Perforation of the intestine (perforation) is the formation of a through hole in its wall with the release of contents into the abdominal cavity. Pathology develops against the background of intestinal disease or as a result of abdominal trauma. Intestinal perforation causes purulent inflammation of the peritoneum (peritonitis) and without surgical intervention leads to the death of the patient.
Symptoms
Intestinal perforation is an acute condition; the patient usually names the exact time of onset of symptoms. The clinical picture of the disease includes two successive stages: primary shock (the first 6 hours after perforation) and peritonitis.
Primary shock stage
Changes in the body according to the mechanism of development resemble shock. Intestinal contents spill into the abdominal cavity, irritating and damaging the peritoneum.
- intense cutting pain, which is initially localized in the perforation area, then spreads throughout the abdomen;
- shallow breathing;
- abdominal muscle tension;
- cold sweat;
- decrease in blood pressure.
Stage of peritonitis
The sensitivity of the nerve endings of the peritoneum is impaired, the bacterial flora of the intestinal contents leads to purulent inflammation in the abdominal cavity.
- pain becomes less intense;
- dry mouth, thirst;
- repeated vomiting;
- bloating;
- fever;
- weakness.
The clinic depends on the location and size of the defect. The higher and larger it is, the more pronounced the symptoms. Perforation of the duodenum is the most acute and severe.
It happens that a small hole in the intestinal wall is covered by a lobe of the liver or a strand of omentum. The contents of the intestine stop flowing into the abdominal cavity, and the pathological process is limited. The patient's well-being improves. Subsequently, an abscess forms at this site.
Intestinal perforation. Classification, patient management methods, prognosis
Perforation can occur in both the small and large intestines
The intestine is a collective concept. Symptoms of the pathology develop acutely, but may differ from the location of the ulceration. In this case, there is always severe pain and other signs of shock.
The diagnosis is established using instrumental methods. A distinctive diagnostic sign is the presence of free air in the peritoneal space. There are:
Perforation of the small intestine Perforation of the large intestine
Therapeutic tactics for perforation of any area of the intestine are as follows:
Surgical intervention without options Antibiotic therapy Infusion of drugs, blood, plasma depending on the severity of the patient
The prognosis for recovery depends on the severity of the injury, the patient’s condition before, during and after surgery, and the degree of penetration of intestinal or stomach contents into the peritoneum. The likelihood of death is extremely high.
Causes
- Duodenal ulcer. Ulcer perforation is one of the most serious complications of the disease. It is more common in men aged 30-40 years.
- Tumors. Ulceration and disintegration of intestinal tumors leads to perforation in the affected area.
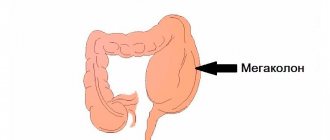
- Nonspecific ulcerative colitis is a chronic disease in which multiple ulcers form in the colon. Intestinal perforation is possible with exacerbation of pathology and toxic expansion of the intestine (megacolon).
- Crohn's disease is a severe autoimmune lesion of all parts of the intestine. Granulomatous inflammation and ulcers develop in the intestinal walls.
- Diverticulitis is an inflammation of diverticula - hernial protrusions of the colon. Violation of the structure, thinning of the wall contributes to perforation.
- Intestinal obstruction. In the late stage of the disease, intestinal necrosis develops and rupture is possible.
- Foreign bodies . Bones with sharp edges, needles, and nails, when moving through the digestive tract, can damage its walls. If a foreign body is accidentally swallowed, seek medical attention.
- Abdominal injuries – knife and gunshot wounds, closed injuries.
- Iatrogenic causes - perforation during diagnostic and therapeutic procedures: rectoscopy, colonoscopy. Complications occur when there are pronounced changes in the wall of the organ or removal of polyps.
Diagnostics
Patients with suspected intestinal perforation should be immediately taken to a surgical hospital.
History taking and examination
The doctor makes a diagnosis based on the following clinical data:
- acute onset of the disease, typical symptoms;
- the presence of a disease that can lead to perforation;
- grimace of pain on the patient's face;
- the tongue is dry, with a white coating;
- stationary position, lying on your back or side, legs brought to your stomach; trying to change position increases pain;
- the stomach is board-shaped, does not participate in breathing;
- on palpation – muscle tension, severe pain, symptoms of peritoneal irritation;
- when auscultating (listening) the abdomen - a sharp weakening or absence of peristalsis.
Laboratory methods
- Complete blood count - with peritonitis, the number of neutrophilic leukocytes and ESR increases.
- General urine analysis - high relative density, traces of acetone.
- Blood biochemistry – electrolyte disturbances, increased acute phase parameters.
Instrumental methods
- A plain radiograph of the abdomen is the main method for diagnosing intestinal perforation. In 80% of cases, the x-ray reveals gas that has entered the abdominal cavity through a hole in the wall of the organ. The study is carried out in a standing position or lying on the left side. In case of perforation against the background of intestinal obstruction, the fluid levels are visible in the image - the Kloiber cup.
- FGDS - prescribed if the result of radiography is negative. Using endoscopy, an ulcerative defect is identified and its condition is assessed. If the abdominal pain intensifies after air injection, a repeat radiograph is taken.
- Computed tomography (CT) - a series of images reveals free fluid and gas in the abdomen, a perforation.
- Ultrasound - detects fluid and gas outside the intestines, abscesses.
- Diagnostic laparoscopy is a mini-surgery, endoscopic examination of the abdominal cavity through small incisions in the abdomen. Upon perforation, exudate is revealed.
Treatment
In case of intestinal perforation with peritonitis, emergency surgery is indicated; the only contraindication to it is the patient’s state of agony. The earlier surgery is performed, the better the treatment results and prognosis.
If perforation is limited, the patient’s condition is satisfactory, and an infiltrate of up to 4 cm in size has formed, conservative treatment is carried out.
Surgery
The operation is performed under general anesthesia. At the preparation stage, the stomach is emptied using a tube. After a laparotomy (an incision in the abdomen), an opening is found in the intestine. The scope of intervention depends on the location of the lesion, the time from the onset of the disease, the patient’s condition, and the doctor’s qualifications.
Operation techniques
- Excision of the ulcer is carried out when the defect is localized in the duodenal zone and there is no diffuse peritonitis. The ulcer and the pylorus of the stomach are removed within healthy tissue, sutured, plastic surgery of the pylorus and vagotomy (dissection of the vagus nerve) are performed.
- Suturing of the intestinal defect is carried out when the diameter of the hole is no more than 5 mm, the edges of the ulcer are soft and the duration of the disease is up to 6 hours. A double-row suture is applied in the transverse direction. If the hole is localized on the anterior wall of the duodenum, laparoscopic surgery is possible.
- Bowel resection with anastomosis is performed when there is perforation of the small intestine. The affected area is excised, the sections of intestine are connected (anastomosis is performed).
- Bowel resection with colostomy is performed when the colon is perforated. The affected area is removed, and a piece of intestine is brought out onto the abdominal wall. The patient will have to use a colostomy bag for several months. The colostomy is then sutured and anastomosis performed.
An important stage of surgical treatment for perforation is washing the abdominal cavity from intestinal contents. Drains are placed to drain exudate from the peritoneal cavity.
Recovery period
In the postoperative period, diuresis and drainage discharge are monitored. If the patient’s condition is satisfactory, early activation is recommended to prevent complications. After recovering from anesthesia, patients are advised to freely extend and bend their arms and breathe deeply; a day later - get up and do breathing exercises.
Nutrition and fluid:
- on the second day after surgery, you are allowed to drink (no more than half a glass per day);
- by day 4, increase the volume of liquid to 4-5 glasses per day: jelly, tea, broth, compotes, vegetable decoctions;
- on day 5 add pureed liquid porridge, cottage cheese, slimy soups;
- after a week, pureed rabbit, turkey, and veal are introduced into the diet.
Further diet is prescribed depending on the underlying disease and the extent of the operation performed.
If the recovery period is smooth, the sutures are removed after 8-10 days. The duration of inpatient treatment is 14-15 days.
Drug therapy
Drug therapy is carried out for the purpose of preoperative preparation, stabilization of the patient’s condition, and to prevent complications in the postoperative period.
- Infusion therapy - solutions are administered for detoxification, restoration of hemodynamics, and electrolyte balance. Main drugs: Hemodez, Ringer's solution, Ringer-Locke, Dextrose, Reopoliglucin.
- Antibiotics are means to fight infection. A wide range of drugs and their combinations are prescribed: cephalosporins, aminoglycosides, fluoroquinolones, imipinemes.
- Cardiac glycosides – drugs for the treatment of heart failure; Strophanthin and Korglikon are administered intravenously.
- Painkillers are means to combat pain. For 3 days after surgery, narcotic analgesics (Promedol) are prescribed, then Analgin + Diphenhydramine.
- Respiratory analeptics - used in the postoperative period to stimulate the respiratory center: Sulfocamphocaine, Cordiamine.
- Cholinesterase inhibitors . To activate intestinal motility, the drug Proserin is prescribed.
What is intestinal perforation called?
This pathology is extremely dangerous. It develops as a result of a violation of the integrity of the mucous membrane and the intestinal wall itself. This condition is also called intestinal perforation. In other words, a through hole appears in its wall. Through it, feces and intestinal juice enter the abdominal region from the intestines. This provokes peritonitis. If the situation is not dealt with in time, the patient may die.
Types of disease
Depending on the location of the perforation, perforation of the large and small intestines is distinguished. Each of these cases has its own reasons. Perforation of the colon is considered the most dangerous. In any case, the problem can only be solved by surgery. Pathology occurs even among newborns. If you notice its symptoms, call a doctor immediately.
Complications, possible outcomes
After surgery for intestinal perforation, complications are possible:
- Pneumonia is inflammation of the lungs due to decreased ventilation with low physical activity of the patient.
- Abdominal abscesses are purulent complications associated with insufficient sanitation of the abdominal cavity, resistance of the bacterial flora to antibiotics, and decreased immunity.
- Impaired motility of the digestive tract - gastrostasis, intestinal paresis, manifested by vomiting and lack of stool.
- Failure of sutures is associated with an infectious process, suppuration.
The results of treatment depend on the duration of the disease, the size of the perforation, the age of the patient, and the presence of concomitant pathology. Postoperative mortality for intestinal perforation ranges from 1.3 to 19.4%, and with the development of purulent peritonitis reaches 30%. Causes of death: postoperative complications and decompensation of chronic diseases.
If you consult a doctor within the first 6 hours after intestinal perforation, the prognosis is favorable. In the future, patients should be monitored by a gastroenterologist.
In continuation of the topic, be sure to read:
- Causes of bloating and increased gas formation, treatment methods
- Rectal cancer: symptoms, stages, treatment and prognosis for life
- Rectal fissure: causes, symptoms and treatment of pathology
- Details about bowel cancer: stages, symptoms, treatment and prognosis
- Details about intestinal colonoscopy: preparation and procedure
- More about hemorrhoids: causes, symptoms and treatment methods
- Irritable bowel syndrome: symptoms and treatments
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Peritonitis: what kind of disease is it, how does it manifest and be treated?
- Proctosigmoiditis: how is the pathology manifested and treated?
Forecast
Survival rates for gastric perforation can be determined after symptoms are identified. Only time can tell the doctor how effective the treatment will be. Indeed, during inflammation and before surgery, such a disease can develop in different ways and at different speeds. The patient's age and the presence of other concomitant diseases are also taken into account.
Doctors report that up to 50% of patients can survive after surgery. Successful surgery is not a guarantee of recovery.