Nutrition for stomach cancer can help treatment and speed up recovery, reducing the manifestations of nutritional deficiency, which is typical for patients at all stages of treatment and after its completion.
Proper nutrition for stomach cancer is more than dietary food, it is a therapeutic effect to increase the effectiveness of therapy - nutritional support.
- Proper nutrition for stomach cancer
- Recommended foods for stomach cancer
- Prohibited foods for stomach cancer
- Daily menu options
- Nutrition during and after chemotherapy for stomach cancer
- Nutrition in the early stages of stomach cancer
- Nutrition for inoperable cancer in advanced stages
- Nutrition after treatment
- Nutrition before and after stomach cancer surgery
- Preventive diet
Proper nutrition for stomach cancer
The correct diet during different periods of carcinoma development and its treatment has significant differences, so when preparing for surgery, one menu is selected, after chemotherapy, another is prescribed, and as the process progresses, a third is required. What unites the periods is the need to regularly change the dietary regimen in favor of therapeutic nutrition, that is, adjusting the menu and meal times in order to increase the effectiveness of treatment.
Therapeutic nutrition or nutritional support is not the same as dietary, when the menu is compiled based on the patient’s diseases and with an eye to maximum harmlessness in order to avoid exacerbations. The dietary regimen is always gentle and non-provoking, nutritional support is a therapeutic effect using a set of products compiled adequately to the needs of the patient and additionally saturated with elements missing from the body - proteins, vitamins, microelements.
The vast majority of patients with stomach cancer have a lack of certain nutrients - proteins and microelements; every sixth patient at the time of diagnosis is underweight, that is, has already lost weight due to the disease.
There are plenty of reasons for insufficient absorption of nutrients in the body of a stomach cancer patient:
- Impaired functioning of the stomach due to cancer infiltration of the walls, ulceration of the mucous membrane and improper production of gastric secretions, leading to inadequate absorption of nutrients and the development of metabolic disorders.
- Reduced food volume due to stomach deformation, appetite disturbances and pain, as well as removal of part or all of the organ.
- The influence of cancer on all processes in the body due to the release of aggressive substances and robbing normal cells of proteins and microelements.
- The damaging effects of treatment are adverse reactions of chemotherapy leading to loss of nutrients with vomiting and diarrhea.
- The negative impact of psychological stress accompanying diagnosis and all stages of treatment.
At different periods of tumor development and at different stages of therapy, one mechanism of nutritional deficiency may prevail or several may be combined; depending on them, the diet and its volume, the time of food intake and its constituent elements should change.
Not a single patient is able to make adequate adjustments to their menu; this requires not only blood tests, but also the knowledge of a nutritionist with experience working with cancer patients.
Nutrition during and after chemotherapy
Chemotherapy is an integral part of the treatment of stomach cancer. The use of cytostatics negatively affects not only cancer cells, but also the entire body as a whole, weakening it and disrupting the normal functioning of organs and systems.
As a result of treatment, changes in taste and olfactory sensations, inflammation in the oral cavity, difficulty and pain when swallowing, nausea, vomiting, and stool disorders are possible.
Food should be as gentle as possible, but at the same time nutritious, in order to effectively compensate for the lack of essential substances and help the body recover faster.
In the first days of treatment, when the side effects of chemotherapy are most pronounced, food is consumed in liquid form, then gradually pureed foods are included in the diet.
Excluded:
Spicy, salty dishes, spices, alcoholic drinks - everything that irritates the mucous membranes of the gastrointestinal tract.
Nutrition must provide sufficient protein, which is necessary for the construction of new cells. Optimally suited: turkey, beef, liver, low-fat fish and seafood.
It is necessary to drink more fluids, as treatment is often accompanied by diarrhea. Various fruit drinks, compotes, jelly, natural juices, and rosehip infusions are allowed.
Slimy oat and rice porridges and vegetable broths are recommended. It is useful to include buckwheat, lentils, and fermented milk products in your diet: fresh kefir, natural yogurt, low-fat sour cream.
For inflammatory phenomena of the mucous membranes, it is recommended to drink herbal teas and infusions with sage and chamomile. They have a beneficial effect on mucous membranes damaged as a result of chemotherapy, providing an anti-inflammatory and healing effect.
The diet must include soft-boiled quail and chicken eggs or in the form of steam omelettes.
If any product causes disgust, then it is not recommended to use it forcefully. You should consult your doctor and find an alternative.
Recommended foods for stomach cancer
There is no clear understanding of the causes of the development of stomach cancer, and no cause-and-effect relationship with food consumption is seen. Modern oncology indicates the etiological influence of certain toxic substances on the development of cancer of the esophagus or intestines, but not the stomach. There are no foods that are especially beneficial for cancer patients; no specific nutritional diet has been developed for any cancer disease.
When selecting therapeutic nutrition, the patient’s initial nutritional status is taken into account: compliance with the weight standard (BMI, waist circumference), the ratio of muscles and fatty tissue, the sufficiency of blood proteins and microelements.
If there is a lack of protein, a menu with the addition of a special nutritional mixture is necessary. If there is dissonance between the protein fractions of albumin and globulin, the set of products and the type of nutritional mixture are changed. If during treatment the excretory function of the kidneys changes, then adjusting the food supply will become a vital necessity.
Proper nutrition for a patient with stomach cancer is a currently necessary and balanced food set, enriched with the missing elements from nutritional mixtures, which is what is required today to maintain strength and fight the tumor.
Authorized Products
Fruits and vegetables, frozen in winter, should be present daily in the diet of a cancer patient. Vegetable and fruit juices with pulp are extremely useful; they improve intestinal motility and promote the rapid removal of toxic substances and decay products from the body. You can also prepare vegetable salads, purees, casseroles.
The most useful fruits are red and orange in color. They contain carotenoids - substances with high antitumor activity.
Vegetables that help fight cancer
Cabbage is rich in ingredients that slow down the growth of cancer cells. The vegetable is useful in any form, but it is preferable to eat fresh cabbage or after short-term heat treatment in order to preserve the beneficial substances as much as possible.
Tomatoes contain high amounts of lycopene and antioxidants, which have anti-cancer properties and prevent cell damage.
Beets reduce the side effects of chemotherapy drugs. The vegetable is consumed in the form of side dishes or juice. You should not drink freshly squeezed beet juice, as it can cause nausea and a sharp drop in blood pressure.
To prevent unwanted effects, the drink is placed in the refrigerator for several hours and only then drunk.
Beetroot juice can be mixed with fresh apple and carrot juice and drink a fruit and vegetable cocktail on an empty stomach, starting with one tablespoon, as individual intolerance is possible.
Beets that have undergone heat treatment partially lose their medicinal properties.
Pumpkin is rich in vitamins and minerals such as copper, iron, zinc, which are essential for weakened cancer patients. Pumpkin can be eaten boiled as a side dish or made into porridge from the vegetable.
In addition to vegetables, the following products are recommended:
- Boiled eggs soft-boiled or in the form of a steam omelet.
- Lean meats and fish.
- Hard cheese, mild.
- Soy products.
- Vegetable broths.
- Fermented milk products, low-fat cottage cheese.
- Onion garlic.
- Vegetable, olive, butter.
- Bread made from premium flour.
- Herbal teas, jelly, natural juices, compotes, fruit drinks, still mineral water.
Prohibited foods for stomach cancer
There is no evidence of the existence of products prohibited for cancer patients. Of course, with inflamed mucous membranes, ulcerations and inadequate production of gastric juice, you should avoid irritating foods: marinades, sauces, spices. It is advisable to eat dishes that are not spicy, not sour, not hard, without crusts and seeds. But porridge from morning to evening is not a solution to the problem, but rather aggravates it by excluding from the diet the proteins and fats necessary for building tissue.
In each period of illness, the patient needs a list of foods that are currently undesirable for consumption, changing in accordance with the nutritional status, the consequences of treatment measures, the main thing is compliance with the current condition and the urgent needs of the body. A doctor at a European clinic will help you create such a list.
Reviews and results
The diet includes an extensive list of foods and different ways of processing them (except frying). Therefore, it can be diversified with new dishes. Since the food contains the physiological norm of protein and fat, it can be prescribed for a long time.
Feedback from patients indicates that therapeutic nutrition has become the norm for many people during their illness, and deviation from it immediately affects digestion. You can diversify it with new dishes, and it will not seem monotonous.
- “... Proper nutrition is the only way out for this disease after surgery to remove most of the stomach and chemotherapy. The slightest deviation or increase in portions immediately affects your health: diarrhea, bloating and abdominal discomfort. Over the course of a year, I studied my body and its reaction to food. I tolerate food well, but cooking gives my wife some trouble - I have to cook separately. I can eat something from the common table. I’m already used to steamed cutlets, it’s good that you can add dill and garlic to them - it doesn’t turn out so cloying. Sometimes I have a desire to eat smoked food, but then I feel bad”;
- “... After the operation I had to follow a therapeutic diet for a long time, probably 8 months. Now my condition is normal (I came in on time and had a successful operation), so I have expanded my diet somewhat - I can drink coffee, a piece of fried meat, and some sweets. The illness itself, the operation and dietary restrictions affected my weight - I lost 7 kg, and given my weight this is very good. I take great care of my diet and treatment so that there is no relapse”;
- “... 2 years have passed since the operation - they say this is a good time. I feel good, I started eating right and avoiding constipation, I drink a lot of water. The doctor warned me that the longer and stricter I follow the diet, the lower the risk of relapse. I’m trying really hard because I don’t want to go through everything again.”
Daily menu options
It is impossible to write out a menu for all occasions for a patient with stomach cancer; there should not be a standard list of dishes for all days, like hospital menus compiled for the week. A monotonous diet cannot be correct simply because the human body and psyche requires dietary diversity. However, there are three standard diets that take into account the nutritional needs of a certain body weight, digestive and metabolic disorders.
All options involve additional enrichment with dietary fiber, vitamins and microelements based on the individual needs of the patient. All dishes are prepared by boiling or steaming, stewing or baking, served not hot and not iced 4 to 6 times a day. The volume of nutrients and energy value, the amount of liquid and indications for prescription vary:
- An option for a patient with normal weight, without obvious metabolic and digestive disorders - physiological content of proteins, fats and carbohydrates, up to 2 liters of liquid and no more than 2400 kcal.
- The option for patients with underweight, after chemotherapy and surgery, involves a high content of proteins, fats, complex carbohydrates with a limitation of easily digestible sugar, normal fluid intake and high calorie intake - up to 3600 kcal.
- An option for disorders of metabolism and excretion of metabolites, that is, with metastases in the liver or renal disorders, after chemotherapy with platinum drugs. Protein, salt and liquid are limited, there is no place for pickles, alcohol and chocolate, but the starchiness of dishes increases with almost standard calorie content.
The list of specific dishes should be based on their nutritional value and the patient’s gastronomic preferences; eating without pleasure just for the sake of a biological need also does not help treatment, like fasting.
Features of digestion in patients
After removal of the stomach for cancer, as after any other surgical operation on the digestive organs, the main task of doctors and the patient is to organize proper rehabilitation and form new eating behavior. Without this factor, all the doctors’ efforts will be in vain: no matter how timely and no matter how high-quality the resection is done, there will be no result without a successful recovery period. And on the contrary: after operations to remove cancer on the gastrointestinal tract, it is diet that can lead to recovery to a much greater extent than medications.
Nutrition after removal of the stomach due to a malignant tumor undergoes dramatic changes:
- in terms of the amount of one-time volume - the capacity of the stump of the stomach or the part of the small intestine that plays its role is small after the cancer is removed, so the portions become significantly smaller;
- in terms of nutritional quality – it is vital to provide adequate nutrition with sufficient protein and carbohydrates, a limited amount of fat, and a ban on certain foods;
- according to the method of preparation - lifelong dietary restrictions after removal of stomach cancer to frying, smoking, salting foods;
- according to the frequency of eating episodes during the day - it is recommended up to 8 times a day, long breaks are unacceptable.
Nutrition during and after chemotherapy for stomach cancer
Chemotherapy for stomach cancer has become the standard of care. It is used before surgery and after the surgical stage for a total of two months, with metastasis it lasts more than 4 months. Effective drugs are toxic to the mucous membranes (fluorouracil), the nervous system (taxanes) and the kidneys (platinum derivatives).
Platinum drugs have an affinity for nervous tissue and impair renal function, causing nausea and vomiting even against the background of antiemetics. Damage to the mucous membranes of varying severity - mucositis - lasts for more than a week, significantly limiting the very possibility of nutrition, permanently and negatively changing the nutritional status of the patient.
Cancer patients tend to be underweight, and chemotherapy exacerbates cell and tissue loss. Immediately after the course and for a couple more days, due to nausea, there is no desire to eat, and on the fifth day it is no longer possible to eat due to inflammation of the mucous membranes, sometimes complications are accompanied by diarrhea.
Chemotherapy should be approached prepared so as not to aggravate nutrient deficiency and the associated protracted recovery with the addition of infections. Preparation consists of developing a long-term strategy for proper nutrition, with the possibility of adjusting the plan if complications develop.
Baby formula or cereal cannot meet the needs of an adult. The use of enriched nutritional mixtures during this period is the norm; it is important to choose the right composition and volume. A diet developed by a specialist will help improve your well-being and quickly restore damaged tissue.
Principles
Nutrition after gastric resection for cancer involves adherence to a number of general simple principles.
In the first two days after surgery, intensive therapy is carried out, during which the patient is allowed to eat only through the intravenous administration of special solutions. Parenteral nutrition should be prescribed for each patient individually, and it is important to take into account the individual characteristics of the body.
The duration of the diet should be at least four months. If complications develop during this period, the diet is extended. At this time, the diet should be as complete as possible. It should consist of a large amount of fats, proteins and carbohydrates, but mechanical and chemical irritants should be completely excluded.
It is necessary to move from crushed food to regular food at a slow pace. Adding new products should be done gradually in small doses. At the same time, it is necessary to monitor how the body will react to innovations.
Only the attending physician can prescribe a diet after gastric removal.
On this topic
- Oncogastroenterology
First signs of rectal cancer recurrence
- Natalya Gennadievna Butsyk
- December 3, 2021
When the main rehabilitation period ends, the patient’s body should receive at least 300 grams of carbohydrates, 140 grams of protein or 100 grams of fat with food. Daily calorie content – from 2800 kcal.
All dishes consumed are prepared exclusively in a steam bath or by boiling and stewing.
Food can only be consumed when its temperature reaches no more than 55 degrees. If vomiting begins after warm meals, they are replaced with cooled ones.
Often, cancer patients begin to develop hypercalcemia - this is a pathological condition accompanied by an increase in the concentration of calcium in the body. In such situations, reduce the consumption of dairy products and increase the amount of meat and fish.
As for the drinking regime, you need to be as careful as possible. If the kidneys are functioning normally, then you can drink up to two liters of fluid per day. Only one glass of water is allowed at one time.
On this topic
- Oncogastroenterology
What kind of pain occurs with rectal cancer?
- Olga Vladimirovna Khazova
- December 3, 2021
You need to eat in small portions in 5-6 meals. To increase appetite, experts recommend eating food in the fresh air. In addition, you should try to eat at the same time. This will improve the digestion process, which will prevent irritation of the mucous membrane.
It is important to give up on-the-go snacks and dry food. These habits will further damage your digestive system.
Nutrition in the early stages of stomach cancer
Early gastric cancer is a tumor lesion within the mucous membrane and less than 2 centimeters in length, usually without ulceration. The minimal lesion is asymptomatic, in most cases it is found during preventive endoscopy or clinical examination.
During this period, disturbances in nutritional status are unlikely unless the patient has other chronic diseases, so there is no need for dietary restrictions. The menu should be based on the principles of proper nutrition, taking into account gastronomic preferences and concomitant chronic diseases.
Diet after chemotherapy
After chemotherapy, the patient's diet should include easily digestible and high-calorie foods. This is due to an increased gag reflex and decreased appetite. Particular attention should be paid to the following products after chemotherapy:
- sprouted grain – accelerates the regeneration of the epithelium, saturates the body with essential microelements and enzymes;
- beekeeping products – strengthen the patient’s immunity, coat the walls of the stomach, helping to reduce irritation of the mucous membrane;
- cabbage;
- pumpkin – contains vitamins and microelements that contribute to faster recovery of the body.
Basic principles of nutrition after chemotherapy
- it is necessary to prevent the processes of bloating and nausea, so the liquid should be consumed between meals;
- the food consumed must have a liquid, fine consistency;
- you need to eat only when you really want to eat;
- It is recommended to use heat treatment methods such as boiling or baking.
Properly selected nutrition after surgery will help the patient quickly improve the functioning of the stomach, intestines, liver and restore suppressed immunity.
After gastric surgery, the patient can completely switch to a normal diet after 6 months. The transition from crushed to chunky food should be done gradually so as not to create stress on the intestines. During this period, experts recommend consuming lactic acid products and vegetable juices as much as possible. It is the dairy diet after surgery that allows the body to produce the necessary enzymes for digestion of food.
Often, if the diet is not followed, the growth of cancer cells continues, and the patient’s condition worsens. To prevent the recurrence of stomach cancer, you need to follow a diet throughout your life.
Nutrition for inoperable cancer in advanced stages
It is a difficult time for a cancer patient, when the need of cancer cells for nutrients increases, chronic tumor intoxication deprives one of appetite, and the functions of the digestive tract organs decrease, making it impossible to satisfy the increasing demands for structural elements and energy.
The vast majority of patients develop anorexia-cachexia syndrome:
- progressive weight loss with decreased and perverted appetite - anorexia;
- insufficient food intake forces the body to take proteins from muscle tissue, causing muscle atrophy and reducing physical activity;
- the functions of all body systems decrease to the point of failure - cardiac, liver, and so on;
- a general inflammatory reaction and metabolic disorders develop.
Stages of the syndrome:
- precachexia - loss of about 5% of initial weight over six months in the presence of anorexia and inflammation;
- cachexia - large weight loss with a decrease in muscle mass and an increase in other signs of trouble;
- refractory cachexia - all symptoms have worsened so much that there is no response to treatment.
During this period, it is very important not to give up eating by mouth, that is, enteral nutrition , and always enrich the diet with nutritional mixtures. But there is a high need for intravenous administration of nutrients - parenteral nutrition . In case of gastric obstruction, a tube method of administering nutritional mixtures is used. Parenteral nutrition is more convenient and creates a state of rest in the stomach, but less proteins are absorbed, so the volumes of administered solutions are more significant than when combined with enteral nutrition. Without the participation of a nutritional support specialist in treatment, the success of treatment for anorexia-cachexia syndrome and the improvement of the patient’s well-being are not expected.
Nutrition after treatment
The diet after completion of therapy is determined by the body’s capabilities and losses incurred, mainly by the volume of the remaining stomach.
A sharp reduction in the stomach leads to the development of pathological syndromes, the most unpleasant of which is dumping syndrome; they try to prevent its development by modifying the operating technique. A few months after partial resection, the gastric wall will stretch and you can return to your normal routine and diet, however, weight loss is inevitable in the first 2 years due to the inability to consume adequate amounts of food and insufficient absorption.
After gastrectomy, not only a dietary, but also a therapeutic diet is necessary, strictly individual and for life.
Additional use of chemotherapy can affect the functions of other organs, in particular the liver and kidneys, which also requires drug adjustment and first therapeutic, and when the condition improves, a dietary menu that prevents exacerbations. An experienced nutritional support specialist will help you quickly overcome the consequences of treatment.
Nutrition after gastric resection (removal)
During gastric resection, the patient should adhere to the general rules of nutrition for cancer. However, the peculiarities of human nutrition after resection have been established. Rules that are recommended to be followed when the stomach is removed:
- Food should be warm, but not higher than 37 degrees, with a semi-liquid consistency.
- Try to process food with saliva and hold it in the mouth a little before swallowing.
- Eat only approved foods.
- Eat small portions at two-hour intervals.
- Drink half an hour after eating food.
- Eliminate sugar and sugar-containing products.
- Drink at least two liters of water per day.
- Observe calorie content: for women 1500 kilocalories, for men 2000.
After removal it is allowed to eat:
- Protein-containing foods: eggs, chicken breast, white fish.
- Vegetable puree soups.
- Cereals reduced to the state of overcooked porridge.
- Yogurt, kefir, milk, fermented baked milk and other dairy and fermented milk products.
- Vegetable and fruit salads.
- Pumpkin – removes cholesterol from the body and creates optimal digestion.
Sample menu after removal of the stomach for cancer:
- Breakfast: still mineral water with a drop of lemon juice - to awaken the metabolic processes of the human body.
- Second breakfast: vegetables or fruits + a glass of kefir.
- Lunch: smooth puree soup, fresh vegetable salad, boiled lean meat.
- Afternoon snack: biscuit, various types of nuts, honey, fruit or dried fruit compote, juice.
- Dinner: rice porridge, baked vegetables, boiled meat, processed until smooth.
Nutrition before and after stomach cancer surgery
Surgery is stressful for the body, especially for gastrointestinal cancer; the consequences are more severe when several weeks of preoperative chemotherapy are performed.
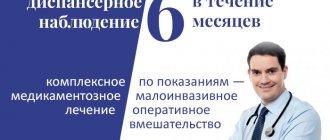
A patient with a pronounced decrease in nutritional status is not subject to surgical treatment. Therefore, over the course of a week or two, he is actively prepared for surgery with intravenous administration of nutritional solutions and enrichment of meals with nutritional mixtures, and only when protein metabolism indicators are restored is he taken for surgery. High-quality preoperative nutritional preparation can reduce the likelihood of complications and speed up the patient’s recovery.
After surgery, the body’s need for “building materials” and energy sharply increases, so the tactics of as early as possible postoperative nutrition with enriched mixtures have been adopted. If there is an initial violation of the nutritional status, already 6 hours after the operation they resort to the introduction of mixtures through a tube, and a day later the patient’s menu is expanded with additional volumes of mixtures. Sometimes it is possible to avoid probing if the patient drinks mixtures on his own and is able to swallow in the first 12 hours after the intervention. Normally, by the end of the week the patient is able to eat independently.
The duration and “aggression” of postoperative nutritional support depends on the volume of intervention, the initial condition and concomitant diseases of the patient.
The therapeutic diet is completed with an increase in weight and volume of muscle mass, normal biochemistry of proteins and microelements, absence of anemia and restoration of motor activity.
Allowed dishes and ingredients
For cancer patients, doctors create a menu and select a diet based on the individual characteristics of the body. A person suffering from cancer needs to know what is acceptable to eat if he is ill.
Featured
The list of foods recommended for stomach cancer is varied. The diet is selected in accordance with the patient's taste preferences. For stomach carcinoma (the most common type), you are allowed to eat:
- Soups: from root vegetables, dairy or based on any cereal. Boil all ingredients well. Vegetables and cereals are reduced to a mushy state. The meat is ground to a puree.
- Sea fish and white meat without fat: the fish is steamed without skin. Preferable meat products:
- young bulls;
- cattle;
- lamb meat;
- rabbit;
- dietary varieties (turkey and chicken).
When preparing a meat dish, the main ingredient should be boiled or cooked using a double boiler. Dishes baked in the oven are allowed after several months of dieting.
- Porridges: rice, buckwheat, pumpkin, semolina and oatmeal. Boil with water or milk base, boil thoroughly. At first, eat semi-liquid porridge; later you can switch to a crumbly version with the addition of vegetables or curd mass.
- Eggs: in a bag or as an omelet, up to two per day.
- Dairy products – preferably low-fat:
- cottage cheese;
- whey;
- other fermented milk drinks.
- Sweets:
- jam;
- jelly desserts;
- paste;
- meringues;
- cookie.
- Berries: strawberries or raspberries. Sweet desserts are prepared from ground berries with the addition of semolina. At first, the berries are cooked a little. After several months, fresh berries are allowed.
- Fruits and fruits of vegetable plants: the most useful fruits of the citrus family, preferably red, orange, yellow colors of plants - such colors indicate the content of a large amount of pigment in the product, which prevents the growth of tumors.
- Compotes, jelly, rosehip decoction, carrot, pumpkin, apricot juice.
- Yesterday's baked goods.
- Greens: parsley, dandelion, nettle.
Prohibited
Cancer becomes a basis for bans in many products. We will have to exclude:
- Fried foods and smoked meats.
- Fatty, rich broths made from meat, fish or mushrooms (mushrooms in any form are not allowed).
- Marinated snacks, rolls.
- Drinks containing caffeine.
- Drinks containing gases and strong black tea.
- Semi-finished products.
- Red meats and fish.
- Unripe fruits and vegetables, sour berries.
- Alcohol.
- Spicy and salty.
- Sour berries.
- Fried and hard-boiled eggs.
- Peas, beans and other legumes, red peppers cause bloating.
Prohibited foods should not be eaten under any circumstances. By eating a product from the above, the patient risks aggravating his own condition, causing irritation of the esophagus and gastrointestinal tract!
Preventive diet
It has been proven that a healthy and varied diet, quitting smoking, and maintaining a normal weight along with regular physical activity help prevent cancer. There are no foods that definitely lead to malignant processes, but adequate consumption of fruits and vegetables rich in vitamins and microelements while limiting “dark” animal meat helps maintain health. This is a good prevention of malignant processes in the stomach.
Contact a specialist at the European Clinic to find out how to increase the effectiveness of antitumor treatment, as well as what diet is indicated specifically in your case.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Obukhova O.A., Bagrova S.G., Besova N.S. et al. /Assessment of the nutritional status of patients with inoperable gastric cancer at the time of initiation of antitumor treatment. Preliminary results of a prospective observational study // Difficult patient; 2018; 6.
- Potapov A.L., Dorozhkin A.D., Gamayunov S.V. and others /Perioperative nutritional support for gastric cancer: current state of the issue// Siberian Journal of Oncology; 2019; 18(6).
- Snegova A.V., Kononenko I.B., Larionova V.B. and others/Anorexia-cachexia syndrome in cancer patients//Clinical oncohematology; 2015; 2.
- Khomichuk A.L. /Optimization of nutrition for patients after gastrectomy// Questions of dietetics; 2013.
- Fukuda Y., Yamamoto K., Hirao M., et al./Prevalence of Malnutrition Among Gastric Cancer Patients Undergoing Gastrectomy and Optimal Preoperative Nutritional Support for Preventing Surgical Site Infections//Ann Surg Oncol.; Dec 2015; 22 Suppl 3.
- Weimann A., Braga M., Carli F., et al./ ESPEN guideline: Clinical nutrition in surgery // Clin Nutr.; 2021 Jun; 36(3).
Diagnostics
Diagnosis of gastric adenocarcinoma is complex and includes a number of examinations that not only help determine the type of tumor, but also the stage of the disease:
- FGDS is an examination that is carried out using a special device - a flexible endoscope. With its help, a visual examination of the gastric mucosa is carried out, and the device transmits an enlarged image of the area under study to the monitor, which makes it possible to detect minor changes in the mucosa. Secondly, the endoscope is equipped with a special manipulation system, with which you can take a piece of tissue for histological analysis and accurately determine the type of tumor and the degree of differentiation of its cells.
- Ultrasound. This research method makes it possible to clarify the size of the tumor, its relationship with neighboring organs, and the presence of metastases in regional lymph nodes.
- CT and MRI also help verify the size of the malignant tumor and its ingrowth into surrounding tissues, but the main goal is to look for metastases in the lymph nodes and distant organs (for example, the lungs).
- PET-CT (positron emission computed tomography) can detect distant metastases up to 1 mm in size.
- Determination of tumor markers CEA, CA72-4, CA19-9. In gastric cancer, these markers do not have diagnostic value as such, but if the norm is initially elevated, they can be used to monitor treatment and relapse. After surgery, the level of tumor markers should decrease, it may reach normal. If a relapse or progression of the disease occurs, it will increase again.
Dr. M.S. Burdyukov conducts a diagnostic examination of the stomach - FGDS