What is the connection between the pancreas and diabetes?
The pancreas is an organ that produces insulin and plays an important role in regulating blood glucose levels.
There is a clear connection between the pancreas and diabetes. Type 1 diabetes occurs when the pancreas does not produce enough insulin. Type 2 diabetes develops when the body cannot use insulin properly.
In this article we will look at the connection between the pancreas and diabetes. We will also describe complications of diabetes related to the pancreas and other organ disorders.
Diagnostics
Diagnosis includes determining the form of diabetes, its severity and the presence of possible complications. If diabetes is suspected, the following types of inheritance are prescribed:
- Fasting blood glucose. Normally it is 3.3 – 5.5 mmol/l. An increase in this indicator above 11 mmol/l in the absence of errors in the diet allows a diagnosis of diabetes to be made without further examination.
- Blood sugar with load. Blood is drawn on an empty stomach and 2 hours after ingestion of a glucose solution. Normally it is 7.8 mol/l. Anything above is regarded as a prediabetic condition or impaired glucose tolerance.
- Sugar in urine. Normally it shouldn't be there. Glucose in urine is determined only when the renal barrier is exceeded (over 6 millimoles per liter).
- Glycosylated hemoglobin. Determines whether there has been an increase in sugar over the past 3 months. Blood for this test is taken only from a vein.
Ultrasound is one of the methods for diagnosing the pancreas
To diagnose possible complications of diabetes, additional research methods are performed: fundus examination, ultrasound of internal organs, electrocardiogram.
Biochemistry and general clinical tests are also taken.
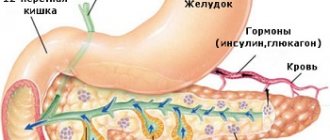
What you need to know about the pancreas
The pancreas is located in the abdomen, behind the stomach, and it produces digestive enzymes.
It also produces insulin, a hormone that regulates blood sugar. The cells that produce insulin are called beta cells. They are located in the islets of Langerhans, located in the body of the pancreas.
Insulin helps the body use carbohydrates in food for energy. It transports glucose from the blood to the body's cells. Glucose provides cells with the energy they need to function.
If there is too little insulin in the body, cells can no longer absorb glucose from the blood. As a result, the level of glucose in the blood increases.
How to replace sugar for pancreatitis
Many confectionery manufacturers produce glucose-free products based on various sweeteners. The following additives are most often used as sweeteners: sorbitol, xylitol, saccharin.
Sugar substitutes can also be used to make sweets at home.
However, before including these products in food, the patient should discuss the advisability of their use with the attending physician, so as not to provoke the development of complications associated with the functioning of the pancreas.
Fructose
Fructose is a fairly popular sweetener, the processing of which does not require insulin, so it can be consumed by patients with pancreatitis. The product is absorbed gradually, as a result of which the glucose level rises slowly and does not exceed the permissible limit. You are allowed to consume no more than 60 g of fructose per day. This will protect against the development of flatulence, diarrhea and lipid metabolism disorders.
We recommend reading: Can you eat cauliflower for pancreatitis?
Honey
Honey not only treats colds, but is also a natural sugar substitute. It contains a lot of useful substances and microelements that help digestion and have a beneficial effect on the diseased pancreas. However, in the acute stage of the disease, honey, as well as sugar-containing products, is removed from the patient’s menu. It is allowed to introduce it into the diet no earlier than a month after an exacerbation.
What exactly is the connection between the pancreas and diabetes?
Type 1 and 2 diabetes are related to the pancreas.
Diabetes is characterized by high blood sugar levels. This is a consequence of insufficient insulin production or function, which can be one of the consequences of problems with the pancreas.
People with diabetes have varying blood sugar levels depending on what they eat, how much they exercise, and whether they take insulin or diabetes medications.
Type 1 diabetes
Type 1 diabetes occurs when the pancreas does not produce enough or any insulin. Without insulin, cells cannot get enough energy from food.
This form of diabetes occurs as a result of the immune system attacking the insulin-producing beta cells of the pancreas. Beta cells become damaged, and over time the pancreas no longer produces enough insulin to meet the body's needs.
People with type 1 diabetes can balance their blood glucose levels by injecting themselves with insulin each day or by getting an insulin pump.
Doctors once called this type of diabetes "juvenile diabetes" because it most often develops during childhood or adolescence.
The main cause of type 1 diabetes has not yet been identified. Some evidence suggests that this diabetes is a consequence of genetic or environmental factors. In the United States, an estimated 1.25 million people live with type 1 diabetes.
Type 2 diabetes
This type of diabetes occurs when the body creates insulin resistance. Although the pancreas can still produce the hormone insulin, the body's cells can no longer use it effectively.
As a result, the pancreas produces more insulin to meet the body's needs, and is often no longer able to meet the increased demand.
When there is not enough insulin in the body, diabetes develops. Over time, beta cells become damaged and may stop producing insulin altogether.
Like type 1 diabetes, type 2 can cause blood sugar levels to rise and prevent cells from getting enough energy.
Type 2 diabetes can be the result of poor genetics and family history. Lifestyle factors such as obesity, lack of exercise and poor diet also play a role. Treatment often includes increasing your level of physical activity, changing your diet, and taking certain prescription medications.
A doctor can detect type 2 diabetes in an early stage called prediabetes. A person with prediabetes may be able to prevent or delay the onset of the underlying disease by making immediate changes to their diet and lifestyle.
Diabetes mellitus during pregnancy
Pregnancy can cause type 2 diabetes, known as gestational diabetes. This type of diabetes can cause complications during pregnancy and childbirth.
Gestational diabetes usually goes away after birth, but there is evidence that it increases the risk of developing type 2 diabetes later in life.
Fruits and vegetables
First of all, you need to pay attention to them. They are not only incredibly useful for humans, but are also enriched with numerous vitamins that are so necessary for full life.
You should try to consume plenty of vegetables and fruits every day. Only then will you be able to make up for the lack of vitamins and gradually improve your health. Fruits and vegetables are natural food for the human being, which is why they are so well absorbed by the body.
Anyone who eats right lives longer, without any problems with the nervous, cardiovascular and digestive systems.
Diabetes and pancreatitis
Pancreatitis causes inflammation in the pancreas.
There are two types of pancreatitis:
- acute pancreatitis, in which symptoms appear suddenly and last several days
- chronic pancreatitis, a long-term condition in which symptoms come and go over several years
Chronic pancreatitis can damage pancreatic cells, which can eventually cause diabetes.
Pancreatitis is treatable, but severe cases may require hospitalization. Anyone should take pancreatitis seriously as it can be life-threatening.
Frequent symptoms of pancreatitis:
- vomit
- pain in the upper abdomen that may radiate toward the back
- pain that gets worse after eating
- fever
- nausea
- jumping pulse
Additional tests
If the doctor suspects that a patient has developed pancreatitis, then, in addition to the CBC and biochemical examination, he may prescribe other blood tests. Among them is a laboratory blood test for immunoreactive trypsin. This analysis is very informative, as it allows you to obtain data not only on the condition of the pancreas, but also other organs, which makes it possible to promptly identify the patient’s complications due to pancreatitis, for example, hypercortisolism, renal failure, etc.
Venous blood is taken to study immunoreactive trypsin.
It should immediately be noted that the main indicator of the development of pancreatitis is a decrease in the level of trypsin in the blood. And the lower it is, the less favorable the prognosis. However, this analysis is carried out very rarely in medical practice, since it is paid and costs a lot of money.
It should also be said that when diagnosing pancreatitis, a urine test is often prescribed. But not the general one, but the one that allows you to identify the level of trypsinogen in the material under study. This enzyme is an inactive form of trypsin and it appears in the urine only when there are inflammatory processes in the pancreas.
The development of pancreatitis negatively affects the functioning of the entire digestive tract. Therefore, when it occurs, almost 9 out of 10 patients experience bowel problems. It is for this reason that a stool test is mandatory in diagnosing this disease. When studying it, special attention is paid to:
- the presence of fat in the stool (during normal functioning of the digestive system it should not be present),
- the color of the material being examined,
- the presence of undigested food elements in the stool.
In the presence of any deviations from the norm, we can talk about the presence of various disorders of the digestive tract. Moreover, to determine them it is not at all necessary to conduct a laboratory study. The patient himself can identify such disorders if he carefully examines the stool. Its discoloration indicates blockage of the bile ducts. At the same time, the feces themselves are poorly washed off the walls of the toilet, which also indicates the presence of inflammatory processes in the body. Due to the high fat content, stool becomes shiny and emits an unpleasant, pungent odor.
As mentioned above, laboratory tests of blood, urine and feces alone are not enough to make a diagnosis. To verify the development of pancreatitis in a person, it is imperative to conduct an ultrasound examination of the pancreas, as well as fibroesophagogastroduodenoscopy, which will reveal abnormalities at the junction of the main pancreatic duct into the duodenum. As a rule, instrumental diagnostics are carried out in a hospital setting and allow a full assessment of the condition of the body and pancreas.
Diabetes and pancreatic cancer
According to the Pancreatic Cancer Society, people who live with diabetes for 5 years or more are 1.5 to 2 times more likely to develop pancreatic cancer.
The onset of type 2 diabetes later in life may be a symptom of this type of cancer.
The direct link between diabetes and pancreatic cancer is still poorly established. Diabetes is known to increase the risk of developing this type of cancer, and pancreatic cancer can sometimes lead to diabetes.
Other risk factors for pancreatic cancer:
- obesity
- aging
- poor nutrition
- smoking
- genetic inheritance
In the early stages, this type of cancer may not cause any symptoms. Doctors most often diagnose it in the later stages, when the patient is usually no longer operable. Therefore, it is necessary to undergo an annual examination of the gastrointestinal tract.
Reviews
Dear readers, your opinion is very important to us - therefore, we will be glad to hear your feedback about sugar for pancreatitis in the comments, this will also be useful to other users of the site.
Tatiana:
During an exacerbation, you don’t want to eat anything at all. I live for a week on fermented milk products and medicinal teas. You start craving sweets after about 2 weeks.
Marina:
During remission I don’t deny myself sweets, but everything is normal. By the way, I stopped liking sweets when digestive problems appeared. I practically don’t eat any kind of cakes, pastries or sweets. Sometimes ice cream, cookies, buns with jam, chocolate.
Other diseases of the pancreas
Cystic fibrosis can also lead to the development of insulin-dependent diabetes (type 1).
In a person with cystic fibrosis, persistent sticky mucus causes scar tissue to form on the pancreas, and scarring can prevent the organ from producing enough insulin. As a result, cystic fibrosis-related diabetes (CFRD) may develop.
The signs and symptoms of CFRD may resemble those of cystic fibrosis. A person may not know that he does not have cystic fibrosis, but diabetes, until he passes the appropriate tests.
Fructose instead of sugar
It is a simple carbohydrate that the body needs to replenish energy. The calorie content of fructose and sugar is almost the same, but the first product is several times sweeter. That is, to drink a cup of sweet tea, you need to add 2 teaspoons of sugar or 1 fructose. Fructose is absorbed more slowly, so it does not provoke a sharp release of insulin. Satisfaction with sweets does not come immediately, but the feeling of fullness lasts a long time. The sweetener is recommended for use in pancreatitis, obesity, and diabetes. The main rule is good in moderation.
You also need to take into account the fact that only natural fructose is useful; it is better to replenish the body with this component by eating berries, fruits, honey, and dried fruits. The popular corn sweetener, also called fructose, leads to obesity, heart disease, vascular disease, and digestive problems. Excessive consumption of fructose leads to the development of hypertension, gout, fatty liver disease, accumulation of “bad” cholesterol, type 2 diabetes, and oncology.
How sugar affects memory
5. You will remember information better
© Auero
You will notice your memory improve dramatically after you eliminate sugar from your diet.
Consuming too much sugar can lead to forgetfulness and even memory loss.
If you continue to consume sugar uncontrollably, you can develop serious brain diseases, experts say.
In their opinion, it is sugar that is responsible for the deterioration of our memory. This is evidenced by research by scientists at the University of California.
In addition, its uncontrolled use affects your learning ability and ability to perceive information. These skills will gradually deteriorate if you do not stop and start consuming minimal amounts of sugar.
© SergeyBaykov/Getty Images
Its effect on the brain in general is quite negative. Sugar has been proven to interfere with the functionality of cells in the human body.
One scientific study describes an experiment that showed that our cognitive abilities are influenced by the foods we eat.
Products containing sugar and high fructose content have a negative impact on health.
Metabolic syndrome or MetS is a known link between consuming too much sugar and brain damage and is a risk factor for obesity.
However, the connection to mental health tends to be largely ignored. Since on average some people are known to consume 2-3 times more sugar than doctors allow each day, it can be assumed that the long-term effects of this product on brain function are very harmful.