduction of antibiotics into the fistulous tract.
Rice. 24 and 25. The photo shows chronic paraproctitis. A fistula tract has been identified.
Disease prognosis
With timely seeking medical help and adequate (correctly performed) radical treatment, the prognosis is favorable.
During surgical treatment in cases where the connection between the abscess and the intestinal lumen has not been eliminated, the prognosis is unfavorable due to the formation of a rectal fistula or the occurrence of relapse of acute paraproctitis.
In terms of prognosis, the fact of a long course of the disease and severe concomitant pathology is unfavorable.