Causes of paraproctitis
The cause of paraproctitis, like any other inflammation, is infection. Pathogens usually spread from the rectum.
At the junction of the intestine itself into the anal canal there are special folds - crypts, or anal columns. The anal glands open in them and produce a mucous secretion. It protects the intestinal wall from damage from feces, and also slows down the growth and reproduction of bacteria, which, for obvious reasons, are very abundant in the rectum.
Sometimes the lumen of one of these glands becomes clogged, and the stagnant secretion becomes a favorable environment for the proliferation of pathogenic microbes. A suppurating cyst is formed, from which inflammation spreads into the perirectal tissue, forming an abscess - purulent inflammation. This is the most common cause of paraproctitis.
Less commonly, the infection enters the perirectal tissue through the bloodstream from other inflamed organs (hematogenous spread) or after injuries to the anal area and perineum.
Conditions that reduce general and local protective reactions of the body contribute to the development of infection:
- concomitant acute or chronic infection;
- hypovitaminosis, malnutrition;
- diabetes;
- Crohn's disease;
- rectal fissures, hemorrhoids;
- constipation
When are medications indicated?
Antibiotic drugs are indicated for patients with paraproctitis if there are corresponding symptoms or concomitant pathologies requiring anti-inflammatory therapy.
For parapraktitis, in some cases, antibiotics are indicated
Indications for taking antibiotics:
We have selected useful articles on the topic
Victory over excess weight. Keto Slim drug
05.02.2021
How to use Gepatrombin G suppositories according to the instructions
20.05.2019
The use of activated carbon for colic
20.05.2019
- Lack of access to a doctor. In a situation where the patient cannot temporarily visit a medical facility, medications can help slow down the process and reduce the intensity of symptoms.
- Contraindications for surgery. Surgical intervention is not performed if the patient has serious concomitant chronic diseases that are in the acute stage.
- Postoperative period. After surgery, dressings are regularly performed, requiring treatment of the wound with an antibacterial external agent to prevent infection.
- Inflammatory process after surgery. In cases where inflammation inside the rectum persists after surgery, antibiotics help suppress it.
If the fever does not subside, you also need to take antibiotics
- Long-term maintenance of elevated body temperature. When the temperature rises above 38 degrees for several days, the infection in the body may progress, which is stopped by antibacterial agents.
- Concomitant development of a fistula with subsequent removal. When performing two operations together, it is advisable to take antibiotics, since the risk of wound infection is much higher.
The main purpose of antibiotic therapy for paraproctitis is to prevent infection of the body. For this reason, drugs of this group are used more often in the postoperative period for the purpose of prevention.
Classification of paraproctitis
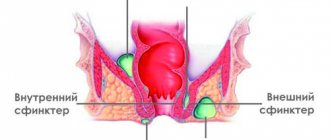
The rectum is quite complex.
According to the nature of the inflammation, paraproctitis can be acute or chronic. In chronic paraproctitis, fistulous tracts are formed from the area of purulent inflammation, through which pus is constantly released onto the surface of the skin or into the lumen of the anal canal.
According to the localization of purulent leakage, paraproctitis is divided into:
- subcutaneous;
- submucosal;
- intermuscular;
- ischiorectal (ischiorectal);
- pelvic-rectal:
- pelviorectal,
- retrorectal,
- horseshoe-shaped.
According to the location of the purulent fistula:
- intrasphincteric;
- transsphincteric;
- extrasphincteric.
The surgical tactics and the likelihood of complications depend on the location of the lesion and the nature of the purulent tract.
According to the nature of the pathogen:
- aerobic;
- anaerobic:
- clostridial,
- non-clostridial.
This division is necessary for choosing a treatment method. Anaerobes - bacteria that exist without oxygen - cause more severe damage. Particularly dangerous are pathogenic anaerobes of the genus Clostridia, different types of which cause diseases such as tetanus, gangrene, botulism, and necrotic enteritis.
The feasibility of using antibiotics
Treatment of paraproctitis with antibiotics, as a rule, is carried out only if indicated. Experts do not recommend using anti-inflammatory drugs unless prescribed by a doctor, since the effect of antibacterial therapy will not follow. In addition, medications can affect the overall clinical picture, which will lead to difficulties in diagnosis.
The pathology cannot be treated therapeutically. Antibacterial therapy is allowed only after diagnosing the disease and determining a treatment regimen. Antibiotics for inflammation can alleviate the patient’s condition, but will not stop the development of the pathological process.
Since the disease is chronic and can only be treated surgically, taking antibiotics as monotherapy is not advisable.
Symptoms of paraproctitis
Paraproctitis - causes, symptoms, treatment, dietary table
Manifestations of paraproctitis can be general and local. General symptoms are characteristic of acute inflammation, to which the body reacts like any other acute infection: fever, weakness, headache.
Local symptoms occur directly in the affected area. In acute paraproctitis, this is pain in the perineum, anus, and sometimes in the buttocks or behind the pubis. Everything will depend on the location of the abscess. The deeper it is, the more vague the discomfort: due to irritation of the outer (serous) membranes of neighboring organs (bladder, uterus, prostate), pain can radiate to various areas of the abdomen. With subcutaneous abscesses in the perianal area, you can see a red and swollen area (infiltrate); in other cases, the doctor can palpate the abscess through the rectum.
With chronic paraproctitis, the general symptoms are usually erased. The temperature is about 37, the patient begins to consider weakness as his normal state. Due to the fact that pus constantly flows through the formed fistula (to put it simply, at some point it “corrodes” the surrounding tissue, breaking out), there is no compression. Therefore, the pain is much weaker than with acute paraproctitis.
Description of the disease
Antibiotics for paraproctitis without surgery are used in the initial stages of development as prescribed by the doctor. The dosage and treatment regimen depend on the severity of the disease. Paraproctitis is purulent formations that occur in the tissue joints that surround the rectum. The disease occurs in the form of inflammatory foci that change the location.
Inflammation occurs accompanied by a feeling of heaviness and discomfort. There is a burning sensation, a pain syndrome that occurs not only when going to the toilet, but also in a calm state. These are the main symptoms. If not treated promptly, purulent masses accumulate, their quantity can reach an impressive volume. Due to further accumulation, the purulent formation may burst when all the contents enter the intestines, rectum.
How and where does paraproctitis develop?
Complications of paraproctitis
If acute paraproctitis is not cured in time, pus can break through the skin - in this case, a fistula is formed and chronic paraproctitis develops. But more often, pus begins to spread throughout the surrounding tissues, forming extensive phlegmons (foci of purulent tissue melting). In especially severe cases, it can break into the peritoneum, causing peritonitis, or provoke sepsis (blood poisoning).
With long-term chronic paraproctitis, it is possible to replace muscle fibers with scar connective tissue (pectenosis), which disrupts the normal functions of the rectum: with formed stool, it is difficult to empty the intestines, and liquid feces do not hold.
Diagnostics
Typically, paraproctitis is diagnosed based on characteristic complaints, examination and digital rectal examination of the rectum. Transrectal ultrasound examination of the pelvic organs helps to detect deep ulcers.
To determine the general condition of the patient, a clinical analysis of blood and urine is done, and the level of glucose in the blood serum is determined.
In chronic paraproctitis, the course of the fistula is determined using contrast radiography: the fistula is filled with a radiopaque substance and a series of photographs is taken.
Types of drugs for local treatment
During the treatment of paraproctitis, topical antibacterial agents are more often used after surgery. In the postoperative period, wound treatment with ointments and anti-infective prophylaxis with rectal suppositories are recommended. Ointments for paraproctitis with antibiotics are presented in the table.
| Drug name | Active substance | Properties and pharmacological action |
| Fuzimet | Fusidic acid, dioxomethyltetrahydropyrimidine | Fuzimet prevents the spread of infection and enhances the regeneration process |
| Levosin | Trimecaine, dioxomethyltetrahydropyrimidine, chloramphenicol, sulfadimethoxine | Levosin has anti-inflammatory, analgesic and anti-infective effects |
| Ichthyol | Ichthammol | Ichthyol ointment for paraproctitis has an analgesic and anti-inflammatory effect, relieves swelling and accelerates wound healing |
| Levomekol | Chloramphenicol | Levomekol for paraproctitis prevents suppuration and inflammation of wounds, increases the rate of regeneration |
| Vishnevsky ointment | Xeroform, tar, castor oil | Vishnevsky ointment for paraproctitis has an antiseptic effect, reduces swelling and promotes tissue healing |
Apply ointments during the dressing process for three weeks.
Levomekol ointment can be used to treat wounds.
Suppositories for paraproctitis in adults are prescribed by a doctor in case of preparation for surgery, inflammation of the rectum after surgery, or in case of contraindications to surgical treatment. Rectal suppositories for paraproctitis are presented in the table.
| Name of candles | Active ingredient | Properties |
| Proctosedyl | Framycetin | Proctosedyl has an antiseptic and analgesic effect |
| Olestesin | Sodium etazol sulfonamide, anesthesin, sea buckthorn oil | Olestesin has anti-infective and antifungal properties and has an analgesic effect. |
Candles can only be used as prescribed by the attending physician. Self-medication with rectal suppositories is unacceptable without appropriate indications.
Treatment of paraproctitis
Localization of inflammation in paraproctitis
Paraproctitis can only be cured by surgery. In acute cases, the abscess is opened and drained - conditions are created for the free outflow of pus and wound discharge. The source of infection (crypt) is also excised to prevent relapse of the disease. Antibiotics are prescribed orally or by injection to destroy the root cause of the disease.
In chronic paraproctitis, despite the constant outflow of pus, the abscess cavity is not completely emptied, so it also has to be opened. After cleansing the area of purulent-necrotic (dead) masses, the fistula tract is excised and the tissue is sutured, leaving drainage. In the same way as in an acute process, antibacterial drugs are recommended.
After surgery for paraproctitis, a “slag-free” diet is prescribed for the first three days to minimize the formation of feces. The diet includes broths, eggs, cottage cheese, lean meat. Any products containing fiber are excluded: cereals, cereals, fruits and vegetables. From the fourth day, the diet is gradually expanded in order to achieve natural soft bowel movements on days 5–7.
Smoked meats, spices, canned food, and alcohol are prohibited for at least 3 months after surgery.
Is antibiotic therapy effective?
This condition is removed surgically. Only in exceptional situations is it possible to treat paraproctitis with antibiotics.
This becomes acceptable if the purulent formation is localized close to the skin and does not form a fistula . In other cases, treating the disease at home is ineffective and soon becomes chronic.
The most effective way to cure paraproctitis is surgery .
However, there are cases in which there are contraindications for its implementation. This may be the period of lactation or the presence of concomitant diseases in the body. Surgery is also contraindicated when the patient is in remission. Effective means of getting rid of pathology in an inoperable way are:
- the use of baths and lotions;
- the use of suppositories with antibiotics for paraproctitis (ichthyol suppositories, suppositories with propolis, with methyluracil, Anuzol, Posterizan, Ultraproct, Olestesin);
- applying Vishnevsky ointment;
- procedures with therapeutic enemas filled with infusions of Sage, Yarrow, Chamomile and Calendula.
Important! If the disease is in a chronic stage, stopping it using folk methods is useless! Using remedies such as suppositories, antibiotics and lotions can only stop the inflammation process. For remission to occur, it is necessary to get rid of purulent accumulations. Only surgery can help here.
When a patient is diagnosed with paraproctitis, treatment with antibiotics without surgery is prescribed if there are concomitant inflammatory processes in the human body that triggered its development, or other factors that only a proctologist can identify by collecting a wide range of tests.
Groups of antibacterial agents
A competent approach to stopping the disease with the help of antibacterial agents will significantly reduce its development. Antibiotics for the treatment of paraproctitis are selected exclusively by the attending physician based on the identification of the causative agent of the infection.
This is carried out by obtaining research data on bacteria with the determination of a pronounced microbial pathogen in relation to groups of antibiotic medications.
Today, the following groups of antibactericidal varieties are applicable:
- semisynthetic penicillins;
- cephalosporins;
- macrolides.
These groups may be present in various medications. Depending on the scale of the inflammatory process, they can be in the form of suppositories containing antibiotic components, tablets, capsules, injections.
If, based on an in-depth study, the above diagnosis is made, the dosage of antibiotics for paraproctitis without surgery is prescribed by the attending physician.
Names of antibacterial agents by group
- Semi-synthetic penicillins include: Oxacillin, Amoxicillin, Ticarcillin, Azlocillin.
- Cephalosporins include: Bayotax, Bastum, Betasporina, Bidroxil, Biotraxon, Biotum, Boncephin.
- Macroclids include: Erythromycin, Roxithromycin, Clarithromycin, Oleandomycin, Azithromycin, Josamycin, Midecamycin, Spiramycin.
In addition to the listed antibiotic agents by group, there are other antibacterial components for local treatment that contain antibacterial components.
Important! What antibiotics to take for paraproctitis can only be decided by the attending doctor, so you should not self-medicate and choose your own cure to eliminate the source of infection!