What is pyloric stenosis?
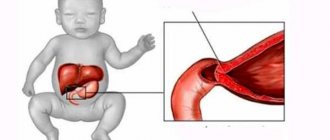
This is an anomaly in the development of the gastrointestinal tract, in which there is a narrowing of the pyloric part of the stomach (the place of transition to the duodenum, the pylorus).
Even before the baby is born, the circular muscles in the wall of his stomach greatly increase and become overgrown with connective tissue. The pylorus becomes olive-shaped, resembles cartilage in density and can no longer contract.
Interesting fact: the pathology occurs in every 2-3 children per 1000 newborns. Moreover, there are 5-7 times more boys than girls.
Diagnostic methods
To diagnose pyloric stenosis in infants and newborns, various methods are used in medical practice.
Ultrasound of the pyloric stomach in a newborn
Ultrasound of the pyloric stomach in newborns is performed by a surgeon, pediatrician or other pediatrician who has the appropriate license and qualifications.
Important! It is advisable to refrain from feeding your baby 3 hours before the procedure.
Ultrasound is performed on babies in an upright or lying position. The specialist applies sensors to the body, thanks to which the condition of the esophagus, stomach, lymph nodes and endocrine glands can be seen on the monitor.
Diagnostics
Additional Information. Based on the results of the ultrasound examination, a detailed protocol is drawn up with a transcript of the data obtained and a medical report.
The specialist does not give the little patient a final diagnosis and does not prescribe how to treat the disease. Its task is to identify the stage of development of the pathology and the characteristics of the course of the disease. The results are sent to a gastroenterologist who prescribes therapy.
Other methods
In addition to ultrasound, the following methods are used to diagnose pathology:
- a gastroenterologist collects an anamnesis of the disease based on complaints from parents and clinical signs identified during examination of the child;
- fiberoscopy is prescribed;
- radiography.
Symptoms of the disease in newborns
From the very first feedings, parents notice that the baby often spits up. Even if you hold the baby upright, the number of regurgitations does not decrease, but rather increases. Then vomiting and other symptoms appear. The most common symptoms for pyloric stenosis in newborns are as follows:
- Vomiting 20-25 minutes after feeding. The volume of vomit is greater than the volume of milk consumed. There may be a sour smell.
- The child urinates little. The color of the discharge is deep yellow with a pungent odor.
- Stools are rare, in small portions. The color of the stool is dark due to the large amount of bile.
- The baby quickly loses weight, becomes lethargic and capricious.
- When examining the abdomen, you can notice the characteristic “hourglass” sign. This is the name given to two protrusions of the abdominal wall, between which there is a thin bridge.
- The fontanel begins to sink, the skin becomes flabby and loses elasticity.
- The child looks hungry, facial features become sharper.
The clinic is growing gradually. One after another, there are three stages of disease development:
- compensation;
- subcompensation;
- decompensation.
Compensation
Pyloric stenosis in newborns at this stage manifests itself little. The baby may be fussy. He's probably worried about nausea and heaviness (but he can't talk about it yet). After vomiting, he feels better for a short time. The stomach increases in volume and actively contracts to “push” food through the narrowed opening of the pylorus.
Subcompensation
Vomiting occurs several times a day. The child quickly loses weight, becomes lethargic and inactive, and does not breastfeed well. He is bothered by abdominal pain (paroxysmal, reminiscent of colic). Belching has a rotten smell. Contractions of the stomach wall become noticeable when examining the abdomen.
Decompensation
Fountain vomiting. Symptoms of dehydration increase: pale skin and decreased elasticity; dry tongue; blood pressure drops. An enlarged stomach protrudes through the abdominal wall.
Important! If a child begins to spit up after every feeding and/or vomits several times a day, there is no need to wait until the condition becomes critical. The sooner the doctor makes a diagnosis and prescribes treatment, the better the baby will endure the operation and recover faster. Self-diagnosis is not acceptable.
Causes of pyloric stenosis
Doctors have different opinions about why the defect develops. More and more studies confirm a genetic predisposition to the disease. Inheritance is recessive, sex-linked.
But there are several factors that can also contribute to the occurrence of an anomaly. These include:
- Severe toxicosis in the first trimester of pregnancy.
- The use of medications (especially antibiotics) in the early stages of pregnancy.
- Some viral infections (herpes virus, cytomegalovirus, rubella, etc.).
- Disturbed hormonal levels during pregnancy.
- Mother's use of alcohol or drugs.
How to determine pyloric stenosis in infants?
Diagnosis begins with anamnesis. The doctor finds out the symptoms and the time of their onset: how quickly the condition worsens, whether there are cases of pyloric stenosis among relatives and other questions.
Next, the doctor examines the child. In the upper part of the abdomen, the stomach (sometimes the pylorus) is clearly palpated and its peristalsis is felt. The lower parts of the gastrointestinal tract are in a collapsed state.
In a clinical blood test, the number of erythrocytes (red blood cells) and hemoglobin is increased, and the ESR is decreased.
The examination necessarily includes gastroscopy (examination of the stomach using a special probe), ultrasound and radiography with contrast (barium suspension). Initial signs of pyloric stenosis:
- Barium does not leave the stomach into the duodenum for half an hour or more.
- Deep peristaltic waves.
- The contrast remains in the stomach for more than a day.
At later stages, the walls of the organ stretch and the waves decrease.
It is necessary to distinguish pyloric stenosis from other diseases in which an infant may vomit. Differential diagnosis is carried out with the following pathologies:
- Diaphragmatic hernia,
- Achalasia (or chalasia) of the esophagus,
- Meningitis (especially purulent),
- Pylorospasm.
Diagnosis of pyloroduodenal stenosis in newborns
This pathology requires the following diagnostic measures:
- Conversation with the baby’s parents about the presence of certain diseases. The doctor also clarifies how long the child’s anxiety symptoms have been present, whether they have changed over time, and whether they are related to feeding.
- Initial examination of a small patient . The specialist pays special attention to the upper section of the abdomen. With pyloric stenosis, pulsation will occur in this section. In some cases, palpation confirms the presence of a dense, plum-like form of the pylorus. If the oral cavity and lips are dry, the fontanelle is sunken, and there are no active movements on the part of the child, dehydration is diagnosed. At this stage, the doctor also weighs the baby, determining the intensity of his weight loss.
- Laboratory blood test. Using a general blood test, the level of hemoglobin and ESR is determined: with pyloric stenosis, the first indicator will be slightly overestimated, and the ESR will be slowed down. Biochemical blood testing is necessary to determine the level of chloride and sodium in the body.
- The use of ultrasound to study the pyloric canal, as well as the contents of the duodenum. Today, this technique is the most popular in diagnosing the disease in question.
- Fibrogastroduodenoscopy. It is carried out in a hospital setting by specialists who have experience working with newborns. FGDS is prescribed only in situations where ultrasound diagnostics turned out to be uninformative.
- X-ray of the peritoneum is not used so often these days, due to the availability of more gentle and informative diagnostic methods. In the event that the procedure in question is nevertheless resorted to, preference is given to radiography using barium sulfate. This contrast agent is mixed with breast milk and given to the baby to drink. In the absence of pathological conditions, such a substance is eliminated from the stomach on average within 3 hours. If barium lingers in the stomach for a day, this indicates the presence of pyloric stenosis.
At the time of diagnosis, it is very important to differentiate pyloric stenosis from pyloric spasm , which are similar in their symptoms.
The thing is that pylorospasm does not require surgical intervention, and can be quite successfully treated therapeutically. With this disease, disturbances occur in the nervous system of the pylorus, but its muscle layer is not transformed.
Video: Pyloric stenosis, pylorospasm, what is the difference?
Treatment methods
Congenital pyloric stenosis in children can only be treated with surgery. With pylorotomy (dissection of enlarged pyloric muscles), the patency of the sphincter is restored, and food easily passes into the duodenum.
How long preoperative preparation will last depends on the severity of the patient: most often it is 2-4 days. Before intervening, doctors need to:
- Correct the water-electrolyte balance, replenish the loss of fluid and ions.
- Add parenteral nutrition (intravenous administration of vitamins, glucose and other necessary substances).
- Start treatment for aspiration pneumonia (if it develops).
- Provide additional therapy for other diseases and abnormalities (if any).
Pyloric stenosis cannot be treated with herbs, spells and other methods of traditional medicine. If you delay visiting a doctor, death from dehydration is possible.
What is the danger
First of all, due to a decrease in contractility, food is not able to be evacuated normally, and the stomach itself is stretched. The contents need to go somewhere, so frequent vomiting occurs, and as symptoms increase, they literally gush out.
Narrowing of the pylorus disrupts the normal functioning of the digestive tract and is life-threatening. In the central photo below you can see the “hourglass” symptom, when the stomach protrudes in the form of two tubercles
Along with vomit, fluid loss occurs, as a result of which the water-electrolyte balance is disrupted, the blood thickens, and the body lacks vitamins and microelements. All children experience alkalosis (a shift in blood pH towards alkalization). The disease, left to its own devices, is fatal.
Surgery for pyloric stenosis in newborns
The most common intervention is Frede-Ramsted pylorotomy. Its peculiarity is that the outer serous membrane is dissected along the entire length of the pylorus. Then the enlarged muscles are separated (without cutting!) until the gastric mucosa appears in the wound. They try to avoid wounding this membrane, since the resulting bleeding is more difficult to stop and after surgery, gastric contents may leak into the abdominal cavity.
If a dissection of the mucous membrane has occurred, then the wound is sutured (in layers), and a new incision is made one cm from the old one. After the intervention, the patient is given drainage (special tubes through which fluid flows from the abdominal cavity) and prescribed a course of antibiotics.
They begin to feed the child in the early postoperative period. After two hours, he is given 10 ml of glucose to drink, and after another hour - 20 ml of expressed breast milk. From days 1 to 5, feeding occurs every two hours. The volume of food increases by 100 grams per day. From the 5th day they switch to seven meals a day (every 3 hours with a break at night). After a week they begin to apply it to the breast.
Recovery after surgery takes 7-8 days. Pyloric stenosis in newborns, when surgery is performed on time, has a favorable prognosis. With age, only a scar on the abdomen will remind you of the problem.
Treatment
The earlier the correct diagnosis is made, the sooner treatment can begin: in this case we are talking about surgical intervention. The operation is urgent, but still requires preparation. Therefore, it is usually carried out 2-3 days after diagnosis.
Preoperative preparation includes restoring water and electrolyte balance and replenishing micronutrient deficiencies. To do this, the child is infused with various solutions. If there are concomitant inflammatory diseases, treatment with antibacterial drugs is prescribed.
The main task of surgeons is to restore the lumen of the pylorus, but at the same time keep the stomach intact
Pylorotomy (the so-called operation when the pylorus is dissected) is performed according to the Frede-Ramstedt method. As the anatomical obstacle to the evacuation of chyme is eliminated, the patency of the pyloric canal returns to normal. Feeding with breast milk (or formula) in the postoperative period is dosed. That is, the baby is fed often, but in small portions. If everything went well, little patients are discharged home for 8-9 days.
What is the difference between pyloric stenosis and pylorospasm?
Pylorospasm is a pathological condition in which the pyloric muscles are toned for a long time and do not allow food to pass from the stomach into the intestines.
The occurrence of spasm occurs when nervous regulation is disrupted. The disease is functional, since there is no organic damage.
Manifestations of the disease are very similar to pyloric stenosis. Regurgitation, then vomiting, dehydration and nutritional deficiency. But there are significant differences.
| Differences between pyloric stenosis and pylorospasm | ||
| sign | pylorospasm | pyloric stenosis |
| Time of onset of symptoms | Immediately after birth | From the second week of life |
| Volume of vomit | Less food eaten | More food eaten |
| How does weight gain happen? | There is weight gain, but less than normal | Weight drops sharply |
| Skin condition | Normal | The skin is flabby, the density is reduced, the color is grayish |
| Bowel movement | Regularly, normal color | Tendency to constipation. The color is dark due to the large amount of bile |
| Therapy | Relieving muscle spasms with medications, restoring nutritional deficiencies | Operation only |
Diagnostics
A preliminary diagnosis can be made by a neonatologist in the maternity hospital or a local pediatrician during the next visit. In the case of pyloric stenosis, noticeable peristalsis of the stomach attracts attention. When stroking, an hourglass-shaped protrusion appears in the epigastric region. This symptom is one of the leading ones and makes it possible to distinguish pyloric stenosis from pyloric spasm in the early stages.
To clarify the diagnosis, the following methods are used:
- Ultrasound
Ultrasound examination with pylorospasm reveals noticeable thickening and stretching of the pylorus of the stomach (length more than 14 mm, thickness more than 4 mm).
- Endoscopic examination
Fibrogastroduodenoscopy is performed in a hospital and only if the diagnosis could not be established during ultrasound. The procedure is performed under local or general anesthesia. With FGDS, the doctor can see the narrowing of the pylorus, and also find out the possible causes of this condition.
If pyloric stenosis is suspected, consultation with a pediatric surgeon is mandatory.
Consequences and problems of pyloric stenosis in children
The most dangerous symptom of the anomaly is vomiting, since with it the child loses a lot of fluid. Dehydration leads to thickening of the blood, increased risk of blood clots, imbalance of electrolytes, increased heart rate, and disturbances in the functioning of the nervous system.
When vomiting, stomach contents can enter the respiratory tract and aspiration pneumonia develops.
The child does not receive the necessary nutrients and becomes weaker, his immunity decreases. Any infection can be complicated by sepsis (sometimes fatal).
What is pylorospasm?
Pylorospasm is a contraction of the pyloric part of the stomach due to a violation of its innervation. He also needs treatment, but only conservatively. How can it be distinguished from pyloric stenosis?
| Pyloric stenosis | Pylorospasm |
| As a rule, symptoms become more pronounced 3-4 weeks after birth. | Symptoms are visible immediately after birth. |
| Persistent weight loss. | Weight is gained according to the norms. |
| The skin is loose due to dehydration. | The skin is normal. |
| Tendency to constipation and scanty stool. | Regular bowel movements. |
Recommendations for child nutrition
After the operation, you do not need to follow a special diet. The functions of the stomach are restored completely. It is only recommended to use common sense and UNICEF standards:
- Until six months, complementary foods are introduced only as prescribed by a doctor.
- Any formula (even the most balanced) will not replace breast milk.
- Breastfeeding up to two years and older.
- Proper storage and processing of products.
- As the child grows, add new foods and dishes.
- During illness, you need to give your child more to drink and not force him to eat.