Terminology
Achalasia cardia is a disease of neuromuscular etiology and belongs to the chronic form. The disease is characterized by the absence or partial opening of the cardia when swallowing food. Against this background, the patency of the esophagus is disrupted, and chaotic contraction of the smooth muscles of almost all parts of the esophagus develops.
The cardia is a valve, or, in other words, the sphincter of the esophagus. The location of this organ is on the border between the esophagus and the stomach. The main purpose of the sphincter is to regulate food and feces as they move between parts of the body.
If the functioning of the valve is disrupted, then this pathology is called cardia insufficiency, or reflux.
Development mechanism
When the disease occurs, the lower esophageal sphincter stops relaxing during meals. If pressure on the inferior valve increases, the valve narrows further and the esophagus re-expands. As a result, undigested food accumulates.
Most often, the disease develops against the background of pathological changes in the nerve cells located between the walls of the esophagus and the muscle layers. The development of malignant neoplasms and diabetes mellitus can also cause the disease. A possible cause may be dystrophic changes in both muscle fibers and the plexuses of the esophagus, or Chagas syndrome after bedbug bites.
The pathology of achalasia cardia develops quite slowly. The diagnosis can only be made by X-ray examination or endoscopy.
Causes
Gastric cardia insufficiency can occur in any person and at any age. And most often it is not even possible to establish the exact cause of the pathology. And some factors that lead to illness cannot be eliminated from your life. However, there is a certain list of factors that most often lead to achalasia cardia:
- alcohol and tobacco abuse;
- food with a lot of salt;
- excess weight, especially against the backdrop of a sedentary lifestyle;
- irregular meals, snacks before bedtime and “heavy” foods;
- some medicines;
- nervous shocks;
- very rarely the disease can develop during pregnancy.
Diagnosis and treatment
If there is a problem with the sphincter, the patient can also be examined using MRI.
Open gastric valves can be detected using laboratory and instrumental studies, as well as by the presence of complaints in the patient characteristic of this disease. More often, radiography is used with preliminary administration of a contrast agent, which helps to visualize the mucous membrane of the stomach and esophagus. Fibrogastroscopy, determination of the pH level in the esophagus and a methylene blue test are also used. Magnetic resonance imaging is performed as an additional method. The patient is recommended to undergo a general blood and urine test, as well as culture a scraping from the stomach wall for the presence of Helicobacter pylori.
The initial degree of insufficiency of the valve between the stomach and esophagus can be treated by normalizing the diet and eliminating factors that negatively affect its condition. It is necessary not to overeat, eliminate irritating foods from the diet, cure chronic cough and constipation, and eliminate physical activity. It is recommended to bend less, as well as limit the consumption of alcoholic beverages and not smoke. To get rid of symptoms, temporary use of antacid drugs is prescribed, which neutralize the hydrochloric acid that has entered the esophagus. The following means are most often used:
- "Gaviscon";
- "Almagel";
- "Smecta";
- "Maalox."
To reduce the secretion of hydrochloric acid, Omeprazole is used, and to restore motility, Cerucal or Metaclopramide is used. If conservative measures are ineffective, surgery is recommended. It should be done in case of severe cardia insufficiency. The actions of surgeons during its implementation are aimed at ensuring that the sphincter can independently close and open the hole. To do this, the muscles are tightened and possible hernial protrusions are sutured.
Stages
Today, there are several stages of pathology development:
- Stage 1. Temporary decrease in sphincter tone, no expansion of the lumen yet.
- Stage 2. The condition is almost the same as at stage 1, but a mild degree of dilatation is gradually developing.
- Stage 3. At this stage of the disease, a stable expansion of the esophagus is already observed with simultaneous suprawall narrowing of the lower part of the esophagus. Scar changes form.
- Stage 4. Achalasia of the cardia at this stage progresses, complicated by fibrous mediastinitis, esophagitis or periesophagitis.
Diagnostics
Some of the previously listed symptoms accompany other diseases (stomach ulcer, gastritis, etc.), and various factors act as catalysts for reducing the tone of the valve muscles. Therefore, it is important to correctly determine the nature and causes of the ailment. The following types of research are used for this:
- X-ray;
- gastrofibroscopy;
- pH-metry of the esophagus, esophagoscopy, methylene blue tests.
X-ray using barium sulfate contrast determines the parameters of reflux, the presence of esophagitis or esophageal ulcers. If the results of fluoroscopy are unclear, it is followed by esophagoscopy, which makes it possible to examine the esophageal mucosa and the density of muscle closure.
Return to contents
Individual signs
If gastric cardia insufficiency is diagnosed, doctors distinguish several syndromes:
- Dysphagia syndrome. Clinical manifestations in this case are as follows: a feeling as if there is a “lump” in the chest;
- hard to swallow;
- The patient constantly chokes while eating.
It is easier for the patient to eat solid than liquid food. This is due to the fact that solid foods put a lot of pressure on the pyloric sphincter and promote its opening. Simply put, there is a violation of the passage of food. These symptoms are very important for a correct diagnosis; for example, in the presence of cancer or stenosis, the clinical picture is the opposite, and it is difficult for the patient to eat solid food.
If the cardiac sphincter loses its functionality, then in addition to the syndromes described above, the patient also experiences other symptoms:
- unpleasant odor from the mouth due to changes in the diameter of the valve and the constant retention of food particles in the esophagus. Over time, this can cause erosions and ulcers on the mucous membrane;
- heartburn, the patient feels that the pain is burning and moves from bottom to top;
- some patients even feel how food moves through a valve that does not close, leaving behind a sour taste;
- belching with a sour taste;
- excessive salivation;
- hoarseness in the throat;
- problems with teeth and gums, caries;
- increased heart rate.
This pathology is a progressive condition, so exhaustion and deterioration are increasing.
Problems with the pyloric sphincter
The pyloric sphincter regulates the flow of contents from the stomach into the duodenum of the small intestine. Like the lower esophageal sphincter (LES), it is composed of a circular muscle. It works in conjunction with the pyloric muscles, which push a mixture of food and liquid (gastric chyme) out of the stomach. Larger food particles cannot pass until they are broken down by the stomach.
Signs and symptoms include:
- Regurgitation, sometimes vomiting
- Feeling bloated
- Pain in the upper left and middle upper corner of the abdomen
- Heartburn or chest pain (sometimes)
- Diarrhea (sometimes)
Discussed below are just some of the most likely conditions that arise from problems with the pyloric sphincter.
Gastroparesis
Gastroparesis is a condition in which the nerves that control the abdominal muscles can become diseased or damaged. This results in delayed gastric emptying. There is no physical obstruction like a tumor. Instead, the pyloric sphincter may not open properly, and the stomach does not crush or expel food properly. Some of the causes are diabetes-related nerve damage, certain medications, and nerve damage from surgery.
Pyloric stenosis is a narrowing of the end of the stomach due to thickening of the muscles in this area
Pyloric stenosis
Pyloric stenosis is a narrowing of the end of the stomach due to thickening of the muscles in this area. It occurs in infants and may be present from birth. The growth of the muscles that make up the sphincter may not be accompanied by the development of proper nervous nutrition. As a result, some of these muscle fibers may not be controlled by the nervous system and this may affect the function of the sphincter.
Gastric shunt syndrome
Dumping syndrome is when the outflow of stomach contents cannot be controlled . This is mainly due to gastric surgery and gastric bypass procedures in particular. These procedures compromise the ability of the pyloric sphincter to control blood flow. This can also occur if the gastric nerve is damaged. Stomach contents quickly enter the small intestine before they can be properly digested.
Diagnosis methods
The main goal of diagnosis is not only to confirm or refute cardiac spasm, but also to exclude the presence of cancer in the stomach.
As a rule, laboratory tests do not provide any information at all, which is why they are used to determine concomitant pathology.
To determine how the upper and lower esophageal sphincters work, first of all, X-ray examination is used. Diagnosis is carried out with a barium element, which is injected into the stomach on an empty stomach to determine whether the lower valve is closed, which is typical for this type of pathology. The shape of the esophagus may take on something similar to a "bird's beak". The lower esophageal sphincter is usually unchanged in size, and fluid accumulation can be seen above it. At an advanced stage, the esophagus takes on an S-shape.
To clarify the diagnosis of esophageal achalasia and identify the degree of damage to the mucous membrane, and to refute or confirm cancer, esophagoscopy is used. This study is also a preparatory stage in preparation for surgery.
Causes of deficiency
Obesity can cause illness.
There are two groups of reasons, which are defined as organic and functional. The former are not associated with anatomical defects of the body and occur due to hiatal hernias or postoperative complications. Due to functional disorders, the cardiac sphincter does not close tightly and works in the opposite direction. He is hampered by pressure in the stomach cavity or intra-abdominal pressure, pyloric spasm. The valve muscles themselves lose tone, become weak and unclench. These ailments are preceded by the following regime violations:
- binge eating;
- eating food immediately before bedtime;
- obesity;
- passive lifestyle;
- constipation;
- excessive physical activity.
The causes of weak valve muscles include previous surgeries, pregnancy and chronic stomach diseases. Some foods and habits are harmful to the normal tone of the sphincter muscles:
- tomatoes;
- chocolate;
- coffee;
- fatty foods;
- smoking;
- alcohol.
Treatment
To reduce the severity of symptoms and eliminate any obstacles that may occur during the passage of food, 3 treatment methods are used:
- treatment with pharmaceuticals;
- non-drug therapy;
- surgical intervention.
Conservative
The main criterion for the effectiveness of drug treatment is the elimination of symptoms. To determine the effect experimentally, an X-ray examination is carried out with parallel administration of barium. If barium suspensions pass normally through the esophagus, then the treatment has helped.
The following are used in therapy:
- nitrates and calcium channel blockers, which reduce lower esophageal sphincter pressure;
- sedatives.
Psychotherapy is usually recommended to patients along with medications.
Non-drug and surgical
The effect of such treatment is possible mainly in the first stage of the disease. In this case, diet therapy is used, which requires eating in small portions, chewing food thoroughly. After a meal, be sure to drink water, which should wash away food debris from the esophagus. Food should be cooked gently and be neutral in temperature.
Pneumatic cardiodilation for esophageal achalasia consists of dilation of the inferior valve while simultaneously delivering air or fluid under high pressure. In practice, it looks like this: a balloon is inserted into the esophagus under fluoroscopic control. Once the balloon reaches the diaphragm, it is inflated. The treatment method is effective in 75% of cases, but there is a high risk of a side effect in the form of GERD.
Endoscopic cardiodilation is recommended for significant curvature of the esophagus. However, the technique also has a side effect - gastric perforation, which occurs in 5% of cases.
If the patient is not recommended for expansion of the esophageal valve, surgery, or the patient is elderly, then chemical denervation is performed. The effect is achieved in approximately 80% of cases and can last up to 12 months. The essence of the technique is that ethanolamine oleate or botulinum toxin is injected into the esophageal sphincter using an endoscopic needle.
Cardiomyatomy is used if previous procedures to widen the valve have not helped. But there is a huge risk that reflux or strictures will appear - this happens in 15% of cases. The essence of the technique is that after the introduction of anesthesia, local or general, a gradual expansion of the passage is carried out with cylinders of different diameters. The procedure is short-term, no more than 2 minutes. Between procedures (on average 5-6 will be required) a minimum of 4 days should pass.
The pathology of gastric cardia insufficiency can be treated using partial fundoplication. The procedure is also recommended for cicatricial changes on the walls of the esophagus. Treatment consists of cutting the membrane near the junction from the stomach to the esophagus. After cutting, the edges of the incision are sutured to the fundus of the stomach. The operation requires a recovery period of about 14 days, which will most likely have to be spent in the hospital, but in any case without going to work.
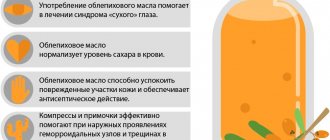
Good results can be achieved by using natural remedies. You can prepare a decoction of anise and fennel, which perfectly relieve inflammatory processes occurring on the mucous membrane. To get rid of heartburn and pain, you can use raspberry leaves or make chamomile or mint tea. However, it should be remembered that before using folk remedies, it is better to consult a doctor so that he can help you select doses taking into account damage to the mucous membrane.
If none of the recommended and carried out methods produces results, then an operation is performed to remove the esophagus.
Therapy
Therapeutic instructions
Before starting treatment, consult a specialist.
The following points must be followed so that the cardia of the stomach works normally and begins to close tightly:
- Correct diagnosis of the causes by a doctor and their subsequent elimination (this applies to pathologies leading to sphincter dysfunction).
- Eat food standing or sitting, keeping your back straight.
- Maintain a gap of 2-3 hours between your last meal and bedtime.
- Elevate your head while you sleep.
- Eliminate from your diet too spicy, fatty, cold or hot, pickled foods.
- Consume plenty of fiber daily and include daily entrees in your diet.
- Switch to smaller meals, do not overeat, especially be careful not to overeat before bed.
- Try to reduce intra-abdominal pressure by reducing the volume of fatty tissue if you are overweight.
- Reduce your consumption of foods that are dangerous to the gastric valve (strong coffee, tomatoes, chocolate, etc.).
- Quit smoking and limit your consumption of alcoholic beverages.
- Try to bend over less.
- Do not lie down after eating so as not to provoke heartburn and aggravate the condition of the esophagus.
- Wear comfortable clothes that are not tight on your body.
- Adjust your physical activity, try to work without significant effort. Walking in the fresh air is especially beneficial.
- Undergo periodic examinations with a gastroenterologist and complete the course of treatment prescribed by him.
- Do not experiment with medications to avoid complications.
Drug treatment
Prokinetics are used as effective treatment, for example: Cerucal, Metoclopramide, Reglan, Domperidone. They increase the activity of the cardiac sphincter, taken before meals up to 4 times a day. Along with prokinetics, medications are prescribed that suppress reflux (propulsid) and antacids that suppress heartburn (“Gaviscon”, “Almagel”, “Smecta”, “Maalox”, “Gastal”, “Phosphalugel”).
Treatment is supported by omeprazole to restore the walls of the esophagus, antiemetics and painkillers. Sometimes it is necessary to use antiprotozoal drugs and antibiotics.
ethnoscience
Dill seeds will help relieve inflammation.
There are several of the most effective folk treatments that do not allow the valve to open, working to eliminate the problem if the valve is open or weak:
- Pre-prepared sweet water (drink in the morning), chamomile, mint or raspberry tea, chewing raspberry leaves, cabbage or potato juice help with heartburn.
- Dandelions and sugar are laid out in even layers on top of each other and ground until smooth. The resulting syrup is diluted in a teaspoon in half a glass of water and drunk every day.
- Decoctions of anise, fennel or dill seeds relieve inflammation of the mucous membranes.
- A tincture of caraway seeds, which is made at the rate of one teaspoon per glass of boiled water, relieves cramps.
It should be borne in mind that any remedy is good in moderation and should not be harmful. Therefore, be sure to consult with your doctor, who should confirm that the decoction or infusion is suitable for you.
Diet
Food should be gentle and not irritate the esophageal mucosa.
When the lower esophageal sphincter stops closing normally, it is important what to eat, how and at what time. First of all, you need to eat at the same time, drink half a glass of water 10-15 minutes before meals. The intervals between meals when the valves are open should not exceed 4 hours. Marinades, pickles, hot or cold food and drinks, alcohol damage the mucous membrane of the esophagus, so they should be completely avoided. The following products have a beneficial effect on the digestive system and when the valve is open:
- steamed food;
- pureed soups;
- light porridges;
- high-protein foods with low fat content (peas, beef, soy, chicken, low-fat cottage cheese).
Prevention
The best prevention for the appearance of an open valve is a healthy lifestyle and proper nutrition. Periodic examinations by a gastroenterologist are necessary. To avoid digestive problems, the following points are mandatory for a person’s entire life:
- Moderate physical activity and special attention to abdominal and back exercises.
- Good sleep, rest and recovery from stress.
- Timely response to heartburn (refusal of certain foods, bad habits and consultation with a doctor).
- Watch your excess weight.
- Drink half a glass of water before meals.
Methods for strengthening the lower valve
As a rule, patients are offered all treatment methods. In our country, alternative methods of strengthening the sphincter are not widely used, although world practice proves their high effectiveness.
There are breathing exercises for gastric cardia insufficiency that allow you to get rid of symptoms in the first stages of achalasia. Therapeutic exercises must be carried out on an empty stomach, using abdominal and chest breathing.
Restoration of the sphincter can be carried out with the help of physical therapy. Treatment is best carried out against the background of conservative therapy, even in the acute period. Electrophoresis and DDT are usually used. Naturally, it won’t work directly on the valve, but the phrenic nerve is stimulated with current. The procedures are carried out about 10 times, every other day.
The electrophoresis method is similar, but medications are applied to the cuff with electrodes. The therapy allows for improved blood supply and healing occurs much faster. Some patients note a slight decrease in pain.
Forecast
If the disease is at stage 1, then the prognosis is quite favorable. Especially if the patient strictly follows the doctor’s recommendations. Physiotherapy and breathing exercises will help restore the sphincter.
The second and third stages are no longer the best prognosis for the patient’s recovery. Most often it is not possible to do without surgical intervention. Patients at this stage after treatment will have to be regularly examined to avoid exacerbations.
If left untreated, esophageal achalasia leads to carcinoma in approximately 5% of cases, and aspiration pneumonia occurs in 10% of cases. Patients will have to give up irregular meals and heavy physical work.