Feeding rules
If you have symptoms of the disease, follow the following nutritional principles:
- The pancreas is given maximum rest during exacerbations. To do this, food is crushed and offered only warm.
- “Irritants” are excluded from the diet: tomatoes, citrus fruits, chocolate, etc.
- It is important for a child’s body to maintain the average daily energy value of food at a level corresponding to age standards.
Prohibited foods cannot be added to the menu even during stable remission and absence of pain in the pancreas. Otherwise - weakness. You can provoke a new exacerbation. As a result, you will have to put your child back on a strict diet. In this case, pity for your beloved child asking for the treasured delicacy risks turning into a new wave of the disease.
Try to avoid situations that provoke diet failure. As a child grows up, he will have to attend various holidays. Not letting him in is not an option. This can adversely affect development and create psychological problems.
Try to warn in advance the adults with whom the child comes into contact and the teachers in the kindergarten about his problems with the pancreas and prohibited foods.
Instill a serious attitude towards your health and the baby himself. After all, the course of the disease and the success of treatment will depend on it.
The main characteristics of nutrition for pancreatitis:
- Ensuring maximum functional rest of the pancreas during acute manifestations of the disease. This is achieved by observing the principles of mechanical (grinding food), thermal (eating warm food) and chemical (excluding irritants) sparing.
- For a child, it is extremely important to maintain the nutritional and energy value of the diet: in no case should you limit the daily caloric intake, the content of proteins, carbohydrates, fats, vitamins, micro- and macroelements! You just need to use suitable products as sources of these nutritional components.
- Even during persistent remission, prohibited products continue to remain prohibited. Any experiments can end very badly - a new severe exacerbation, hospitalization, parenteral nutrition and a return to the strictest diet. Dear parents, remember that your pity for your child, when you are unable to refuse his requests for a piece of delicious cake, ice cream, a sip of lemonade, etc., will always turn against your child!
Different course of the disease
Chronic and acute pancreatitis occurs rarely in children. But reactive is well known to many mothers. Depending on the symptoms, nutritional recommendations for your child will vary.
- For chronic pancreatitis, a strict diet and a careful, gradual transition to a variety of foods on the menu are important. In this case, dietary restrictions are established for a long period. Many foods will have to be abandoned forever, otherwise the symptoms of the disease may return.
- Acute pancreatitis is treated through a strict monthly diet. As the child recovers, the range of products expands. But the strict dietary principles of table No. 5, recommended for this disease, will have to be followed for another five years, even if no symptoms are observed. But even after the established period, excesses in the child’s diet are undesirable, since they can cause a second attack.
- For reactive pancreatitis, the diet lasts one or two weeks. After this, it is necessary to provide the child with age-appropriate nutrition. Otherwise, you won’t have long to wait for a new malfunction in the pancreas.
Features of a child’s diet in different forms of the disease
In childhood, based on statistical data, a disease such as pancreatitis, which occurs in chronic or acute form, rarely occurs. Mostly children are susceptible to a reactive type of illness, which in medical terminology is called dyspancreatism. With this type of pathological condition, the children's pancreas, which is responsible for the production of digestive enzymes, ceases to function normally due to somatic disorders or frequent dietary disorders.
In order to help your child cope with the disease, it is necessary to correctly adjust the diet, including in the daily menu only those foods that the doctor allows.
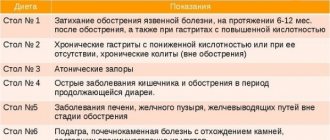
All restrictions in the children's diet necessary for inflammation of the pancreas are directly dependent on the type of disease developing in a small child. To learn more about the nuances of the diet prescribed for children, you should look at the table below. It indicates the main characteristics of the children's dietary menu, which are recommended by the famous TV presenter, Dr. Komarovsky.
Principles of the dietary table for pancreatitis in a child
Form of the disease Nutrition principles Acute pancreatitis From the moment the disease is diagnosed, diet No. 5 is prescribed, which is followed for at least a month. The first week she is very strict, and then as the baby’s health improves, the table begins to gradually expand. But the child must follow the principles of the dietary diet for at least five years, even if there are no negative symptoms. Gross errors in the menu and in the future are undesirable. Reactive type of disease The diet correction recommended for the baby by a gastroenterologist must be followed for at least 14 days. After this period, there will be no strict restrictions in the diet, but the doctor will advise you to feed the child according to his age, including only benign foods in the menu that do not cause damage to the mucous membrane. Chronic process After the exacerbation ends, the strict diet will be canceled and a less gentle diet option will be prescribed. But the diet will remain selective (many products will be completely prohibited) and it will be necessary to adhere to it for life.
Each stage of the disease requires the baby to adhere to a certain diet with strict adherence to all doctor’s recommendations. But even despite the existing bans on certain types of foods due to this disease and strict requirements for food management, parents can make their child’s daily menu not only nutritious, but also tasty. By showing a little imagination when preparing a dish from a meager list of ingredients, you can please even the most capricious and picky eater of a child.
What will you have to forget?
Products strictly contraindicated:
- all types of smoked meats;
- pickled (with added acid) vegetables;
- semi-finished products;
- fast foods;
- spicy seasonings.
For reactive pancreatitis, it is occasionally permissible to include in the menu:
- high-calorie dairy products: cream, condensed milk, ice cream;
- lemonade and mineral water;
- pickles and fermented products;
- broths;
- spicy seasonings;
- fruits and juices;
- any types of vegetables;
- millet cereals and pearl barley;
- meat and fish of any kind;
- baked products, including those containing cream fillings;
- chocolate products.
The listed products should not be given to the child in large quantities. After a long diet, it is advisable to introduce them into the children's menu gradually and in small portions.
What you can and cannot eat
To provide gentle, complete nutrition, the child’s diet should include chopped, steamed, baked or boiled foods.
Meat (beef, turkey, rabbit, chicken) and white fish (cod, hake, pike perch) of low-fat varieties are required.
It is better to grind cereals (oatmeal, buckwheat, rice) in a coffee grinder or puree them cooked. Introduce eggs into the diet with caution - first the white, then the yolk in parts. Boil eggs soft-boiled. Low-fat kefir, milk and cottage cheese are preferred. Bake or boil vegetables (beets, carrots, potatoes) in their jackets. Baked apples, pears, and pumpkin are useful.
The list of prohibited foods is extensive, but there is nothing on it that would be vital for a growing body. This is spicy, fatty, fried food.
You cannot include borscht, rassolnik, mushroom soup, liver and kidney dishes on the menu. You will have to exclude fresh bread, pastry, candy, chocolate, ice cream, sparkling water, coffee, cocoa, canned food, and sausages.
It is not recommended to cook porridge from barley, corn and pearl barley.
Fresh berries, fruits and vegetables irritate the digestive tract, which can also trigger an attack.
How to eat?
Photo: Depositphotos.com. Author: Wavebreakmedia.
In case of acute symptoms of pancreatitis, children are subject to mandatory hospitalization in a hospital.
- In the first days, feeding is excluded, only parenteral (intravenous) nutrition is relevant through the introduction of solutions necessary for the growing body.
- On the second day of hospitalization and in the absence of vomiting, it is allowed to drink warm boiled water in very small sips. It is recommended to drink no more than one glass per day of still mineral water or a weak rosehip decoction.
- On the third day, when health improves, pureed porridge in water with a small amount of freshly prepared puree - cauliflower, potato or zucchini - is added to the child's diet. Natural jelly made with apple juice and dried fruit compote are useful.
Gradually, vegetarian soups, steamed egg white omelettes, and cutlets made from lean, several times minced meat appear on the children's menu.
Authorized Products
A diet for an enlarged pancreas in a child includes the following foods in the diet:
- Vegetable broths/soups based on vegetable broths, into which thoroughly pureed vegetables are added and well-cooked/mashed grains are added. Soups can be seasoned with butter, sour cream, butter; frying is prohibited.
- Lean meat (beef, rabbit, veal, chicken, turkey) in the form of chopped products (meatballs, cutlets, soufflés, quenelles, meatballs), steamed. Boiled poultry/rabbit can be eaten in pieces.
- Porridge (semolina, oatmeal, buckwheat), rice, cooked in water with the addition of milk and well ground to a semi-viscous consistency.
- Vegetables (boiled/grated) until pureed - zucchini, carrots, potatoes, pumpkin, cauliflower, beets, green peas, peeled tomatoes and grated cucumbers. Later, grated pumpkin/raw carrots are allowed.
- Low-fat fish (pike, pollock, pike perch, hake, blue whiting, cod, carp, perch). Used in the form of cutlets, steamed/boiled in pieces.
- Low-fat dairy/fermented milk products (cottage cheese, mild grated cheese, kefir, fermented baked milk).
- Milk/sour cream - as an additive to dishes.
- Dried wheat bread, savory biscuits (biscuits).
- Steamed protein omelettes (1 egg per day).
- Sauces based on vegetable broth (do not fry flour) with the addition of sour cream/milk.
- Baked sweet apples, pureed dried fruits. Boiled, mousses, jelly, sweet fruit pastilles. Limited - pureed raw fruits/berries.
- Fats, first carefully introduce butter, and later refined sunflower oil.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| broccoli | 3,0 | 0,4 | 5,2 | 28 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| apples | 0,4 | 0,4 | 9,8 | 47 |
Nuts and dried fruits | ||||
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| prunes | 2,3 | 0,7 | 57,5 | 231 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| rice | 6,7 | 0,7 | 78,9 | 344 |
Bakery products | ||||
| wheat bread | 8,1 | 1,0 | 48,8 | 242 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| fruit and berry marmalade | 0,4 | 0,0 | 76,6 | 293 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
Dairy | ||||
| kefir 1.5% | 3,3 | 1,5 | 3,6 | 41 |
| curdled milk 1% | 3,0 | 1,0 | 4,1 | 40 |
| acidophilus 1% | 3,0 | 1,0 | 4,0 | 40 |
Cheeses and cottage cheese | ||||
| cottage cheese 1% | 16,3 | 1,0 | 1,3 | 79 |
| cottage cheese 1.8% (low-fat) | 18,0 | 1,8 | 3,3 | 101 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken breast | 29,8 | 1,8 | 0,5 | 137 |
| boiled turkey fillet | 25,0 | 1,0 | — | 130 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| flounder | 16,5 | 1,8 | 0,0 | 83 |
| pollock | 15,9 | 0,9 | 0,0 | 72 |
| blue whiting | 16,1 | 0,9 | — | 72 |
| cod | 17,7 | 0,7 | — | 78 |
| hake | 16,6 | 2,2 | 0,0 | 86 |
| pike | 18,4 | 0,8 | — | 82 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
Non-alcoholic drinks | ||||
| water | 0,0 | 0,0 | 0,0 | — |
| mineral water | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| peach juice | 0,9 | 0,1 | 9,5 | 40 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||
Let's get better
Not earlier than the second week from the start of the fight against pancreatitis, the following is added to the diet:
- kefir;
- meat and fish meatballs, steamed cutlets and meatballs;
- skim cheese;
- vegetable casseroles;
- baked apples.
All dishes prepared for children should be chopped, without strong flavoring additives. A child can only eat them warm. With each subsequent day, the baby’s menu is subject to expansion. As a rule, by the end of the month the need for thorough grinding disappears. All food must undergo heat treatment: stewing, steaming or baking.
Now children can eat mild and low-fat cheese (for example, Adyghe), baked fish, chicken and other types of lean meat. Puddings, cottage cheese casseroles and pasta are added to the diet.
Among the drinks useful for pancreatitis, jelly remains relevant. Children are also given dried fruit compotes and weak tea. It is highly desirable to have fermented milk products on the menu: yoghurts, fermented baked milk, cottage cheese and kefir.
Food for a child should still not be salted or flavored with sugar.
Sample menu during the period of non-exacerbation of the disease
After the acute attack subsides, the child’s diet gradually expands. But at the same time, it is necessary to take into account that the baby’s daily menu should be compiled taking into account the basic nutritional rules that are recommended by nutritionists for this disease. And also we should not forget that the dishes should not contain those products that can lead to complications of the disease. When creating a menu for a child with pancreatitis, you can rely on the following list of allowed dishes:
- Breakfast . In the morning, it is best for your baby to prepare porridge, steam omelet or curd soufflé. You can also offer your child to eat a soft-boiled egg. Children will also like baked apples stuffed with rice during breakfast. Moreover, this fruit is doubly useful for diseases of the gastrointestinal tract - it contains large quantities of iron, which is necessary for the spleen and improves blood composition.
- Lunch . It is a snack between the first and second main meals. A good option here would be fruit puree from fruits approved by the gastroenterologist, crackers, biscuits and a cup of jelly.
- Dinner . A must-have dish is soup. It can be cereal, vegetable, fish or meat. But in the last two options, it is necessary to take into account that meat and fish must be of lean varieties. For the second course, kids enjoy steamed cutlets and meatballs in milk sauce with side dishes of cereals or pasta.
- Afternoon snack . A good option for this snack would be a glass of milk with dry cookies. You can also offer your baby to drink rosehip decoction, jelly, weakly brewed tea, or eat low-fat yogurt.
- Dinner . It should not be dense, so nutritionists recommend that children with pancreatitis eat vegetable stew, buckwheat cooked in water, a piece of boiled chicken or fish in the evening meal.
- Before going to bed , kefir is the best option; you just need to remember that it must be alive, that is, its shelf life cannot exceed 7 days.
The dishes listed above can be combined at your discretion and made up of different types of menus. This will make your baby's table varied and prevent him from losing interest in food.
A few simple tasty and healthy recipes
As already mentioned, children are always picky about food and can refuse any healthy food that they do not like. That is why gastroenterologists recommend approaching the preparation of a children's dietary menu very carefully and showing maximum imagination when preparing foods for a sick child. There are several original and tasty recipes that are completely safe for any gastrointestinal diseases. Most often they are advised to be included in the menu for children whose pancreas (pancreatitis) or gallbladder (cholecystitis) is inflamed:
Rice porridge with pumpkin
Peeled pumpkin (0.5 kg), cut into small pieces, is poured with water so that it lightly covers the healthy summer vegetable, and boiled until soft. Salt and sugar are added in minimal quantities, just to slightly flavor the taste. After the pumpkin becomes soft enough, add 7 tbsp. l. rice and continue to cook over low heat until done. After there is practically no water left in the porridge, pour a glass of boiling milk into it, close the lid, remove from the heat and leave for half an hour to heat.
Carrot soup with semolina
Any picky little one will love this soup and will firmly become part of the family menu even after the baby recovers. To prepare it, 250 grams of carrots are stewed. After the vegetable is ready, it is cooled and thoroughly chopped, and in another bowl at this time, 2 tbsp is boiled in half a liter of water-milk mixture. l. semolina. As soon as the semolina base is ready, add grated carrots and a small amount of sugar and salt. The fully assembled dish is kept on the fire for no more than 2 minutes.
Fish quenelles
The fish fillet is scrolled in a meat grinder with the smallest grid. To the resulting minced meat add white bread soaked in milk, an egg and a little salt. Dip the finished mixture into boiling water with a tablespoon and cook for 20 minutes.
Banana cake
All children have a sweet tooth, so mothers want to pamper them with something tasty. But since with pancreatitis it is forbidden to consume culinary masterpieces in the form of cakes and pastries, you should use a little imagination and prepare a delicacy from fruits allowed for this disease. Moreover, it is very simple. Gelatin is soaked in cold water, and after it swells, mixed with low-fat yogurt without preservatives and mashed banana. A layer of dry cookies is placed on the bottom of the mold, and a banana-yogurt mixture is placed on it. The hostess decides how many delicious layers to make. The finished semi-finished product is placed in the refrigerator for half an hour to harden, and then served.
Oatmeal jelly
Oatmeal jelly is also very useful for children with pancreatitis. Regular use of it will allow you to launch restoration processes in the pancreas, which will quickly improve the general condition of the baby.
The recipe for this dish is very simple. A handful of oatmeal is soaked overnight in half a liter of cold water. In the morning, the infusion is filtered, squeezed out and brought to a boil over low heat, with constant stirring. After boiling, the jelly is removed from the stove and left for an hour. But this healthy drink should only be taken slightly warm, since a hot or cold drink can cause significant harm to the digestive organs instead of benefiting it.
We are expanding our range
During remission of pancreatitis, as the symptoms disappear, the range of products included in the diet should be expanded. But do not do it thoughtlessly, so as not to harm the treatment.
There comes a time when you can put a piece of butter (no more than 5 g) into the porridge, and season the vegetable puree with sour cream or cream (no more than 5 g). You can add yesterday's white bread to the menu.
To sweeten your baby's drink, some nutritionists allow the use of sugar substitutes. But doing this on your own, without medical approval, is prohibited. Each new dish is introduced gradually, monitoring the reaction of the child’s body. At the first signs of pancreatic dysfunction (nausea, increased gas formation, abdominal pain), you should immediately exclude it from the diet.
Meals as part of a therapeutic diet should be divided: every 2-3 hours. Long periods of fasting are unacceptable!
Diet during remission of pancreatitis
As the child’s well-being improves, the range of acceptable foods and dishes expands. However, each new dish is introduced gradually, and at the slightest sign of disturbance in the functioning of the pancreas (nausea, abdominal pain, flatulence, diarrhea), it is immediately removed from the menu. The diet includes fresh juices, fruits (sweet apples and sweet citrus fruits, melon, pineapple), vegetables (cucumbers, tomatoes, carrots, herbs), young green peas, berries (apricots, plums, cherries, strawberries, raspberries, grapes, black currants ). But their quantity is strictly limited and they are not suitable for daily use. Occasionally you can eat white cabbage, eggplant, and young corn. The menu is still based on milk porridges, vegetarian soups, minced meat dishes, stewed or baked fish, skinless chicken and turkey, boiled and stewed vegetables, and fermented milk products. It is not advisable to use whole milk in food, but you can cook soups and porridges with it. Some sweets are allowed: jam, jams, honey, marshmallows, marmalade, sugar - but all in moderation. Meals should be small, frequent - every 3-4 hours. Long hungry breaks are unacceptable!
It is important to know when to stop
The children's menu should include fresh fruits, berries and vegetables, but for a child with pancreatitis their quantity must be limited. Let your fidget eat these foods not every day.
- Introduce white cabbage, eggplant and young corn with caution.
- An important part of the diet for children is milk porridge and soups. Whole milk is suitable for preparing these dishes, but not as an independent product in the diet of a sick child.
- Among the permitted sweets, jam and marshmallows without glaze should be noted, but not chocolate!
What do parents need to know?
In addition to following the rules for preparing and eating food for children with pancreatitis, there are some other nuances that parents should know in order to prevent accidental errors in the baby’s diet:
- Children of preschool age attend preschool institutions. In kindergartens, although exclusively dietary food is prepared, this food is not suitable for children with pancreatitis. Therefore, the mother should warn the teacher that the child has some dietary restrictions. You also need to give the baby’s medical record with the recommendations indicated in it to the nurse of the preschool institution.
- Sometimes, when children follow a gentle diet, a situation arises when children are invited to a birthday or holiday. It is under no circumstances recommended to skip such an event due to dietary restrictions, as this will negatively affect the social adaptation of a small child. In this case, in order to avoid dietary or psychological problems, you need to talk in advance with the parents of the inviting child about the diet prescribed by the doctor.
But gastroenterologists also recommend that mothers remember that new foods should be introduced into the diet of babies suffering from pancreatic problems with extreme caution. The initial portions are made tiny, not exceeding 5–10 grams, and if negative symptoms appear, they are immediately removed from the diet. But after some time, they try to introduce the removed product into the menu again. It is excluded completely only when the baby’s body shows a negative reaction for the second time.
Bibliography
- Baranov A.A. Problems of pediatric enterology at the present stage. Russian Gastroenterological Journal 1995 No. 1 pp. 7–11.
- Baranov A.A., Klimanskaya E.V., Rimarchuk G.V. Pediatric gastroenterology. M., 2002
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. In the book “Handbook of Dietetics”, edited by V.A. Tutelyan, M.A. Samsonova. - 3rd ed., M., Medicine. 2002 pp. 209–217.
- Plotnikova T.V. Recipes of dishes for children's institutions. Phoenix 2013
- Ilyin V.F., Therapeutic diets for pancreatitis and other diseases of the pancreas. M.: Vector, 2010.
- Zikeeva V.K. Therapeutic nutrition for acute and chronic pancreatitis. Handbook of Dietetics edited by V.A. Tutulyana, M.A. Samsonova. 3rd ed., M.: Medicine, 2002, pp. 209–217.
Food for children and adults
Babies have their own feeding habits. But if your baby is sick with pancreatitis, you will have to monitor his menu even more carefully.
- Fresh juices, berries (covered with rough skin and/or having small seeds), vegetables and citrus fruits should not be introduced into the diet of young children under 3 years of age. Even during the period of remission, all food is pureed or crushed in a blender, since babies are not inclined to thoroughly chew the pieces that fall into their mouths.
- For children over 3 years old, the matter is complicated by the need to attend kindergarten or school. The menu in these institutions is designed specifically for children, but is not entirely suitable for patients with pancreatitis. If there is no competent medical professional in the children's educational institution who understands the importance of the problem, make a list of harmful foods for your child yourself and give it to the teacher.
Features of the diet in children over 3 years old
After the age of 3, most children begin to attend kindergarten, and from the age of 7 - school. Although food in children's educational institutions is dietary, it does not correspond to the diet for pancreatitis. Make sure that when registering for school or kindergarten, your child’s record includes a diagnosis of pancreatitis, and the recommendations indicate the need for therapeutic nutrition. If there is no health worker in the kindergarten (school), make a detailed list of foods prohibited for your child and give it to the teacher (teacher). If possible, protect your child from situations that provoke him to fail in his diet. It is clear that it is impossible to prohibit him from contacts with peers; he will attend birthdays and other holidays, which involve eating food, and far from being dietary. If you cannot accompany your child to such events, inform the adults present there (parents of friends, teachers, etc.) about the ban on certain categories of products (cakes, lemonade, chips, etc.). Explain the seriousness of the disease to the child himself and try to instill in him the need to follow a diet: after all, the course of the disease will largely depend on the responsibility of the child himself and his ability to self-control.
Traditional medicine products
Traditional healers advise adding the following points to the traditional treatment of the pancreas:
- non-carbonated mineral water during the day in between meals;
- decoctions of licorice, flax and trifoliate violet;
- infusions of calendula and birch leaves;
- cabbage and carrot juices.
It is better to drink juices and infusions half an hour before meals.
Licorice syrup for children.
Folk remedies can be effective in treating pancreatitis in adults. As for the child, the validity of their use is questionable and must be discussed with the attending physician.
Oatmeal jelly can be considered almost the only relatively safe remedy for a baby.
General principles of nutrition
A diet for reactive pancreatitis in children allows you to relieve the gastrointestinal tract and reduce the load on the digestive organs. The basic principles of nutrition are to create a mechanical, chemical, temperature protective regime for the stomach. This principle is fundamental when creating any diet.
- Meals are fractional. A sick baby should be fed 5 times a day. The intervals between feedings should remain equal in time. The serving size is modest, allowing you to reduce the load on the diseased organ and reduce pain.
- The first weeks after the onset of an exacerbation, food is indicated in the form of purees or semi-liquid.
- It is recommended to serve dishes boiled or steamed, baked in the oven without crust.
- Food is offered slightly warm or at room temperature. Too hot or cold food will worsen the child’s condition.
- The diet is provided rich in protein. This is achieved by increasing the amount of fish, meat, and cottage cheese. Carbohydrates and fats are limited.
In the acute period of the disease, treatment is carried out according to the traditional principle - fasting, cold and rest. During the first 2-3 days, it is necessary to offer the child a minimum amount of food. Complete fasting is not recommended for young children.
The child is urgently hospitalized in serious condition. In a hospital setting, parenteral nutrition is prescribed through intravenous drips.
What needs to be completely excluded
Regardless of the stage and form of the disease, baby food does not include the following products:
- Smoked sausages and fish.
- Factory-made products with a large number of preservatives and flavor enhancers. The category also includes chips and other snacks loved by children.
- Hot and spicy seasonings.
- Fast food.
Acute course of the disease
If the course of pancreatitis in a child is acute, it is necessary to exclude the following foods:
- Ice cream.
- Condensed milk.
- Sweet highly carbonated drinks.
- Pickles and marinated dishes, sauerkraut.
- Canned foods and pates.
- Strong, rich broths made from fatty meats and fish.
- Sour varieties of fruits and berries and juices from them.
- Vegetables containing coarse fiber - cabbage, radish, eggplant, garlic.
- Porridge made from pearl barley or millet.
- Fatty meats - goose, duck, pork, lamb.
- Fatty varieties of sea and river fish.
- Confectionery and baked goods.
- Nuts.
- Chocolate and cocoa in any form.
After reactive pancreatitis has been relieved, it is allowed to introduce small doses of the listed products into the children’s diet, rarely and little by little. Vegetables and fruits are best served baked and peeled. It is preferable to feed the child with pureed or semi-liquid food.
Dish recipes
Steam and bake healthy and tasty dishes.
Potato dumpling soup
Boil the potatoes (200g) and chop them while hot in a blender. Knead the potato dough with egg white and a tablespoon of flour. Form into dumplings and place in boiling vegetable broth. Cook for 5-7 minutes.
Cauliflower soup
Boil peeled vegetables (cauliflower, carrots, potatoes) in salted water and chop with a blender. Serve the finished soup with croutons.
Mince chicken fillet (200g) twice. Add the egg whites beaten with a fork and two tablespoons of ground crackers to the minced meat, add a little salt. Steam for 30 minutes.
Boil the beets, peel and grate on a fine grater. Boil the washed broken rice and mix with beets and egg whites. Bake the formed cutlets for 20 minutes.
Rinse the dried apricots thoroughly and steam with boiling water for 15 minutes. Grind with a blender. Cook semolina porridge with milk, add dried apricots and whipped egg whites. Cook in a water bath. Place a large pan of water on the fire and place a cup of pudding in it. Cover with a lid and cook for 20-25 minutes.
source
What foods can you eat?
- Dried yesterday's bread and dry biscuits.
- Vegetarian soups with vegetables. In a state of remission, you can season the soup with a spoon of non-acidic sour cream or butter.
- Lean meat - rabbit, turkey, chicken, veal. The meat is best served as steamed minced meat.
- Lean, boneless fish or fish cutlets.
- Low-fat dairy products. It is acceptable to give your child non-acidic kefir or yogurt. It is enough to add sour cream to purees or soups.
- Steamed egg white omelettes.
- Well-cooked semi-liquid porridge with milk.
- Puree from boiled or baked vegetables and fruits.
You will have to follow the diet for a long time. If a child visits a child care facility, it is better to inform the staff about the need for dietary nutrition for the baby. You will need to warn relatives to avoid purchasing prohibited treats.
Following a diet for diseases of the pancreas is one of the most important components of successful treatment, which can significantly speed up the recovery process and achieve long-term remission of the disease.