Tummy problems in children under one year of age are quite common. The cause of this symptom may be dysbiosis - an imbalance of microflora in the intestines. This is caused by the immaturity of the gastrointestinal tract, non-compliance by the breastfeeding mother with diets, intestinal infections, change of environment, artificial formulas, etc. With dysbacteriosis, the baby experiences flatulence, abdominal pain, bloating, and regurgitation of sour milk. Along with this, tearfulness, irritability, poor sleep, and appetite are noted. It is these signs that are the reason to prescribe a stool test for intestinal dysbiosis. Learn more about how to take it, prepare, what the study shows, what is the norm, and in what cases the baby needs medical attention.
For what symptoms is a dysbacteriosis test prescribed?
It is worth noting that dysbiosis is not considered a separate disease, it is a combination of pathological and functional disorders. A doctor can recognize an imbalance of intestinal microflora by the following signs:
- disruption of the defecation process - the baby has too frequent stools of a liquid consistency or has not had them for a long time;
- uncharacteristic appearance of feces for his age - the presence of mucus, impurities;
- the baby’s tummy is hard and swollen;
- the baby vomits curdled milk with a sour smell immediately after eating;
- skin rash;
- disruptions in the gastrointestinal tract associated with taking antibacterial drugs;
- weakening of the body’s protective functions against the background of frequent infectious diseases;
- poor appetite.
Parents should be observant and notice uncharacteristic symptoms in time.
What methods are used to detect dysbacteriosis?
The doctor suggests taking the stool first for a general analysis, which is called coproscopy or scatology. It is carried out by microscopying a drop of feces diluted with distilled water.
- slime;
- elements of inflammation;
- undigested dietary fiber;
- red blood cells;
- fatty inclusions;
- worm eggs;
- cystic form of parasites.
There is no exact count of the number of bacteria. In the results, it is important for the doctor to register disturbances in the digestive process. In order to clarify the cause, a biochemical or bacteriological additional study is prescribed.
Biochemical method
Biochemical analysis of stool for dysbacteriosis allows you to get results within an hour. The method is based on the ability of bacteria to secrete fatty acids. By analyzing the type of acidic content, microorganisms are distinguished and localization in the intestine is determined.
The advantages of the method are:
- comparative speed;
- the possibility of extending the delivery time to the laboratory to a day;
- safety of the material when frozen in the refrigerator;
- accuracy of information.
For correct collection, in contrast to the scheme already given, it is necessary:
- provide for a period after antibiotic therapy of at least two weeks;
- women should refrain from taking the test if their periods have not completely ended;
- pick up pieces of feces from different parts.
The acid content is determined in mg per g of feces. The following indicators are considered acceptable:
- acetic acid 5.35–6.41;
- propylene 1.63–1.95;
- oil 1.6–1.9.
Based on the concentration of fatty acids, a conclusion is drawn about the possible composition of microorganisms in the intestine.
Bacteriological culture method
Bacteriological culture of stool for dysbacteriosis is a more labor-intensive research method. The analysis should be carried out as soon as possible after defecation.
Bacteria multiply within 4–5 days. How much dysbacteriosis analysis is done determines the time required for the growth process. They are much larger than in biochemical research, because it is required not only to calculate a quantitative indicator, but also to identify microorganisms by their properties. Results are reported in CFU/g (colony forming units).
The normal distribution of microorganisms should correspond to the following scheme:
- bifidobacteria 10 8 –10 10;
- lactobacilli and Escherichia 10 6 –10 9;
- streptococci 10 5 –10 7;
- non-hemolytic staphylococci 10 4 –10 5;
- clostridia 10 3 –10 5;
- conditionally pathogenic enterobacteria 10 3 –10 4 ;
- hemolytic staphylococci less than 10 3 CFU/g.
The number of bacteria in children under one year old during breastfeeding differs from adults:
- bifidobacteria make up 10 10 –10 11;
- lactobacilli 10 6 –10 7 .
The disadvantages of the method are:
- significant distortion of results depending on the delay in delivery of material;
- lack of accounting for mucosal bacteria found in the colon;
- death of anaerobic microorganisms from contact with oxygen.
How to test for dysbiosis in infants
Analysis for dysbacteriosis involves conducting research in three stages.
- Examination of stool using a coprogram. The analysis reveals the degree of maturity of the newborn’s digestive system, that is, its functional state. Also, using a coprogram, the presence of parasites and impurities (blood, pus, mucus), indicating the presence of an inflammatory process, is determined. It will take the laboratory technician 1 day to get the result. The study is carried out using a high-resolution microscope.
- Sowing for opportunistic microflora. Biological material (feces) taken from the baby is placed in a nutrient medium favorable for growing colonies of microorganisms. This is necessary if the number of pathogenic microorganisms in the stool is so small that it cannot be microscopically recognized. Cultivation lasts 5 days. Using culture, you can identify the type of pathogen and diagnose acute intestinal infections.
- Antibioticogram. Using this study, it is possible to determine the degree of sensitivity of bacteria to the effects of antibacterial drugs and bacteriophages (viruses that selectively infect bacterial cells).
The reliability of the test for dysbacteriosis depends on the correct collection of feces from the baby.
Taking a stool test
The danger of dysbacteriosis lies in the fact that its course cannot always be determined by characteristic signs, since this pathology does not manifest itself in any way. In rare cases, dysbiosis is accompanied by symptoms that can easily be mistaken for another disease. If you have the slightest suspicion of the development of dysbiosis, you should immediately consult a doctor for a diagnostic examination.
Nutrition before submitting stool for analysis
Preparatory stage
If you are prescribed this procedure, then approximately 2-3 days before the analysis you need to review your diet, excluding fermented milk products that contain bacteria, spicy, salty, smoked and fried foods. Drinking alcoholic beverages is also prohibited, as this may affect the test results. Doctors do not recommend taking laxatives or antibacterial drugs during the preparation period. The material for research, which was obtained by performing a cleansing enema, is unsuitable for laboratory analysis. Correct adherence to all doctor’s instructions is the key to a quality procedure.
Laxatives should not be taken
Stool collection
As soon as the preparatory stage is completed, it is necessary to proceed directly to the collection of stool for laboratory analysis. A special container is suitable for this, which you can buy at your nearest pharmacy. Alternatively, you can use other containers that have been sterilized (treated properly and at high temperature). After filling the container, close the lid, thereby preventing the entry of air (when exposed to air, some types of microorganisms may die). Do not allow urine to enter the container as this may adversely affect the test results.
How to properly collect feces
There is no need to fill the container to the brim; 10 mg of stool will be sufficient . Be sure to make a note on the container, writing the date of collection, time, and your first and last name. This must be done with a dark marker, since not all containers have a special paper tag on which you can write data with a regular pen. No more than 4-5 hours should pass from the moment of bowel movement to the time of analysis, so try not to delay your visit to the clinic.
Stool collection technology
Transcript of laboratory research
After a successful analysis, the attending physician will begin to decipher the results. Depending on the age of the patient, analysis standards may vary. All the necessary information is in the public domain, so anyone can familiarize themselves with it in advance.
Table. Interpretation of analysis indicators.
| Microflora | Description |
| Candida | A type of fungal infection that is a key component of human intestinal microorganisms. Candida does not have a negative effect on the organs of the gastrointestinal tract and the digestion process itself, but its increased activity can provoke the development of thrush (candidiasis). |
| Clostridia | Gram-positive pathogenic microorganisms that belong to the group of anaerobic bacteria. They are contained in the intestinal microflora and are actively involved in the process of food digestion. |
| Enterococci | Gram-positive bacteria that help normalize stomach acidity. They participate in fermentation processes, thereby negatively affecting the functioning of the digestive system. Their danger lies in the fact that enterococci are incredibly tenacious and have increased resistance to various antibiotics. |
| Bacteroides | Gram-negative anaerobic bacteria belonging to the rod-shaped group. Their main function is to digest carbohydrates, fats and proteins. |
| Escherichia | Escherichia coli, which lives in the healthy microflora of the human intestine. Its action is to suck oxygen from the small and large intestines. Escherichia also participates in the synthesis of beneficial vitamins. |
| Lactobacilli | Gram-positive lactic acid pathogenic microorganisms that participate in the process of breaking down lactose in the body before its further digestion. Helps normalize the patient's intestinal acidity. |
| Bifidobacteria | They are considered one of the most important representatives of the intestinal microflora. Their task is to protect the human body from the negative effects of pathogenic microorganisms. The development of dysbacteriosis is indicated by a decrease in the number of bifidobacteria. |
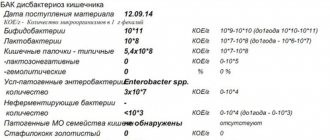
Example of decoding results
Even though you have been diagnosed with dysbiosis, you should not immediately panic. This disease is completely curable; it is enough to follow all doctor’s instructions, take prescribed medications and dietary supplements (dietary supplements). Throughout the entire therapeutic course, the patient must also follow a special diet , which consists of excluding from the diet all harmful foods that negatively affect the digestive system.
But it will not be possible to begin treatment without making an accurate diagnosis, so the patient must have his stool tested for dysbacteriosis. Based on the data obtained, the doctor will be able to determine which drugs are best suited in this case. Only the right approach and timely treatment will allow you to cope with the signs of pathology in the shortest possible period.
Treatment of dysbiosis
How to properly collect material for analysis - useful tips for parents
How to get tested for dysbacteriosis? Before conducting a study, a number of rules must be followed.
- For 3-5 days, refrain from introducing new foods into the child’s diet.
- Limit consumption of meat and meat broths.
- For 2-3 days before the test, you should not use laxatives, do an enema, or use rectal suppositories. If your baby is on a course of treatment with any medications, you should consult a doctor and discuss the possibility of temporarily discontinuing them.
Here are the rules and useful recommendations for parents on how to collect stool for analysis for dysbacteriosis.
- Defecation should occur naturally without the use of enemas, laxatives, or suppositories.
- In the morning, the toilet is performed with thorough washing of the anus.
- The baby's feces are collected from a previously laid clean diaper or oilcloth.
- The biological material is placed in a sterile container (purchased from a pharmacy).
- The amount of feces should be 10-15 g.
- The collection takes place with a special spatula attached to the cup.
After collection, stool must be delivered to the laboratory within two hours , but stool collected the night before can be stored in the refrigerator. Only fresh biological material (in no case frozen) is allowed for research.
Where can I get tested? Stool collection is carried out not only at home, but also in hospital settings. To do this, the laboratory assistant places a sterile cotton swab shallowly into the baby's anus.
Important! If parents have expressed a desire to test their child’s stool for dysbacteriosis within the walls of a medical institution, then it is necessary to find out in advance about the laboratory’s work schedule.
Where can you do a stool test for dysbacteriosis: address and price
The table below presents options for laboratories that conduct stool analysis for dysbacteriosis in various cities of Ukraine and Russia. Here you can choose the appropriate option for yourself, taking into account the cost and location of the laboratories.
| Address | Telephone | Name of hospital/clinic | Price | |
| Vinnitsa | st. Sobornaya, 46A | 958461245 | MC Oxford Medical | 160 UAH |
| Dnieper | st. Chkalova, 38 | 800509090 | Invitro | 180 UAH |
| Dnieper | Pravda Ave., 4B | 563716465 | Diagnosis | 170 UAH |
| Zhytomyr | st. Cathedral Square, 2 st. Berdicheskaya, 32 | 800606777 | Dila | 165 UAH |
| Zhytomyr | st. Chernyakhovsky, 4 | 552255 | Oxford Medical | 170 UAH |
| Zaporozhye | Metallurgov Ave., 24 | 800507030 | Sinevo | 175 UAH |
| Kyiv | st. Pavlovskaya, 26 | 994254465 | Hemotest | 180 UAH |
| Kharkiv | st. Lermontovskaya, 27 | 80050730 | Sinevo | 180 UAH |
| Kharkiv | st. Trinklera, 6 | 577191077 | Analytics | 170 UAH |
| Moscow | st. Nagatinskaya, 1, building 33. | +7 +7 (495) 363-0-363 | Invitro | 1540 rub. |
| Saint Petersburg | st. Marata, 6, Mayakovskaya metro station | — | MEDEM | 3456 rub. |
| Saint Petersburg | st. Marata, 69/71 metro station Zvenigorodskaya | — | Union Clinic | 1200 rub. |
Table for deciphering the norms of analysis for dysbacteriosis
*Literature: Intestinal dysbacteriosis in children: causes, diagnosis, treatment Educational manual / V.I. Bobrovnichiy, L.I. Vyazova. – Mn.: BSMU, 2007.
The analysis results display the entire intestinal microflora. Quantification is made in CFU (colony-forming units) in one gram of collected feces. This indicator reveals the ability of pathogenic microorganisms to multiply.
The quantity is displayed as the number 10 with many zeros or as an exponent. The standards for testing for dysbacteriosis in infants for all types of bacteria are given as a lower limit and an upper limit. An imbalance in the intestinal microflora is judged by deviations from the norm. Presence of pathogenic organisms in the intestinal cavity o, absence – “-”. Many people, when receiving research results, are faced with the concept of “proliferation”. This word means that the number of any bacteria exceeded the norm.
To whom and when is the test prescribed?
A stool test for dysbacteriosis in a child is prescribed by a pediatrician, or parents can carry out this procedure at their own request in private institutions.
Indications for the study of intestinal microflora in infants are:
- loose stools for more than 3 days;
- rash on the skin;
- unpleasant odor from the mouth;
- coating on the tongue;
- excessive salivation;
- intense regurgitation;
- underweight;
- oral candidiasis;
- lack of appetite;
- bloating, flatulence, abdominal pain;
- moodiness or lethargy;
- foamy, bloody, mucous impurities in poop;
- green or liquid stool.
A similar analysis may be prescribed for a child with severe digestive problems. If your baby refuses to eat or eating becomes restless, there is a possibility of a bacterial imbalance. The indication for the study is long-term drug treatment with antibiotics that suppress pathogenic and beneficial bacteria.
Decoding the analysis in children under one year old
All microorganisms in the analysis form are divided into:
- obligate – permanently inhabiting the body, playing an important role in metabolic processes and protection against infectious diseases;
- facultative - non-permanent residents of the body, which are either conditionally pathogenic (lead to diseases when immunity is reduced) or saprophytes (consume decaying organic substances);
- transient - free-living microorganisms that enter the body from the external environment. They can be both saprophytes and pathogens.
Let us briefly describe the main representatives of the above groups of bacteria.
Bifidobacteria
- Promote the breakdown of fats, carbohydrates, proteins that enter the bloodstream through the intestinal wall.
- Produce organic acids.
- Prevents the proliferation of pathogenic flora in the intestines.
- Promotes the absorption of nutritional elements of food.
- Optimize intestinal motility.
- Activate immunoglobulins and lymphatic elements (provide local immunity).
- Neutralizes toxins and waste.
A lack of bifidobacteria leads to flatulence, diarrhea, and frequent diarrhea.
Lactobacilli
- They convert lactose into lactic acid, which promotes better digestion of food.
- Improves digestion.
- Stimulates metabolic processes.
- They fight pathogenic microflora (especially Helicobacter Pylori strains).
- Some enzymes are activated.
- Participate in the synthesis of vitamins.
If there is a lack of lactobacilli, a child experiences frequent colds, poor digestion of milk, allergic reactions, and constipation.
Video from the Union of Pediatricians of Russia. Dysbacteriosis (dysbiosis).
Bacteroides
They occupy approximately half of the entire intestinal microflora. When maintaining a normal amount, bacteroids perform a number of useful functions - they participate in the utilization of proteins, the breakdown of fats, the fermentation of carbohydrates, and the biotransformation of bile acids. If the levels are exceeded, bacteroids lead to infectious and septic complications and contribute to the destruction of beneficial E. coli (in the fight for oxygen).
Eubacteria
They are more common in formula-fed children and are practically absent in children fed breast milk. Most typical for adults. Their role is not clear enough, but it is known that they are involved in some metabolic processes.
Fusobacteria
More often observed in the intestinal microflora of adults. Some species are sown during purulent-inflammatory processes. Little studied.
Opportunistic bacteria and fungi do not cause intestinal problems in a healthy child until the immune system is weakened or the condition of the intestinal mucosa is disrupted. An increase in the level of opportunistic organisms is also observed against the background of a decrease in indicators of lactobacilli and bifidobacteria. At the same time, the baby experiences flatulence, diarrhea, inflammation of the intestinal mucosa, and increased fermentation processes.
Escherichia (opportunistic Escherichia coli)
- Suppress the growth of pathogenic microorganisms, in particular Shigella, Salmonella and putrefactive microbes.
- Promote the synthesis of folic and nicotinic acid, vitamins K and B.
- Provide local immunity.
- They take part in the breakdown of high molecular weight carbohydrates using enzymes.
- Participate in water-salt and lipid metabolism.
- Helps improve intestinal motility.
If the number of these bacteria is reduced, this indicates the presence of a helminthic infection. Typically, this disorder manifests itself in the form of vomiting, flatulence, rumbling in the stomach, and diarrhea. In addition to the number of Escherichia, the level of Escherichia coli with reduced enzymatic activity is determined.
Veillonella
Found in less than half of examined infants. In the process of vital activity, gaseous products are released and, when excessively multiplied in the intestines, cause dyspeptic disorders.
Peptostreptococci
Just like veillonella, they are rarely found in breastfed children. If they find themselves in unusual living conditions, they can cause various infections. In deep abscesses, they often occupy the second place among anaerobic bacteria in terms of occurrence in pathological material.
Clostridia
Participate in the metabolism of fatty acids and suppression of the activity of pathogenic species of clostridia. Some species, when breaking down proteins, can form toxic products. Decreased immunity and excess meat food can lead to the growth of these bacteria.
Enterococci
Enterococci are the most common representatives of streptococci in the intestines. In the intestinal lumen they are able to ferment carbohydrates into lactic acid, thereby maintaining optimal acidity for the proliferation of beneficial microflora.
Staphylococcus
A large group of microorganisms that enter the intestines from the first days of a child’s life. The most numerous of them is Staphylococcus epidermidis. Increased activity of Staphylococcus aureus causes the appearance of infectious diseases.
Interpretation of test results
| Children under 1 year | Older children | Adults | |
| Bifidobacteria | 1010 – 1011 | 109 – 1010 | 108 – 1010 |
| Lactobacilli | 106 – 107 | 107 – 108 | 106 – 108 |
| Escherichia | 106 – 107 | 107 – 108 | 106 – 108 |
| Bacteroides | 107 – 108 | 107 – 108 | 107 – 108 |
| Peptostreptococci | 103 – 105 | 105 – 106 | 105 – 106 |
| Enterococci | 105 – 107 | 105 – 108 | 105 – 108 |
| Saprophytic staphylococci | ≤104 | ≤104 | ≤104 |
| Clostridia | ≤103 | ≤105 | ≤105 |
| Candida | ≤103 | ≤104 | ≤104 |
| Pathogenic staphylococci | — | — | — |
| Pathogenic enterobacteria | — | — | — |
Other indicators in the photo:
- Bifidobacteria are the main representatives of the intestinal microflora. They protect our body from harmful microorganisms. If their number is significantly less than normal, this is a sign of dysbiosis.
- Lactobacilli are microorganisms that break down lactose for subsequent digestion. They are also necessary to maintain optimal levels of intestinal acidity.
- Escherichia coli are Escherichia coli that take oxygen from the large and small intestines, which can destroy beneficial bacteria for humans, and also contribute to the production of vitamins B and K.
- Bacteroides are rods that promote the digestion of proteins, fats and carbohydrates. Peptostreptococci release hydrogen into the intestinal cavity, which is necessary to maintain optimal acidity.
- Enterococci help maintain acidity at an optimal level and stimulate fermentation processes in the intestines.
- Saprophytic staphylococci produce pathogenic enzymes.
- Clostridia contribute to adequate digestion of intestinal contents.
- Candida is one of the intestinal microorganisms that does not have a significant effect on the process of food digestion, but with increased reproduction contributes to the development of candidiasis.
- Pathogenic staphylococci and enterobacteria are not normally found in feces.
Degrees of dysbacteriosis
**Literature: Dysbiotic intestinal disorders in children, principles of correction. Fayzullina R. A., Pikuza O. I., Zakirova A. M., Shoshina N. K. – Methodological manual. – Kazan, KSMU, 2015.
Dysbacteriosis occurs in 90% of infants. Most often, an imbalance of intestinal microflora is diagnosed in babies who are bottle-fed, born prematurely and with low weight. Dysbacteriosis is treated with the help of probiotic preparations - Linex, Bifidumbacterin, etc. These drugs stimulate the reproduction of beneficial microflora. Often, when dysbiosis is detected, a doctor advises sticking to a diet and switching to a different mixture.
What is dysbiosis?
Dysbacteriosis is usually understood as a violation of the ratio of various bacteria found in the human body and contributing to the maintenance of immune, metabolic and biochemical processes. Quantitative and qualitative disorders of the intestinal microflora are extremely common phenomena.
According to statistics, up to 95% of the population faces this problem. Moreover, both adults and children are susceptible to dysbacteriosis. There are many reasons that cause disruption of the biological balance of microflora. These include poor nutrition, lack of vitamins, and treatment with certain medications.
Although modern medicine does not recognize dysbiosis as a disease, this condition is pathological, destructive and poses a threat to human health. The most common consequences of dysbiosis are considered to be disturbances in the functioning of the immune system, metabolism, diseases of the gastrointestinal tract, disruptions in the digestive system, and so on.
Dysbacteriosis often develops against the background of severe fungal infections of the intestines, blood diseases, and diseases of the bronchopulmonary system of a chronic nature.