If constipation or diarrhea occurs, the reasons may be different. Disruptions in the functioning of the gastrointestinal tract occur after illness, overeating, eating low-quality or too fatty foods, a sudden change in diet, or a long flight.
However, if these are isolated cases, there is no need to worry. After just a few days, the functioning of the digestive organs improves independently without the use of medications.
Unstable stools should cause alarm if they occur for a long time. Especially if intestinal upset is accompanied by pain and other ailments. Such signs may indicate the presence of a disease.
Irritable bowel syndrome
Constipation may alternate with diarrhea in irritable bowel syndrome. Irritable bowel syndrome (IBS) is a disorder of the gastrointestinal tract.
Malfunctions of the digestive system can be caused by neurosis. A mental disorder causes disturbances in the activity of the nervous system, which regulates intestinal motility.
The pathological condition affects those who often overeat, eat irrationally and abuse products containing caffeine.
Irritable bowel syndrome can be recognized by the following symptoms:
- it causes nausea, flatulence, heartburn, belching, pain and discomfort in the abdomen;
- the patient has an unpleasant taste in the mouth;
- a person loses appetite;
- periods of severe diarrhea (stool more than 3 times a day) are replaced by prolonged constipation (stool less than 3 times a week);
- alternation of diarrhea and constipation is often observed;
- the feces become either excessively dry, “sheep-like”, or watery, and mucus may appear in it;
- defecation is accompanied by straining and leaves a feeling of incomplete emptying;
- in addition to discomfort in the abdomen, the patient may experience headaches and a frequent urge to urinate (even with an empty bladder).
Also with irritable bowel syndrome, there is a feeling of a foreign object in the throat and dissatisfaction with breathing. The patient suffers from depression, panic attacks and phobias. His hands are constantly cold.
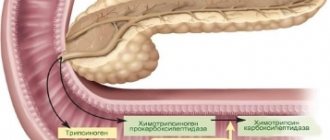
Chronic pancreatitis
Diarrhea and constipation often plague people suffering from chronic pancreatitis. Pancreatitis is a disease in which the pancreas becomes inflamed. As a result of the inflammatory reaction, the enzymes that the organ produces are not pushed into the duodenum, but remain in the gland and cause its destruction. The toxins released during this process have a negative effect on vital organs.
At the initial stage of the disease, the gallbladder and its ducts contract sluggishly. As a result, bile stagnates in the gallbladder and enters the duodenum in small quantities, insufficient to process food. Malfunctions of organs lead to constipation.
As the disease progresses, the stool becomes very loose. Patients with alcoholic pancreatitis suffer especially greatly from diarrhea. The chronic form of the disease is characterized by unstable stools, in which the patient experiences either diarrhea or constipation.
With diarrhea, feces have a mushy consistency and a characteristic greasy sheen. They are difficult to remove from the walls of the toilet.
The pathology is accompanied by nausea, bitterness in the mouth, flatulence and bloating. The patient suffers from dull pain and a feeling of heaviness in the right or left hypochondrium.
Nausea may trigger vomiting. In this case, bile can be detected in the vomit.
Drug therapy
The main task facing specialists is to eliminate the causes of diarrhea and constipation. In this case, a treatment regimen is selected for patients individually, which includes:
- taking antibacterial drugs;
- normalization of nutrition;
- regular eating;
- replenishment of fluid lost by the body;
- taking laxatives or antidiarrheal medications;
- eliminating factors that can lead to stress and nervous tension;
- taking sorbents, antispasmodics, anesthetics and enzymes;
- enemas, which are prescribed for constipation (long-term);
- for malignant neoplasms, surgical intervention is indicated, followed by the patient undergoing courses of chemotherapy, radiation therapy, etc.
This category of patients must adhere to a therapeutic diet during drug therapy:
- Products that may worsen the patient's condition are excluded.
- Experts recommend keeping a food diary in which you should record every meal you eat.
- The diet should include foods that contain large amounts of fiber, which can improve intestinal function. You should start eating such foods with small portions so as not to overload the stomach and prevent bloating and severe flatulence.
- Every day the patient should drink at least 6 glasses of purified water. It is recommended to drink liquid very often, but in small doses.
If constipation develops after diarrhea
- stop taking antidiarrheal drugs;
- the amount of fiber and liquid in the menu increases;
- start taking probiotics;
- the amount of sugar is limited;
- physical activity increases.
If diarrhea develops after constipation
- if the cause of constipation is a fecal impaction, then dry and hard stool is removed from the rectum (this can be done manually, through medications, or surgically);
- medications are taken that normalize the microflora in the intestines;
- the patient’s diet is adjusted, etc.
If disturbance of bowel movements is accompanied by nausea
- You should immediately contact a gastroenterologist who will conduct an examination and make an accurate diagnosis;
- patients are prescribed medications, for example, Ondasetron or Metoclopromide, which will eliminate nausea;
- drug treatment is carried out aimed at eliminating the cause of the condition;
- when intestinal colic occurs, antispasmodics are prescribed, which quickly eliminate discomfort;
- If a pregnant or lactating woman is faced with such a problem, then she is first of all switched to a healthy diet (it is forbidden to take laxatives, as it can provoke premature birth, and antidiarrheal medications will have a detrimental effect on the fetus).
Chronic enterocolitis
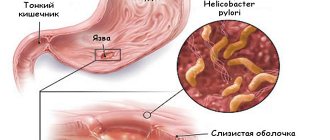
Diarrhea after constipation is observed in chronic enterocolitis. Enterocolitis is a disease of the gastrointestinal tract, which is accompanied by inflammation of the small and large intestines. The pathological process causes atrophy of the intestinal mucosa and disruption of its functioning.
If the inflammatory reaction has spread to a greater extent to the tissues of the colon, the patient suffers from constipation and diarrhea, which alternate. With this form of pathology, aching pain occurs in the abdomen on the right or left. Other symptoms of enterocolitis include: excess gas, flatulence, bloating and rumbling.
Sometimes diarrhea is so severe that the patient is forced to visit the toilet up to 7 times a day. Mucus and particles of undigested food are often found in the stool. During constipation, which causes severe pain, anal fissures may form. In this case, some blood remains on the surface of very hard feces.
When do you need a doctor?
Although diarrhea can most often be stopped with the help of available remedies, it is important to remember that most diseases that cause both symptoms at the same time are very serious. Therefore, in all cases, it is better to consult a specialist and undergo an examination.
We recommend: Causes and how to treat acute diarrhea?
Emergency treatment may be required for the following symptoms:
- sharp pain in the right side;
- lingering pain of moderate intensity;
- severe thirst and dry mouth;
- headache and feeling of shortness of breath;
- the appearance of cold sweat;
- frequent vomiting;
- blood in stool.
If one or more of the above symptoms occur, you should immediately consult a doctor and undergo a medical examination.
Intestinal dysbiosis
Constipation and diarrhea are characteristic symptoms of intestinal dysbiosis. The pathological condition occurs as a result of an imbalance in the intestinal microflora.
A healthy adult has about 50 trillion microorganisms in the intestines, some of which are beneficial microflora, and some are opportunistic, capable of causing diseases under certain conditions.
Microorganisms inhabiting the intestines perform many useful functions:
- dispose of undigested food residues;
- neutralize and remove toxins from the body;
- participate in the synthesis of vitamins;
- train the human immune system.
The number of opportunistic and pathogenic microorganisms is regulated by representatives of beneficial microflora. With dysbacteriosis, the number of beneficial microorganisms decreases. The remaining bacteria do not produce enough substances to inhibit the growth of opportunistic microflora.
Rapidly multiplying pathogens change the acid-base balance of the intestines, creating a favorable environment for the life of pathogens.
Excessive amounts of pathogens cause various ailments. The patient experiences abdominal pain, nausea, belching, unpleasant taste and bad breath. He is tormented by diarrhea and constipation, which appear in turn. Due to a decrease in the number of beneficial microorganisms, immune defense is weakened.
The patient becomes vulnerable to infectious diseases and suffers from allergic reactions to foods that he previously consumed without consequences.
Chronic cholecystitis
Constipation after diarrhea may be a sign of the development of chronic cholecystitis. Cholecystitis is an inflammation of the gallbladder, in which the processes of bile formation and bile excretion are disrupted. The chronic form of the disease in most cases develops after the formation of stones in the organ. Stones cause damage and inflammation to the walls of the gallbladder.
Main features:
- diarrhea in chronic cholecystitis often appears after eating fatty foods;
- when the gallbladder is inflamed, the process of digesting fatty foods is disrupted;
- During diarrhea, stool has a mushy consistency and a strong, foul odor.
Chronic cholecystitis is characterized by pain and a feeling of heaviness in the right hypochondrium or in the area above the navel. Unpleasant sensations appear within the next hour after eating. If the foods included fried, smoked and fatty foods, the pain will be more pronounced.
Then the patient begins to suffer from constipation.
An attack of cholecystitis can be triggered by hypothermia, shaking in transport, stress and excessive physical exertion.
Crohn's disease
Diarrhea and constipation may indicate the development of Crohn's disease. Crohn's disease is a chronic pathology of the gastrointestinal tract that is inflammatory in nature. It is characterized by the formation of granulomas (nodules).
Lesions can appear in any part of the digestive tract. Most often they are localized in the ileum and the initial part of the colon.
First, the patient experiences abdominal pain and diarrhea. The urge to defecate occurs up to 6 times a day, mainly at night. The affected person suffers from excessive sweating, vomiting, nausea and bloating. His body temperature can rise to 38-39°C. Sweating is especially severe at night.
The inflammatory process causes erosions on the intestinal walls. Feces moving along it injure the ulcerated mucous membrane. Therefore, mucus and blood are found in feces. Diarrhea alternates with intestinal obstruction, which results in severe constipation. As a result of fecal retention, the intestinal walls are even more damaged.
Since the disease is autoimmune in nature, the patient may show signs of arthritis (joint damage), stomatitis (inflammation of the oral mucosa), erythema nodosum (skin disease), episcleritis (damage to the whites of the eyes).
The disease is characterized by alternating symptoms. After periods of exacerbation, remission occurs, during which the signs of pathology decrease or completely disappear.
Criteria for constipation and diarrhea
First of all, you need to establish the concept of what is normal feces and the process of defecation. And if changes appear, then you need to figure out whether it is diarrhea or constipation. Normally, a person has an act of defecation once a day, but twice a day, once every two to three days without the occurrence of unpleasant symptoms, is also not a pathology.
Normal feces should be shaped, resemble a sausage, and leave the intestines painlessly without damaging its walls. Mucus can be observed in the stool in small quantities, but there should be no admixtures of blood and pus.
If these criteria change, then there is a possibility of constipation or diarrhea in the person. Let's find out what their criteria are.
| Constipation | Diarrhea | |
| Frequency of bowel movements | The act of defecation occurs rarely, once every three days or even once a week, there is a feeling of incomplete bowel movement, a feeling of incompleteness of the process. | Feces are passed three to ten times a day; the feces must be liquid, otherwise it is rather a peculiar form of constipation. |
| Stool consistency | Constipated stool is hard, may have the form of balls, is dry, does not come out of the anus well and can even injure it. | Diarrhea is loose, sometimes watery, with only mucus instead of stool itself. |
| Stool color | Most often, stool is dark brown in color, sometimes brown or black. In rare cases, discolored stool is observed, which indicates liver problems. | Yellow, green, light brown, sometimes transparent or whitish; if blood is released, the stool may turn red or pink. |
| Impurities | Blood, mucus, or pus may be present. When the intestines are damaged by worms, white stripes are observed - parts of the parasite. | Loose stools contain mucus in large quantities; it can even completely replace feces. There are blood impurities and purulent clots. |
| Smell | Normal, less often foul. | Fetid odor of feces, smacks of rottenness. |
| Additional criteria | With constipation, tenesmus may be observed - the urge to defecate, which does not end in success, the patient strains, but there are no results. Going to the toilet is accompanied by pain in the anus due to the appearance of cracks or tears in hard, dry feces. | A person constantly feels the need to defecate, since the sphincter is in a relaxed state, and the muscles of the anus have to be kept tense all the time. |
Diseases of the rectum
- Alternating diarrhea and constipation can be a sign of a serious disease - rectal cancer. Rectal cancer is a malignant tumor that develops from the cells lining the intestine. A characteristic feature of the disease is alternating constipation and diarrhea. When defecating, blood and mucus are released from the anus. The patient suffers from false urge to defecate and pain in the rectum.
- The appearance of constipation alternating with diarrhea may indicate the development of proctitis or paraproctitis. Proctitis is an inflammation of the rectal mucosa. The acute form of the disease appears suddenly. The patient experiences pain in the perineum, burning and a feeling of heaviness in the rectum. Body temperature rises to 38°C, weakness appears, and stool becomes unstable. If blood or blood clots come out of the rectum along with diarrhea, the process has acquired an ulcerative-necrotic character. With paraproctitis, purulent inflammation of the tissues surrounding the rectum is observed. The patient's body temperature rises above 38°C, severe pain appears in the lower abdomen and rectal area. There is a simultaneous disorder of stool and urination. The urge to defecate becomes frequent and painful.
Treatment
Treatment should be carried out under the supervision of a physician.
Treatment of constipation and diarrhea should be carried out at the etiotropic level, that is, the problem of these symptoms should be eliminated. To do this, the doctor may prescribe anthelmintic drugs, antibacterial agents, anti-inflammatory drugs, sedatives, and surgical intervention may be necessary.
It will be mandatory to establish a diet for the patient. Its main principle is fractionation and exclusion of all foods that irritate the intestinal mucosa (hot, spicy, peppery, fried, salty, fatty). Read about proper nutrition for constipation here.
For symptomatic treatment, antidiarrheal drugs to relieve diarrhea or laxatives for constipation may be prescribed.
An important stage of treatment is to establish a favorable psycho-emotional background for the patient. Establishing a daily routine, moderate exercise, both physical and mental, walks in the fresh air, and proper nutrition will help the patient feel better in the very near future.
Interesting video:
Helminthiasis
The appearance of unstable stool in an adult may be a sign of helminthic infestation. Parasites that inhabit the intestines release large amounts of toxic substances that poison the body.
Toxins cause inflammation and organ dysfunction. If there are a lot of helminths, they can completely block the intestinal lumen, causing constipation. Some types of helminths produce substances that cause diarrhea. When the numbers of these parasites are high, they can cause acute diarrhea following constipation.
If blockage of the intestinal lumen occurs periodically, in this situation there will be an alternation of diarrhea and constipation. The situation is aggravated by intoxication, which negatively affects intestinal function. It can provoke various diseases of the digestive system. They can also cause loose stools.