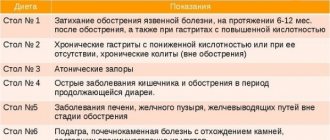
Features of the “Table 1” diet
Indications: peptic ulcer of the stomach and duodenum, as well as gastritis during the recovery period;
Duration: as prescribed by a doctor;
Features: moderation in the amount of food consumed; limiting foods that cause increased gastric secretion; Preference is given to pureed, boiled and steamed foods;
Energy value: 2300-2600 kK;
Fluid volume per day: 1.5 l;
The best type of cooking on a diet Table 1: steam or boil;
Meal frequency: eat in small portions, 5-6 times a day;
Diet “Table 1”: what is possible, what is not
Meat, poultry, fish. For meat and fish dishes, low-fat and soft-textured varieties are allowed. In other words, the meat should be tender, without tendons and skin. The ideal form of the dish is steamed meatballs, zrazy and minced meat cutlets.
Eggs. No more than two pieces per day in any form, with the exception of fried eggs. The best option is a light steam omelette with milk.
Bread and flour. You can: yesterday's wheat bread made from premium flour, as well as crackers and biscuits. Unsweetened baked goods and cookies are also allowed. The strictest ban is on rye bread and crispbread, on any fresh baked goods and puff pastry products.
Dairy products. As part of the “Table 1” diet, you can consume whole and condensed milk, as well as cream, low-fat cottage cheese, sour cream and most low-fat fermented milk products. You should be especially careful with cheese - only mild, low-fat cheese (either grated or processed) is allowed in your diet, no more than once a week.
Vegetables. Theoretically, any vegetables can be consumed, but it is important to be careful about the way they are consumed. Since on the “Table 1” diet it is important to treat the stomach walls “wounded” by ulcers as delicately as possible, fiber-rich vegetables should be boiled and turned into soft purees, light cream soups, etc.
Cereals. Allowed: semolina, oatmeal and buckwheat, as well as sticky rice. Wild and brown rice are prohibited. You can eat pasta, but they should be small in shape, ideally the smallest noodles.
Fruits and desserts. Diet "Table 1" encourages the consumption of any ripe soft sweet fruits - such as peaches, apricots, bananas, plums, etc. In addition, you can eat any fruits and berries in pureed, boiled and baked form, as well as in the form of soufflés, jelly, mousses, etc. Sweets such as marshmallows, marshmallows, bird's milk, desserts such as tiramisu, etc. are allowed. Banned are chocolate, sour berries and fruits, hard-textured fruits (apples, pears, etc.), and ice cream.
Beverages. You can: clean water, weak tea, cocoa, juices, compotes and fruit drinks from sweet fruits and berries. Not allowed: sweet soda, kvass, sour drinks, coffee, alcohol.
Additional prohibitions. It is important to understand the basic principle of the therapeutic diet “Table 1” - foods and dishes are allowed in the diet that do not irritate the damaged walls of the stomach and duodenum either chemically, mechanically, or thermally. This means that everything that enters the stomach must be of a neutral temperature, have a soft (ideally puree-like) consistency, and not be spicy, fatty, sour, or smoked. For example: a salad of white cabbage with carrots is strictly forbidden, but stewed cabbage “Bavarian style” is possible. Millet, barley, quinoa, and corn grits are prohibited from cereals. Legumes are also prohibited (except large white beans). The diet should not contain semi-finished and canned foods, pickles and marinades.
Table No. 1 for gastritis
Diets for gastritis in most cases are associated with one-sided, monotonous nutrition, monotonous taste sensations, which cause in patients not only loss of appetite, but even aversion to food.
In modern medicine, a rational diet is widely used, which combines all the positive aspects of previously existing diets, does not exclude patients from eating appetizing dishes, and can saturate with all kinds of tastes.
The name of this rational diet is table No. 1 (diet No. 1).
This effective method of treating ulcers and gastritis was developed by Soviet research by clinicians V.Kh. Vasilenko, V.N. Smotrova, M.I. Pevzner, I.S. Savoshchenko and others.
They identified the main principles of diet treatment, which ensure maximum rest for the diseased organ (stomach, duodenum), its secretory and motor apparatus, and strengthen the defenses of the human body.
Pevzner diet or table No. 1, 1a, 1b
The purpose of the diet: restore the functions of the stomach and duodenum.
Purpose:
- Chronic gastritis with increased or decreased acidity.
- Exacerbation of chronic gastritis with normal or increased secretion.
- Acute gastritis during the recovery period.
- Acute and chronic course of gastric and duodenal ulcers.
- After a relapse of exacerbation of diseases of the stomach and duodenum.
- Postoperative period.
Basic principles of diet No. 1:
- Fractional meals - 5-6 meals per day.
- Energy value per day: 2800-3200 Kcal.
- Products must be pureed, chopped and steamed or boiled.
- Minimum salt intake.
- Avoid hot and cold foods and eat them only warm.
What is table 1a and 1b
Therapeutic nutrition for those suffering from gastritis and gastric ulcers begins with the most gentle diet 1a. The diet is prescribed during the period of exacerbation of the disease for the first 10-12 days. All dishes are prepared boiled and pureed.
As a rule, the daily menu of diet 1a includes:
- Milk, jelly, jelly (non-sour);
- soft-boiled eggs (no more than three per day);
- once meat soufflé;
- once a day milk porridge: pureed, liquid;
- slimy milky cereal soups.
Bread and bread products are excluded from the diet.
Chemical composition of diet 1a (table 1a):
- proteins 75-80 g;
- fats 80-90 g, of which 25-30 g are vegetable;
- carbohydrates 200 g;
- calories 2000-2200;
- table salt only 6-8g.
This diet helps reduce reflex excitability of the stomach.
When the process of exacerbation of gastritis and peptic ulcer disease subsides, they move from the most gentle diet to a more stressful one - diet 1b.
All dishes are prepared boiled and pureed. To the products and dishes allowed by table 1a, add 75-100 g of white crackers. Meat and fish are not served in the form of a soufflé, but in a rougher culinary preparation - in the form of cutlets, quenelles, and meatballs. More often pureed milk porridges are given. Soups with this diet are no longer slimy, but cereal-based - milk-based, pureed.
Chemical composition of diet 1b (table 1b):
- proteins 90 g;
- fats 90 g (of which 30 g are vegetable);
- carbohydrates 300-350 g;
- calories 2500-2800.
When a patient suffering from a peptic ulcer shows improvement, he is transferred to diet No. 1 (table No. 1).
Diet No. 1 according to M.I. Pevzner for a day
First of all, it is recommended to eat fewer pureed dishes and more often be allowed to eat a boiled piece of meat, fish or chicken. In addition to animal fats, about 30% of the fats in the daily diet are vegetable oils (sunflower, refined, olive).
It is known that vegetable oils have a good effect on the digestive process, improve metabolism, in particular, have a positive effect on fat metabolism.
In addition, vegetable oils promote more intense bile secretion, which improves the process of food digestion.
Daily diet:
- At 8:30 for the first breakfast it is recommended: Boiled lean fish 100g and 200g mashed potatoes. Add 50g milk and 10g butter to mashed potatoes. A glass of tea with 50g of milk and 15g of sugar and a piece of day-old white bread with 10g of butter (in total, no more than 400-500g of day-old white bread is recommended per day).
- At 11-12 o'clock: Carrot puree, which consists of 200g of boiled carrots, 50g of milk and 5g of butter. A glass of tea can be replaced with rosehip decoction (20g rose hips, 200g water and 5g sugar).
- At 14:00: Milk soup with vermicelli (30g vermicelli, 100g milk, 5g butter). For the second course - steamed meat roll stuffed with steamed omelette (meat 100g, bread 20g, milk 25g, 1 egg, 10g butter); the steam roll can be replaced with minced meat or boiled chicken meat without fat. For the third - jelly from a decoction of dry black currants (dry currants 10 g, sugar 20 g, potato flour 10 g), which can be replaced with raspberry or black currant jelly, milk cream, apple jelly or baked apple from sweet varieties.
- At 17:00: A glass of tea with milk (milk 50 g, sugar 15 g), sweet crackers (bread 30 g, sugar 5 g).
- At 19:30-20:00: Cottage cheese with sour cream and sugar (cottage cheese 50g, sour cream 20g, sugar 5g), pureed milk rice porridge (rice 5g, milk 100g, sugar 5g, butter 5g), a glass of tea with milk (milk 50g , sugar 15g).
- At 21:30-22:00: A glass of milk with a small piece of bread or a soft-boiled egg (a glass of milk - 200 g).
Chemical composition of this diet:
- proteins and fats 100g each;
- carbohydrates about 800 g;
- total for the day is about 3200 calories.
What you need to know about the modern preventive diet
First of all, the patient must be convinced that only a nutritious diet will save him from the disease. Such a powerful factor as drug treatment will not be able to have a positive effect if the patient violates the dietary regime.
It should be noted that a cure for stomach disease can occur only if the patient follows a course of dietary nutrition for a long time, even during the period of improvement. The patient may feel cured, but the disease, having gone into remission, is not eliminated at all and can worsen if the diet is violated.
Menu for a week for gastritis
For those patients whose disease is in remission (the ulcer has healed and there are no clinical symptoms), the following sample menu for a week is recommended:
- Monday 1st breakfast: cottage cheese pudding and tea. 2nd breakfast: jelly, or baked apple, or a glass of milk. Lunch: mashed milk cereal soup, steamed meat cutlets, chopped schnitzel, mashed potatoes, milk cream. Afternoon snack: rosehip decoction , croutons with sugar. Dinner: meatballs baked in sour cream, carrot puree, cereal, tea. Before bed: 1 glass of milk.
- Tuesday 1st breakfast: curd cheese, semolina milk porridge, tea. 2nd breakfast: baked apples. Lunch: pureed pearl barley soup, steamed meat meatballs, carrot puree, fruit jelly. Afternoon snack: rosehip decoction, croutons with sugar. Dinner : jellied fish, pureed rice milk porridge, weak tea. Before bed: 1 glass of milk.
- Wednesday 1st breakfast: boiled tongue, pureed buckwheat porridge, milk, tea. 2nd breakfast: curd pudding. Lunch: pureed pearl barley soup, boiled beef stroganoff, mashed potatoes, compote. Afternoon snack: rose hip decoction, croutons with sugar .Dinner: noodle soup with cottage cheese, carrot-apple balls, tea. Before bed: 1 glass of milk.
- Thursday 1st breakfast: cottage cheese with sugar and sour cream, oatmeal porridge, tea. 2nd breakfast: baked apples. Lunch: fanned pureed milk soup; game meat dumplings, pureed buckwheat porridge, fruit jelly. Afternoon snack: rosehip decoction, croutons with sugar. Dinner: jellied fish, cheesecakes with cottage cheese. Before bed: 1 glass of milk.
- Friday 1st breakfast: meat soufflé, semolina milk porridge, tea. 2nd breakfast: potato soufflé with sour cream. Lunch: noodle soup with chicken broth, fried chicken, boiled rice, compote. Afternoon snack: rosehip broth, croutons with sugar. Dinner: meatloaf, stuffed omelet, carrot puree, millet casserole with cottage cheese and raisins, tea. Before bed: 1 glass of milk.
- Saturday 1st breakfast: soaked herring with boiled potatoes, crumbly buckwheat porridge, tea. 2nd breakfast: vinaigrette. Lunch: rice soup with meat broth, potato casserole with meat, apple mousse. Afternoon snack: rosehip decoction, croutons with sugar. Dinner: meatloaf stuffed with omelette, carrot puree, millet casserole with cottage cheese and raisins, tea. Before bed: 1 glass of milk.
- Sunday 1st, breakfast: curd cheese, milk porridge, coffee with milk. 2nd breakfast: pasta with grated cheese. Lunch: pickle soup with meat broth, pilaf, compote. Afternoon snack: crackers with sugar, rosehip broth. Dinner: fish aspic, apple pie, tea. Before bed: 1 glass of milk.
Daily: wheat bread made from 1st and 2nd grade flour and always rye, only 400 g, butter 10 g, sugar 50 g, table salt 12-15 2.
It should be borne in mind that when treating with diet therapy, special attention must be paid to the vitamin composition of the diet.
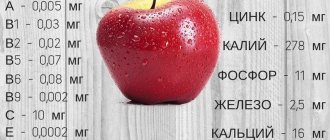
The body needs the following amounts of vitamins:
- vitamin C at least 100 mg;
- vitamins B1 and B2 about 14 mg;
- vitamin A at least 2 mg per day.
Along with the introduction of vitamins into the body with food, vitamin preparations are also prescribed in the form of injections and tablets. Table salt is given in moderation and no more than 10 g per day.
It should be noted that the above diet options are very schematic. The amount of certain food ingredients should depend on the individual characteristics of the patient (age, gender, body weight, national characteristics of the diet).
In all cases, specific recommendations for diet therapy are given by the doctor.
Table No. 1 - do's and don'ts
Diet No. 1 recommends the following dishes and products:
- Milk, weak tea with milk.
- Butter, olive, refined sunflower oil.
- Fresh cottage cheese, sour cream, Dutch cheese.
- Soft-boiled eggs, steam omelettes.
- Milk, cereal, pureed, milk soups with the addition of pureed vegetables (except for cabbage); dairy with chopped vermicelli or homemade noodles; pureed vegetables from carrots, potatoes and beets, seasoned with butter or refined sunflower oil.
- For second courses: boiled meat and fish (lean beef, chicken, pike perch, perch, etc.). You can have minced meat.
- Side dishes: pureed milk porridge and uncooked porridge, vermicelli, finely chopped pasta.
- Vegetables: potatoes, carrots, beets, pumpkin, white zucchini in the form of puree, steam puddings.
- The sauces are prepared white, milk (bechamel).
- Fruits and berries are selected from sweet, soft and non-astringent varieties. They are prepared boiled, pureed or baked (compotes, jelly, etc.).
- Among bread products, yesterday's white bread, sponge cake, and savory cookies.
- Sugar is also included in the diet.
- Vitamin drinks: raw vegetable (carrot, beetroot) and non-acidic berry juices (raspberry, strawberry with 1/3 cup added water), rose hip and wheat bran decoction.
Chemical composition of the diet:
- proteins 100 g;
- fat 100 g, of which 1/3 is vegetable;
- carbohydrates 400-450 g;
- calories 3000-3200.
When organizing diet No. 1, the following are prohibited:
- Meat, fish broths and strong vegetable and especially mushroom broths;
- fatty meats and fish;
- raw, unprocessed vegetables and fruits containing a large number of cell membranes;
- salty dishes, spicy snacks;
- canned food, sausages;
- pastry, pies, brown bread;
- cold drinks, ice cream;
- waters containing large amounts of carbon dioxide.
A course of therapeutic nutrition for gastritis and ulcers is prescribed by a doctor, its duration is individual and depends on the disease. You should switch to a more varied diet only with the permission of your doctor.
To summarize, we can say that the patient’s treatment begins from 1 month: 10-12 days the patient receives table 1a, 10-12 days 1b and then table No. 1.
The most gentle diets 1a and 1b contribute to the disappearance of pain and dyspeptic symptoms (heartburn, belching, nausea). The introduction of vegetable oil into the diet has a beneficial effect on intestinal function and constipation stops.
Diet No. 1 is followed by a person suffering from gastric ulcer for a long time (from 1 to 2 years) after he has become able to work.
Source: https://gastritoff.ru/gastrit/pitanie/stol-%E2%84%961-pri-gastrite.html
Sample menu for a day on a diet for stomach ulcers
You should eat on the Table 1 diet in fractions - 5-6 times a day. An approximate menu for the day might look like this:
- Breakfast: omelet of two eggs and milk, cottage cheese with honey or jam, tea;
- Second breakfast: fruit salad;
- Lunch: sticky rice soup, fish cutlets with vegetable puree, sweet jelly;
- Afternoon snack: a cup of cocoa with marshmallows;
- Dinner: boiled vermicelli with meat balls, salad of boiled and finely mashed beets with prunes, tea;
- 3 hours before bedtime: a glass of low-fat kefir, applesauce;
Healthy recipes for the Table 1 diet will help diversify your diet:
What does the weekly menu consist of?
The approximately weekly menu for table 1a is as follows:
Monday .
- 1st breakfast . Omelet, rice porridge + milk.
- 2nd breakfast . Milk.
- Dinner . Oatmeal milk soup, soufflé (meat), compote.
- Afternoon snack . Egg + milk.
- Dinner . Boiled buckwheat, omelette and milk.
- Before bed - milk.
Tuesday .
- Breakfast . Semolina with milk, omelet and a glass of warmed milk.
- Dinner . Rice milk soup, soufflé (pike perch), jelly.
- Afternoon snack . Omelet and warm milk.
- Dinner . Oatmeal with milk and egg.
- At night - warm milk.
Wednesday .
- 1st breakfast . Semolina in water, egg, glass of milk.
- 2nd breakfast . A mug of milk.
- Dinner . Oatmeal milk soup with egg. Soufflé (beef), jelly.
- Afternoon snack . Milk, one egg.
- Dinner . Rice porridge, warm milk.
- For the night . Milk.
Thursday .
- 1st breakfast . Semolina, milk.
- 2nd breakfast . Omelet, a mug of milk.
- Dinner . Milk semolina soup with 5 g of butter, soufflé (cottage cheese), compote.
- Afternoon snack . Mug of milk, omelette.
- For the night . A mug of warm milk (+ honey).
Friday .
- 1st breakfast . Rice milk porridge, a mug of milk, an egg.
- 2nd breakfast . A mug of milk.
- Dinner . Oatmeal milk soup, soufflé (pike perch), compote.
- Afternoon snack . Egg; mug of milk.
- Dinner . Buckwheat with milk.
- For the night . Milk.
Saturday .
- 1st breakfast . Slimy milk porridge (rice), as well as a mug of milk.
- 2nd breakfast . Egg, compote.
- Dinner . Milk oatmeal soup, soufflé (beef), jelly.
- Afternoon snack . A mug of milk.
- Dinner . Buckwheat with milk.
- For the night . A mug of milk.
Sunday .
- 1st breakfast . Oatmeal with milk (+ honey), a mug of milk.
- 2nd breakfast . A glass of warmed milk with 5 g of butter.
- Dinner . Rice milk soup, soufflé (poultry), jelly.
- Afternoon snack . Milk; egg.
- Dinner . Semolina, omelet and a mug of milk.
- For the night . Milk again.
Glutinous rice soup
Ingredients: 50 g rice, 1 chicken egg, glass of low-fat milk, 15 g butter, water.
Cooking method:
- Cook the rice until completely cooked and strain through a fine sieve.
- Add 3 tbsp to glutinous rice broth. l. boiled rice and place on low heat.
- Mix milk and egg and add this mixture to the broth. After 1-2 minutes, remove from heat.
- If desired, you can add a little grated boiled carrots and finely chopped greens to the finished dish. Before serving, season the soup with a piece of butter.
Boiled beef dumplings in broth
Ingredients: 300 g deveined beef, half an onion, 1 egg, 2-3 slices of white wheat bread, 1 tbsp. butter, 1 tbsp. sour cream, a pinch of salt.
Cooking method:
- Cut the beef meat into small pieces.
- Cut half an onion and fry in butter until golden brown.
- Soak slices of bread in milk, squeeze and mix with sour cream.
- Mix all ingredients and pass through a meat grinder. Add salt to the minced meat and, if desired, a pinch of herbs. Roll the minced meat into a thick “sausage”, wrap it in white cotton cloth, and tie it around the edges with thread.
- Place in boiling salted water and cook for 10-15 minutes. Before serving, “unwrap” the sausage, cut into pieces and place in cups with broth. If desired, you can add boiled vegetables and herbs to the broth.
Diet for gastritis with high acidity
Gastritis is an inflammatory disease of the gastric mucosa, which changes its secretory function and disrupts the proper motility of the organ. Most often, gastritis occurs in young people, because in the older generation, atrophy of cells that produce hydrochloric acid occurs over time.
There is also a connection with a person’s gender. Despite the fact that both men and women suffer from gastritis, more often the inflammation overtakes the fair half of humanity.
This is due to hormonal instability due to the presence of the menstrual cycle and mental lability also due to the “play” of hormones. It has long been proven that stressful situations are quite capable of causing inflammation. There is no mysticism in this. All human activities are regulated by the brain.
Under the influence of stress, a large number of mediators are produced, which, in turn, affect the cells of the stomach. The result is gastritis. This applies not only to problems with the gastrointestinal tract; other areas of life are at risk just as much as the stomach.
Cases of recovery from gastritis with normalization of the emotional background were recorded. Despite this, gastrointestinal diseases are more often the result of poor nutrition, which will be discussed in this article.
What causes gastritis?
The body's protective reservoirs are large, so it takes a long time for symptoms to appear. It is unlikely that gastritis will develop due to only one investigative factor. Sometimes a person leads an incorrect lifestyle for years and only then does abdominal pain make itself felt.
Inflammation of the stomach can occur when:
- Compounded heredity (you need to be especially careful if at least one parent has a history of peptic ulcer disease);
- Infection with H. Pylori (an opportunistic microorganism that begins to multiply intensively under favorable conditions);
- Poor nutrition (abuse of fatty, smoked, spicy foods, improper diet, eating before bed, etc.);
- Stressful situations;
- Systematic consumption of alcohol, smoking;
- Long-term treatment with anti-inflammatory drugs (for example, some diseases of the musculoskeletal system require lifelong use of NSAIDs, which leads to increased acidity of gastric juice);
- Chronic infections;
- Endocrine disorders;
- Hypovitaminosis;
- Worm infestation.
Doctor, everything hurts
Any inflammation is accompanied by pain, gastritis is no exception. A person complains of epigastric pain. It can have absolutely any character. Some describe it as pulling, others as aching, others as pressing, etc.
This is due to stagnation of food in the stomach and impaired motility. The second most common symptom is heartburn.
In the future, a person may complain of constipation or diarrhea, nausea, vomiting, deterioration in health, and even a rise in temperature within the subfebrile range (37-37.9).
How does gastritis occur?
The secretion of gastric juice varies throughout the day and depends on food intake. But, logically, the gastric mucosa is constantly exposed to hydrochloric acid, so why does inflammation not develop immediately? Our body is thought out to the smallest detail; protective factors help prevent gastritis. These include mucus, rapid regeneration, motor skills and good blood flow.
There are also aggression factors: hydrochloric acid, pepsin, H. Pylori. Under the long-term pressure of bad habits, the “scales break” - the traction force is on the side of the aggressive factors, the protective factors weaken and their quantity is not enough to prevent inflammation and ulceration.
It is at this stage that you need to take medications that reduce stomach acidity and go on a special diet.
Why do you need a diet?
Diet for gastritis with high acidity
is nothing more than table No. 1 according to Pevzner. The goal of diet therapy is to normalize protective factors and reduce aggressive factors.
It is strictly forbidden to completely get rid of hydrochloric acid and pepsin; an excess of antacid drugs can lead to the exact opposite result - hypoacid gastritis, which will be treated in a completely different way.
With gastritis, motility is impaired, and the secretory function is aimed at producing large amounts of hydrochloric acid and pepsin. The purpose of the diet is to eliminate disorders and normalize the processes occurring in the stomach.
Eating right
- Fasting for gastritis
with high acidity is not recommended, since the content of hydrochloric acid in gastric juice is extremely high, this will lead to ulcer formation. However, an exception may be the first day of illness, when a person suffers from nausea and vomiting. In this case, fasting is acceptable for one day.In this case, a person should drink a lot of water (about 2-2.5 liters) and take proton pump inhibitors (to reduce stomach pH).
- In the following days, it is possible to switch to dishes that are easy to digest and do not increase acidity (porridge, puree soups, low-fat dairy products, steamed food, boiled meat);
- Meals should be fractional.
The intervals between meals reach 3-4 hours, and the food itself should be easily digestible.Example:
- Breakfast (8:00) – Muesli with sweet berries;
- Second breakfast (11:00) – a glass of low-fat yogurt;
- Lunch (14:00) – rice soup, chicken cutlet, piece of bread;
- Afternoon snack (16:00-17:00) – jelly;
- Dinner (19:00-19:30) – mashed potatoes, vegetable salad, weak tea.
- Half an hour to an hour before bedtime - a glass of low-fat kefir.
- It is unacceptable to eat too hot or cold foods; Excluded from the diet at the time of exacerbation: fatty, smoked, canned food, fast food, carbonated drinks, “dry snacks” in the form of chips, nuts, seeds, etc., fatty meat.
Prohibited
At the time of exacerbation, these foods should be completely eliminated from your diet:
- Fatty fish and meat, broths based on them;
- Fatty foods, smoked foods, canned foods;
- All types of spices, seasonings;
- Fresh bakery products;
- Carbonated drinks, fast food;
- Boiled eggs;
- Fresh fruits and vegetables;
- Concentrated juices, strong tea or coffee:
- Confectionery (chocolate, candies).
Alcohol and cigarettes are also contraindicated for patients with gastrointestinal pathologies.
Tasty and healthy
Eating for gastritis of the stomach with high acidity means food that is steamed or baked with a minimum content of oils.
In case of pathology you can:
- Weak tea, tea with cream, milk;
- Bakery products from yesterday. Dried bread or crackers are well digestible and do not force the stomach to “work” more than usual;
- Lean meat, fish, ham, cheese. The main thing is that they are without spices and additives;
- Steamed, boiled or baked vegetables, fruits;
- Low acidity dairy products (milk, yogurt, fermented baked milk, sour cream, bifidok, etc.);
- Soft-boiled eggs or an omelet made from them with the addition of milk;
- Soups, puree soups, milk soup;
- Cereals (in particular, semolina, oatmeal, buckwheat and rice);
- Pasta;
- Sweet fruits, berries, vegetables after normalization of general well-being;
- Honey, sweet jam, sugar, marshmallows, marshmallows;
- Homemade juices (non-acidic), compotes, herbal decoctions.
Hypovitaminosis and gastritis
With gastritis, the absorption of vitamins is impaired, and tablet forms can do more harm than good for the already irritated gastric mucosa.
In order to improve motor skills and reduce secretory function, it is necessary to include dairy products, cereals, meat, fish, and seafood in the daily diet.
They contain a large amount of B vitamins, which help not only to recover from gastritis, but also to normalize the state of the nervous system.
Vitamins for gastritis with high acidity are necessary, but some, such as vitamin C, must be taken with extreme caution. It is found in abundance in all citrus fruits, but for gastritis with high acidity they are strictly prohibited. You can replenish the vitamin balance with a decoction of rose hips and sea buckthorn.
Attention - exacerbation
We all know that nuts contain a large amount of vitamins, many of which directly affect the proper functioning of the gastrointestinal tract.
However, they are limited in the diet to almost a few pieces per day, because eating it in large quantities can easily cause gastritis.
Needless to say about mushrooms, which contain a storehouse of useful substances, but are very difficult to digest. Outside of exacerbation of gastritis, they should be eaten very carefully, but during illness it is better to avoid them altogether.
Ice cream, cakes - you should give up all of this until you reach remission; the high content of preservatives, coupled with the low temperature of the dish, have an extremely negative effect on the stomach. This kind of sweets should be replaced with honey, jam, marshmallows, of course, in reasonable quantities.
FermentationBurning
Coarse fibers that provoke fermentation are found in corn, legumes, and pearl barley. Separately, it is worth highlighting grapes, which can and even should be included in the diet, provided that the skin is first removed from it.
Fatty meats such as pork, goose, and various smoked meats, paradoxically, reduce the acidity of the stomach, but they have a negative effect on its motor function, so they are also excluded from the diet. If you have gastritis, it is unacceptable to eat foods that contain both dough and meat.
As an example, everyone’s favorite dumplings. You can eat both separately, but together they take a very long time to digest and disrupt the functioning of the gastrointestinal tract. Despite so many restrictions, a person will still not feel hungry. There is a great alternative to dishes that won’t take you a lot of time to prepare.
Your doctor will give you a list of approved foods that you can combine with each other and eat tasty and healthy every day!
Sample menu
Monday:
- Buckwheat porridge with milk;
- A glass of low-fat yogurt;
- Ukha, two pieces of bread;
- Cheesecakes, weak tea;
- Rice with steamed vegetables.
Tuesday:
- Rice pudding;
- Sweet berry smoothie;
- Pea soup, toast;
- Skim cheese;
- Steamed pilaf with chicken, weak tea.
Wednesday:
- Oatmeal with honey and berries;
- Kissel;
- Buckwheat soup with chicken, toast, weak tea;
- Bread and compote;
- Vermicelli, vegetable salad.
Thursday:
- Muesli with berries;
- A glass of kefir;
- Cauliflower soup, toast;
- Kissel;
- Mashed potatoes with lean fish, weak tea.
Friday:
- Semolina porridge, weak tea;
- Sweet fruit dessert;
- Fish soup, toast, beef cutlet;
- Compote, dried croutons;
- Cauliflower puree, toast, weak tea.
Saturday:
- Oatmeal with honey, weak tea;
- A glass of yogurt;
- Pea soup, toast;
- Vegetable salad;
- Buckwheat porridge with chicken cutlet.
Sunday:
- Couscous with vegetables;
- Compote;
- Buckwheat soup, two slices of bread;
- Cottage cheese casserole;
- Boiled potatoes with vegetables.
Also, before going to bed, drink a glass of non-acidic dairy products that have a fresh expiration date (1-3 days).
Recipes
Despite the fact that there are a lot of restrictions with gastritis, a person can pamper himself not only with tasty, but also easy-to-follow recipes. Each of the dishes listed below does not take more than half an hour to prepare.
Syrniki
You will need:
- Low-fat cottage cheese – 500 g;
- Wheat flour - 0.5 cups;
- Egg – 1 pc.;
- Sugar – 2 tbsp;
- Vegetable oil – 2 tbsp;
- Salt - to taste.
Add sugar, egg, salt to the cottage cheese, sift the flour and mix well. Grease a baking sheet with oil, place the dough in the form of pies on it (the dough is thick and lends itself well to modeling). Bake for 25 minutes at 180 degrees in the oven.
After 25 minutes, the cheesecakes must be turned over and baked for another 5-7 minutes. You can serve cheesecakes with sour cream, sweet berries or honey. An ideal drink would be weak tea or a glass of low-fat kefir.
Bon appetit!
Potato and spinach soup
You will need:
- Spinach – 1 bunch (about 350 g);
- Water – 1 liter;
- Potatoes – 1 medium or 2 small;
- Vegetable or olive oil – 2 tbsp;
- Onions – 1 pc.;
- Salt - to taste.
Boil the onion, pre-fried in oil, until golden brown in a saucepan. Salt, add potatoes, wait 10-15 minutes, and then add spinach and leave to simmer under a closed lid for 20 minutes. You can serve it with breadcrumbs and herbs. Bon appetit!
Rice with steamed vegetables
You will need:
- Rice – 3 cups;
- Water – 5.5 glasses;
- Vegetable oil – 2 tbsp;
- Olive oil – 1 tbsp;
- Cauliflower – 1 head;
- Carrots – 1 pc.;
- Spinach – 1 pc.;
- Broccoli – 1 pc.;
- Salt - to taste.
Water is boiled in a double boiler with oil and salt, washed rice is added. Chop the vegetables and add them to the rice and simmer for 30 minutes. Salt to taste, add herbs. Bon appetit!
Pumpkin with zucchini and feta cheese, baked in a pot
Ingredients: 400-500 g pumpkin, half a zucchini, 100 g white beans, 200 g feta cheese, 2 tbsp. butter.
Cooking method:
- Pre-boil the white beans until half cooked.
- Peel the pumpkin and zucchini, cut into small cubes. Also cut the cheese.
- Preheat the oven to 200 degrees, then reduce to 180 degrees.
- Place pumpkin with zucchini, boiled beans and pieces of cheese in a pot.
- Place pieces of butter on the top layer.
- Cover the pot with foil and place in the oven. Simmer for about 25-30 minutes. Then turn off the oven, leaving the dish to simmer for about 10 minutes. If desired, you can add a spoonful of sour cream to the dish before serving.