To make a correct diagnosis of gastrointestinal lesions and prescribe effective treatment, certain studies are necessary. One of them is gastric probing. It is important to know under what circumstances the procedure is needed, how it is performed and when it is contraindicated.
Probing of the stomach is a very important diagnostic procedure
Indications for probing
In gastroenterology, gastric probing and lavage are very important procedures, without which it is impossible to determine what disease a person is facing. Let's consider under what circumstances a study is ordered:
- To determine what disease has affected a person and prescribe effective treatment therapy.
- If you need to feed the patient or administer a medication directly into the stomach. This is necessary for premature babies, if the patient has pathologies or injuries that are associated with the esophagus, pharynx, oral cavity, as well as people in a coma.
- When you need to rinse your stomach during intoxication caused by chemicals or poor quality food.
Probing may be required in case of drug overdose and intoxication
Gastric and duodenal intubation allows the doctor to determine the characteristics of the development of the disease, whether the gastric tissue has changed, and also check for the presence of tumors.
In case of poisoning, using a special type of probe, it is possible to quickly remove toxic substances from the body, so that they do not disrupt the functioning of vital internal organs.
What is sounding and who is it prescribed for?
The contents of the stomach and duodenum are aspirated using a probe and then examined in the laboratory, where the pH of gastric juice is determined by titration method. Determining the acidity of gastric juice is important when prescribing drug therapy. The study is carried out fractionally, first on an empty stomach, then after 15 minutes and after stimulation.
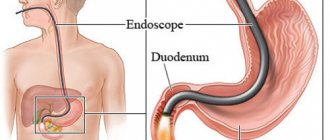
The procedure involves inserting a tube through the patient's mouth or nose, which is then advanced into the stomach. This examination does not cause discomfort, although it is performed without anesthesia.
Modern medicine has made it possible to use a very thin probe with a diameter of 0.5 cm for this procedure. That is why probing does not bring any unpleasant sensations. In addition, now one end of the probe is equipped with a small video camera, which displays a picture on the monitor screen about the condition of the stomach and its structure.
Content:
- What is sounding and who is it prescribed for?
- Preparation for the procedure
- How is probing carried out?
- Interpretation of survey results
- Contraindications to undergoing the examination
- Recovery after the procedure
- Summing up
This diagnostic method allows the doctor to more accurately diagnose the patient, detect and prevent the development of various diseases.
With the help of gastric probing, diseases such as stomach ulcers, reflux esophagitis and gastritis with low or high acidity can be detected in the early stages.
In addition, this procedure is used for other purposes. Often, a probe is used to introduce medications or food directly into the stomach of a patient who cannot do this themselves: premature babies, patients with injuries to the esophagus, face, oral cavity or pathologies of the larynx, unconscious patients.
Probing is also often used in medical practice for aspiration of poisons and toxins from the stomach in case of toxic damage. A special type of probe is used for this.
This type of diagnosis also makes it possible to identify malignant neoplasms in the early stages and prevent their development, signal any changes occurring in the gastric tissues, and also learn about the structural features of the mucous membrane.
Types of sensing
In medicine, there are two main methods of gastric intubation. Simultaneous probing of the stomach through the mouth is carried out with a thick gastric tube. This device looks like a rubber tube, about 100 cm long, and its diameter is up to 13 mm. The study got its name from the one-time pumping of stomach contents. This method has long been outdated and is practically not used due to the fact that it does not give a complete picture of the state of the organ. Due to the large size of the device, the patient feels uncomfortable and gags.
A special device is used for probing
Fractional research is carried out with a thin device in the form of a tourniquet, 100–150 cm long, its diameter is only 2 mm, the end of the tube is rounded, there are two holes and marks on it. The other edge of the device is equipped with a syringe, which is used to pump out gastric contents. There is no gagging during the procedure, so the doctor has the opportunity to conduct the study for an unlimited amount of time. Probing by the fractional method is carried out in 3 stages:
- Empty gastric juice. Once the tube is inserted, the contents of the stomach are removed.
- Basal gastric juice. The secretion is sucked out for 1 hour.
- Stimulated gastric juice after administration of a stimulant. The duration of secretion is about 2 more hours with suction of the stomach contents at intervals of 15 minutes.
The examination does not cause discomfort and can last quite a long time.
Technique for fractional intubation of the stomach.
Functional purpose of the PMU: diagnostic - for the study and assessment of the secretory function of the stomach.
Indication: as prescribed by a doctor.
Material resources: Devices, instruments, medical products - a sterile tray with a thin gastric tube (1.5 m long, 4 mm in diameter), napkins, a clamp, a 2.0 ml syringe, a tray for collecting saliva, a Janet syringe
Medicine - parenteral irritant - pentagastrin, containers with disinfectant. solution, skin antiseptic
Other consumables – respirator, napkin, rack with 9-10 test tubes (numbered), direction, glass of boiled water, gloves, towel
Characteristics of the methodology for performing a simple medical service:
preparation for the procedure
:
— identify the patient (the patient’s full name must match the full name on the referral);
— inform the patient about the doctor’s prescription, explain the process and purpose of the procedure;
- obtain consent, inform that the procedure is carried out in the morning on an empty stomach, the evening before he should not eat rough and spicy food;
— the patient must bring a towel with him;
— invite the patient to the probing room;
- the nurse washes his hands at a hygienic level, treats them with an antiseptic,
performing the procedure:
- seat the patient at the table opposite you;
— place a towel on the patient’s chest and give a tray to collect saliva in his hands;
- puts on gloves and a respirator;
- take the probe and measure the distance to which you will insert it (see how you do when washing the stomach);
— carry out the technique of inserting a probe into the stomach (see gastric lavage);
- after inserting the probe into the stomach, attach a Janet syringe to the opposite end of the probe and collect, sucking out the contents of the stomach, into test tube No. 1, this is an fasting portion;
—
for an hour, every 15 minutes, collect gastric contents by suction and pour into test tubes, these are portions - 2nd, 3rd, 4th, 5th;
- after collecting five portions, inject pentagastrin subcutaneously, apply a clamp to the opposite end of the probe for 15 minutes;
- after the time has elapsed, every 15 minutes for an hour, use a Janet syringe to collect the contents of the stomach - this is the 6th, 7th, 8th, 9th portion;
completion of the procedure
:
— after the procedure, carefully remove the probe using a napkin and place it in the waste material tray;
- give the patient boiled water to rinse the mouth;
— ask about the patient’s well-being, show him to the room;
— take the rack with test tubes and directions to the clinical laboratory;
— disinfect the probe and trays in a 3% chloramine solution for an hour (all separately);
- remove gloves, a respirator and disinfect them in a 3% chloramine solution for an hour, wash your hands;
— make a note about the manipulation on the patient observation sheet.
Achieved results and their evaluation
The main assessment of the procedure performed will be to obtain the full scope of analysis required for research.
A simple medical service is performed with minimal discomfort for the patient
Parameters for assessing and quality control of the method implementation
— Availability of a record of the results of the prescription in the medical documentation
— Timely execution of the procedure (in accordance with the doctor’s prescription)
— No post-injection complications
— Patient satisfaction with the quality of the medical service provided.
— Samples were delivered to the laboratory in a timely manner
— There are no deviations from the execution algorithm.
Technique for duodenal intubation.
Functional purpose of the PMU: diagnostic - obtaining duodenal contents for research.
Indication : as prescribed by a doctor (liver and gallbladder disease).
Contraindications: acute cholecystitis, narrowing of the esophagus, angina pectoris, myocardial infarction, gastric bleeding.
Material resources: Devices, instruments, medical products, sterile tray with duodenal probe (1.5 m long with a diameter of 4-5 mm at the end - olive), Janet syringe, clamp,
The medicine is a 33% solution of magnesium sulfate at a temperature of 40 C in an amount of 50 ml, containers with disinfectant. solution, skin antiseptic
Other consumables - a heating pad with warm water, a stand with test tubes, a jar for collecting gastric contents, gloves, a towel, a bench, a glass of boiled water, a respirator.
Patient preparation:
2-3 days before the test, exclude from food foods that cause flatulence (sauerkraut, potatoes, dairy products, white bread, vegetables, apples). During these days, food should be rich in carbohydrates - drink tea with honey or sugar. In the evening I should eat 2 tbsp. l. honey or drink an ampoule of 40% glucose, put a warm heating pad under the right hypochondrium, drink soothing tinctures (tincture of valerian, peony) at night. The study is carried out in the morning on an empty stomach.
Characteristics of the methodology for performing a simple medical service:
preparation for the procedure:
— identify the patient (the patient’s full name must match the full name on the referral);
- inform the patient about the procedure, explain the process and purpose of the procedure;
— get consent, explain how to prepare;
- invite him to the room for sounding;
- sit on the couch, put a towel on your chest;
- wash your hands at a hygienic level, treat them with an antiseptic;
performing the procedure:
- wear gloves and a respirator
- take the probe and measure the distance to which you will insert (from the earlobe to the tip of the nose + from the incisors of the teeth to the navel and the width of the palm), put a mark, moisten the olive in water;
- stand to the right of the patient, ask the patient to open his mouth, place the olive on the root of the tongue and ask the patient to close his mouth and make swallowing movements;
- as you swallow, you move the probe to the mark;
- after this, fix the probe with a bandage to the patient’s head, give him a jar to collect gastric contents and ask him to walk quickly around the room for 15 minutes;
— after 15 minutes, place the patient on the couch on his right side with his legs bent, place a warm heating pad under the right hypochondrium, a cushion under the patient’s pelvis, and apply a clamp to the probe;
— place a bench next to it, on which there is a stand with test tubes (the bench should be lower than the couch);
- when the olive enters the duodenum, a yellow liquid begins to flow, remove the clamp and lower the probe into the test tube, this is portion “ A ”
is a mixture containing bile, pancreatic secretion, intestinal juice. In 20-30 minutes, 15-40 ml are delivered;
- after collecting portion “ A ”, lay the patient on his back, and using a Janet syringe, inject 50 ml of magnesium sulfate solution (to stimulate the gallbladder) and apply a clamp to the probe for 10 minutes;
- after 10 minutes, put the patient in the same position, remove the clamp, lower the probe into a clean test tube, and immediately a dark olive liquid begins to flow - this is portion “ B ”,
30-60 ml is collected. When there is stagnation in the gallbladder, dark green bile is released;
- after the release of portion “B”, a bright yellow liquid immediately enters portion “ C”
“This is liver bile, 15-20 ml are secreted;
end of the procedure:
- after receiving three servings, seat the patient on the couch;
— carefully remove the probe using a napkin and place it in the waste material tray;
— let the patient rinse his mouth with boiled water;
— ask about your health, show you to the room;
— deliver the rack with test tubes and directions warm to the clinical laboratory;
— disinfect the probe, tray, napkin in a 3% chloramine solution for an hour (all separately);
- remove gloves, a respirator and disinfect them for an hour in a 3% chloramine solution, wash your hands;
— make a note about the manipulation on the patient observation sheet.
Achieved results and their evaluation
The main assessment of the procedure performed will be to obtain the full volume of portions required for research.
A simple medical service is performed with minimal discomfort for the patient
What is needed for research
Gastric lavage and probing are very important procedures that take a long time. To perform the procedure, doctors use:
- a stool for positioning the patient;
- a special container in the form of a basin;
- a thin sterile probe;
- a syringe or pump that fits onto the hose;
- towel;
- several labeled sterile test jars.
All of the above items must be prepared before the procedure begins, as they should always be on hand by the specialist conducting the study.
Each endoscope has a syringe or pump to control the manipulation of the device
Indications
Fractional (multi-stage) gastric intubation is prescribed for the following conditions:
- Stomach ulcer;
- Diseases of the biliary tract, liver;
- Anemia (anemia);
- Stomach disorders (achlorhydria, “irritable” stomach);
- Cancerous neoplasm;
- Diseases in which the stomach is involved in the process;
- Gastritis.
Preparation for gastric intubation
Preparing the patient for gastric intubation plays a very important role, since without this process the results of the study may be false. These measures do not require any special effort; they are aimed at ensuring that the stomach is completely emptied before the procedure for a clear and clear picture of the examination through the probe:
- during the day before the study you should refrain from smoking and taking medications;
- do not eat foods that increase the secretion of gastric juice and the accumulation of gases;
- 14–16 hours before the procedure begins, do not eat anything, you are only allowed to drink clean water in unlimited quantities;
You should not drink soda before the procedure.
- improve your psychological state, do not be exposed to stress, otherwise the secretion of gastric juice will increase and the results of the study will be incorrect, which will prevent the disease from being correctly diagnosed;
- Immediately before the examination begins, the inserted dental structures should be removed.
Preparation for the procedure
The most important thing before carrying out such a procedure is to calm down and put your nervous system in order. Excessive anxiety and nervousness will only negatively affect gastric juice and cause an unwanted gag reflex.
Before diagnosis, it is recommended to talk with your doctor about exactly how the examination will take place, tune in to a positive effect and stop worrying.
In addition, before probing, it is necessary to refrain from eating any food and smoking for twelve hours, so as not to disturb the composition of the gastric juice. You can still drink water.
If the patient is taking any medications, he must notify the doctor who will conduct the examination. Before this procedure, it is not recommended to use antacids, caffeine, atropine and other medications that affect the functioning of the stomach.
Next, the patient is prepared for the procedure directly in the doctor’s office. To do this, he lies down on his left side and covers his chest with a napkin so as not to stain his clothes with saliva. Saliva is spit out during diagnosis; it is not allowed to swallow it.
A special ring is inserted into the patient’s mouth, which will prevent him from closing his jaw and accidentally damaging the probe. The oral cavity is treated with an anesthetic aerosol to reduce sensitivity.
The probe is inserted directly behind the root of the tongue, and then the patient, using swallowing movements, pushes it deep into the stomach. Afterwards it is fixed on the patient’s clothes so that it does not slip deeper.
The free end of the probe is connected to a special pump, which will be used to aspirate the contents of the stomach.
How is the procedure performed?
The methods of duodenal and gastric intubation are very similar, so let’s look at how the study is carried out:
- the patient sits on a chair with a back, or sits on a couch, lying on his side;
- to avoid staining clothes with saliva or vomit, cover your shoulders and chest with a towel;
- a person is given a special container to spit saliva into;
Before probing, the throat is treated with an analgesic
- to reduce sensitivity and also eliminate pain, the pharynx is treated with a local analgesic;
- the edge of the probe is placed on the tongue as deeply as possible (there may be holes or a camera on it, depending on the purpose of the procedure), then the patient swallows, and the doctor carefully pushes the tube inside;
- the rhythm of nasal breathing is checked, it should be calm;
- With each swallowing movement, the device is pushed deeper and deeper until it reaches the desired mark. The required depth is determined according to the following scheme: 100 cm is subtracted from the person’s height. After that, the probe is attached to the patient’s clothing for fixation;
The patient is given a small tube to swallow
- then a pump or syringe is put on the opposite edge of the device and all its contents are pumped out of the stomach;
- the basal gastric secretion is sucked out in several stages, the duration of which is no more than 5 minutes, with breaks between them of 10 minutes;
- Next, the patient is given a so-called “test breakfast” in the form of a light broth or special enzymes that stimulate the productivity of gastric juice (thanks to this, the doctor determines how the stomach functions when food enters it);
- then over the course of an hour, samples of gastric juice are taken 7 times every 10 - 15 minutes;
- when gastric intubation has come to an end, the device is removed.
The doctor then takes samples of gastric juice
Detailed description of the research technique
The probing technique consists of stages:
- The end of the probe, which may be equipped with a small chamber or holes, is placed on the tongue. The purpose of the study determines the choice of equipment type. The patient then swallows to move the probe inside. The tube moves further until the desired level is reached. The level is calculated as follows: 100 cm is subtracted from the patient’s height or 55 cm is added from the edge of the teeth. This allows you to calculate the level of tube insertion individually.
- The probe can be inserted through the nasal cavity. The tube is lubricated with Vaseline and carefully inserted 10 cm into the nose. Then the subject is asked to swallow. Next, the desired depth of tube insertion is achieved.
- For fixation, the tube is attached to the patient's clothing.
- Using a vacuum suction or syringe, the contents of the stomach are aspirated. The part of the secretion taken away is called the “fasting” portion.
- Obtaining part of the contents “on an empty stomach” or basal secretion is carried out in several stages. The duration of each stage is five minutes, the break between stages is ten minutes.
- Later, the production of gastric secretions is stimulated using a parenteral stimulus. This type of stimulants includes: histamine, insulin, pentagastrin. The stimulant is selected to be strong and fast-acting. Also, the secretory effect is achieved by administering drugs enterally. Then, using a tube, special stimulating drugs or products are introduced into the stomach, assessing the functioning of the stomach after eating.
- Fifteen minutes later, the next gastric contents are collected.
- The sampling is carried out seven times over the course of an hour.
- The tube is removed and the patient is allowed to rest.
Evaluation of results
After gastric intubation has come to an end, test tubes filled with tests that have been previously signed are handed over to the laboratory for testing. To determine the correct diagnosis, the color, volume and nature of the secretion obtained is taken into account:
- It is considered normal if the secretion has a transparent appearance and moderate ductility.
The resulting secretion is sent to the laboratory for analysis.
- If the amount of secretion is greater than the norm and with the presence of undigested food residues, then this indicates that the person secretes gastric juice at an increased level with clearly impaired acidity.
Other laboratory tests are needed to determine the exact acidity level.
- When the secretion is not transparent, but has some shade, this means that the patient has health problems. A green or yellow tint indicates the presence of bile in the stomach, which comes there from the duodenum. Red and brown tints indicate that blood is present in the organ.
- If the gastric juice is too viscous, then the person is faced with gastritis or peptic ulcer.
If the mucus is thick, the patient most likely has gastritis
Interpretation of survey results
This procedure is aimed mainly at studying the secretory function of the stomach. It can be used to diagnose most diseases of the digestive system:
- a clear, non-viscous liquid with normal acidity indicates a completely healthy stomach;
- the predominance of yellow or green in the liquid indicates an admixture of bile, red and brown - an admixture of blood;
- food residues in the pumped out fluid and an increased total volume make it possible to judge hypersecretion of gastric juice;
- increased fluid viscosity indicates the presence of gastritis;
- depending on the content of hydrochloric acid, treatment is directed either to limit its production, or, conversely, to stimulate it;
- the acidity of the stomach is established: low or high.
Recommendations after the procedure
Gastric intubation causes almost no side effects in anyone. During the day you may feel slightly unwell and have an upset stomach. There is no need to treat such phenomena; the condition will improve on its own. To avoid stress on the stomach, it is recommended not to eat too much during the day after the examination. It is best to have lunch with crackers and sweet tea; in the evening, when the condition returns to normal, you are allowed to have a full dinner.
There is no need to be afraid of gastric probing and put it off. Thanks to the latest technologies, the procedure is now much more comfortable and painless compared to what it was before. The main thing is to realize that probing allows the doctor to determine the correct diagnosis and prescribe competent therapeutic therapy, thanks to which health will be restored or even a life will be saved.
How is gastric intubation performed? They will tell you about this in the video: