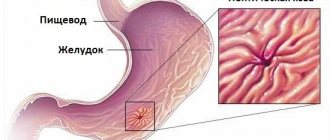
Varicose veins develop when the blood supply to the stomach is disrupted. The condition is usually accompanied by changes in the structure of blood vessels, such as dilation, elongation, and the formation of loops or nodes. Pathology appears against the background of liver damage, in particular with cirrhosis. An invariable companion of varicose veins in the tissues of the stomach is small or heavy bleeding.
Descriptions and features
Gastric varicose veins are a dangerous pathology. The condition is characterized by an increase, often dilatation, of the veins of the organ with the formation of blood clots. The insidiousness of the disease lies in the absence of symptoms at an early stage, so timely diagnosis is almost impossible. Mostly men suffer from this disease. The main provoking factors for the development of the disease, as well as liver damage, are:
- alcohol;
- unhealthy diet;
- uncontrolled drug treatment.
Etiology and pathogenesis of the disease
The classification for varicose veins of the esophagus is as follows:
- Grade 1 esophageal pathology is characterized by an increase in the diameter of the veins (three mm);
- in the second degree, the size of the arteries is 3–5 mm in diameter;
- Grade 3 esophageal pathology is determined by the size of the veins (diameter more than 5 mm);
The arterial expansion of the esophagus is due to its anatomical connection with the portal vein system, as well as the spleen and other organs of the gastrointestinal tract. Phlebectasia develops against the background of diseases leading to blockage of venous networks and the formation of collaterals and aneurysms.
There are congenital and acquired varicose veins of the digestive tube. The first disease is less common than the second disease. With acquired varicose veins in the esophageal tube, the saccular arterial dilatations are significantly increased.
Symptoms
Gastric varicose veins have a poor clinical picture. Symptoms are often similar to other gastrointestinal pathologies. However, there are distinctive features:
- Bloody vomiting with black vomit, which indicates the opening of gastric bleeding. Vomiting may be frequent and contain pink mucus.
- Increased heart rate with frequent interruptions.
- Abdominal pain.
The initial stages of gastric varicose veins are often accompanied by severe heartburn, which, although it causes discomfort, does not cause the need to go to the doctor. As the pathology develops, gastric bleeding begins. This condition is accompanied by symptoms such as:
- ascites, when free extrudate accumulates in the peritoneum, which provokes a strong increase in the size of the abdomen;
- profuse, bloody vomiting that does not cause pain;
- tachycardia with erratic and rapid pulse;
- hypotension, characterized by a sharp decrease in blood pressure;
- hypovolemic shock, accompanied by a sharp decrease in the effective volume of circulating blood.
Signs signaling the development of varicose veins in the stomach
But if you take a closer look at this problem, the differences can still be identified in a timely manner:
- severe vomiting mixed with biological fluid and black vomit;
- frequent vomiting with pink mucus in it;
- pain in the abdomen;
- rapid heart rate, which is accompanied by frequent interruptions.
As a rule, the pattern of bleeding from the upper gastrointestinal tract, often massive, develops suddenly, not accompanied by pain. Signs of shock may be detected. Blood loss usually occurs from the lower part of the esophagus, less often from the fundus of the stomach. Blood loss from gastric varicose veins can also be acute, but more often - subacute or chronic.
Bleeding into the gastrointestinal tract due to liver dysfunction contributes to the increase in portosystemic encephalopathy.
At the initial stage of the disease there are no specific symptoms. Therefore, it is difficult to determine the problem. But as the problem develops, the patient experiences certain signs of phlebectasia.
- Heaviness and discomfort in the chest.
- Enlarged abdomen due to accumulation of fluid in the abdominal cavity.
- A “jellyfish head,” as it is called, may appear in the anterior part of the abdominal wall. This is a pattern of veins dilated in the esophagus.
- Shortness of breath as a result of activity.
- Severe heartburn regardless of food intake.
- Swallowing dysfunction.
It’s great if the patient pays attention to the listed signs and consults a doctor. Diagnosis of the disease based on the listed symptoms will make it possible to take urgent measures to treat gastric varicose veins.
When bleeding begins, the signs of the problem become more pronounced.
- Vomiting with bloody discharge.
- Black stool, as well as noticeable admixtures of blood in it.
- Decreased blood pressure.
- Cardiopalmus.
- State of shock.
Bleeding from varicose veins can be minor, but most often it is massive. Treatment must be started immediately, as the problem can lead to serious deterioration or death.
Causes of gastric varicose veins
Gastric varices appear as a result of portal hypertension or increased pressure in the portal vein. The normal pressure in this vein is up to 6 mm Hg. Art. If this value jumps to 12-20 mm Hg. Art., blood flow is disrupted and vasodilation occurs. The root cause of portal hypertension is compression of the portal vein, which can cause thrombosis or stone passage in gallstone disease. Other causes of gastric varicose veins are:
- dysfunction of the pancreas, stomach;
- cirrhosis, hepatitis;
- echinecoccosis;
- tuberculosis;
- polycystic disease;
- acquired or congenital fibrosis;
- sarcoidosis;
- tumors, cysts, adhesions of various etiologies;
- aneurysms of the arteries of the spleen or liver;
- eosinophilic gastroenteritis;
- intestinal obstruction;
- general cardiovascular failure.
Sometimes gastric varicose veins are preceded by a sudden load: heavy lifting, severe fever. Rarely, the disease is congenital. The reasons for this anomaly have not yet been discovered.
Causes of varicose veins
Varicose veins of the esophagus can be acquired or be a congenital pathology. The acquired form appears more often and develops against the background of portal hypertension.
The condition is characterized by excess pressure in the portal vein, which is responsible for blood circulation from organs to the liver. Portal hypertension provokes thinning of the venous walls with an increased risk of internal bleeding.
The direct cause of the development of the disease is a blockage of blood supply.
- liver pathologies - cirrhosis, hepatitis, tuberculosis, etc.;
- vascular thrombosis;
- persistently high blood pressure;
- thrombophlebitis (Chiari syndrome);
- compression of the portal vein by tumor or cystic formations, enlarged lymph nodes, gallstones.
Upper varicose veins of the esophagus are provoked by the following reasons:
- malignant goiter;
- benign tumor (angioma);
- vascular problems in Rendu-Osler syndrome.
Less commonly, varicose veins of the esophagus develop against the background of chronically poor circulation due to cardiovascular insufficiency. More often, the pathology appears in men aged 50 years and older. The causes of the congenital form are not clear.
Gastric varicose veins can develop due to increased pressure in the portal vein. Initially, a compression process occurs in the portal vein, which provokes a blood clot or stone if a person suffers from gallstone disease.
Varicose veins of the mucous membrane of the stomach and the lower third of the esophagus are far from being as common a pathological condition as varicose veins of the lower extremities or hemorrhoidal plexus, however, a number of patients experience dilation of the veins of the mucous membrane of the gastrointestinal tract in the lower part of the esophagus and the cardiac part of the stomach of varying degrees. degree of expression.
Unlike varicose veins of the lower extremities, the causes of this condition and the factors that contribute to its progression are completely different, as are the symptoms, which are often completely absent in the first stages and appear exclusively in the terminal stages of the disease.
Varicose veins of the stomach and lower esophagus are a disease characterized by a violation of the outflow of blood from the veins of these organs and a change in their structure (vessels dilate, become unnaturally looping, long and form nodes).
Gastric varicose veins or phlebectasia is a serious pathology that requires urgent measures to be taken to solve the problem. The disease provokes protrusion of the walls of the stomach and an increase in the lumen. As a result, tortuosity is observed in the area of the vessels, and this requires proper treatment.
The main reason for the development of gastric varicose veins is portal hypertension, which provokes swelling of the veins in the esophagus. Often this condition is observed with cirrhosis of the liver, as many scars appear on it. But this is not the only reason for the manifestation of an unpleasant disease.
There are other reasons that can cause the disease:
- Liver diseases that cause impaired blood flow.
- The appearance of blood clots.
- Compression of the rotary vein by tumors.
- Vascular and heart failure.
Particular attention should be paid to diagnosing the likelihood of venous disease in patients suffering from liver cirrhosis and hepatitis. Since these organs become even more vulnerable and untimely treatment can lead to negative consequences.
Diagnosis of the disease
Detection of varicose veins is possible only through instrumental examination. For this purpose the following methods are used:
- General and clinical blood tests, which are necessary to assess the general condition of the patient.
- Functional and hepatic examinations to determine coagulopathy.
- X-ray with contrast (barium sulfate), carried out to assess the functionality of the digestive tract.
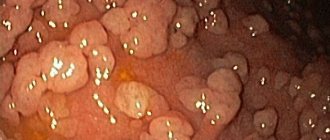
- Esophagogastroscopy, used to visualize the condition of the internal walls of the stomach. The method is highly accurate, but requires increased attention and accuracy, since the affected tissues are fragile and the probe can cause bleeding.
- Ultrasound of the abdominal organs, which is necessary to confirm the diagnosis.
Types and degrees of varicose veins
The classification of the disease consists of the degree of damage to the veins. There are four degrees. Depending on the degree of varicose veins, treatment is prescribed. The greater the degree, the more likely surgical treatment is.
In total, there are four degrees of varicose veins of the stomach or esophagus.
- Degree 1 – no symptoms are observed, venous ectasia is isolated, which does not prevent the patient from feeling great. The first degree of the disease can only be determined using endoscopy.
- Grade 2 – vascular structures become tortuous and uneven. But at the same time, swelling does not exceed 3 mm, and the gaps narrow to insignificant distances. In this case, bleeding is rare. The problem can also be identified mainly using x-rays or endoscopy. Symptoms are not expressed.
- Degree 3 – the venous lumen noticeably narrows, the veins bulge. At this stage, the nodes are clearly visible, the tone of the walls narrows. The main symptoms are already appearing; all that remains is to notice them in time, since the risk of bleeding at this stage of the disease increases markedly. Treatment cannot be delayed at the third stage.
- Degree 4 – the nodes are clearly visible, the lumens are narrowed, the gastric mucosa is seriously thinned. A whole thread of affected vessels may diverge from a large node. All of them are so thin that bleeding can open at any moment. If this happens, the patient is in serious danger.
To diagnose venous disease and determine its degree, doctors use different research methods:
- Laboratory tests of blood, urine and feces.
- Ultrasound of the abdominal organs.
- Esophagoscopy.
- X-ray studies.
Operation
Surgery can be performed in three ways:
- Ligation of dilated veins. For this, a special rubber bandage is used. The effectiveness of the technique is higher than sclerotherapy.
- Shunting in intrahepatic tissues. The technique is necessary to lower blood pressure. To do this, a stent is inserted into the middle of the liver. The procedure is performed under X-ray control. The goal is to create a connecting bridge between the hepatic and portal veins.
- Splenorenal shunting. The technique is used for preventive purposes - to prevent the development of bleeding. To do this, the veins of the spleen and left kidney are combined with a shunt.
Diet therapy
To treat gastric varicose veins, it is important to maintain proper nutrition. The basic principles are as follows:
- Fractional meals in small portions - up to 6 times a day.
- The last snack is 3 hours before going to bed.
- Increasing in the diet the amount of foods rich in vitamins such as:
- vitamin E (greens, yolk, corn or sunflower oil);
- vitamin C (berries, potatoes, fresh peppers, all types of citrus fruits);
- rutin (nuts, tea, grapefruit, currants);
- bioflavonoids (cherries);
- plant fibers (legumes, fresh vegetables and fruits).
- Organize plenty of drinking - up to 2.5 liters of water per day.
- Complete rejection of harmful products:
- alcohol;
- concentrated black tea, coffee;
- sweets and sugar;
- hot seasonings and spices;
- flour products.
- Preferred culinary processing is boiling, baking in the oven, stewing, steaming.
- Dishes must be warm.
Treatment
Pathology is most often detected at a late stage, which often leads to hypovolemic shock or death. The patient is required to undergo immediate hospitalization and resuscitation. The first step is to stop the bleeding, stabilize the body’s condition, replenishing the blood volume.
Drug treatment
Treatment of varicose veins involves squeezing the problem area. This is how you get rid of bleeding. The effectiveness of treatment is 90%. When operating on damaged vessels of the esophagus, relapses are possible. Often another surgery is performed. To increase the chances of recovery, the following methods are used:
- Injection of a special solution into the vein that has ruptured to reduce the outflow of blood.
- Monthly repetition of actions aimed at stopping possible internal bleeding.
- The use of drugs that affect gastric juice to reduce pressure on the walls of blood vessels.
- Astringents that stop possible bleeding.
- Multivitamin complexes to increase vascular elasticity.
Surgical intervention
Measures are carried out in several ways: damaged veins are ligated using a rubber bandage, intrahepatic material is shunted to reduce pressure. A special device is inserted into the liver to prevent blood from accumulating in the cavities, preventing bleeding from occurring. Actions are carried out using an X-ray machine to avoid possible errors.
The third method is splenorenal shunting. Used to prevent fluid accumulation. A shunt connects certain veins, preventing hemorrhage.
Folk remedies
To supplement treatment with basic remedies, traditional medicine can be used. The activities improve intestinal function and improve the choleretic process. The following drugs are used for treatment:
- Tincture of Sophora japonica. 1 tbsp. l. The drink is diluted in 1 glass of boiled water. Drink the composition 4 times a day before meals.
- Rose hips or rowan berries: 1 tbsp. l., mixed with 0.5 l. water. The liquid with fruits is kept on the fire for 5 minutes, then cooled and drunk. Drink 0.5 liters daily. composition, in parts, at regular intervals.
- Chestnut flower drops (sold at pharmacies). Add 30 drops of solution to a glass of warm water. Drink a glass a day.
- Propolis tincture. Mix and use in the same way as the previous composition.
- Liquid formulations of calendula, chamomile: mix them, adding 10 drops of each product to a glass of water. Use the solution warm 4 times a day for at least a month.
Do not forget that the traditional method of treatment does not help get rid of a dangerous disease, but only serves as an addition to the main treatment.
Nerves and varicose veins
The condition of the body and its performance depend on the stability of the nervous system. When a person is exposed to significant and prolonged stress, anxiety, or depression, the digestive system suffers first. Neurological causes of the development of varicose pathology:
- Chronic state of hatred.
- Feeling of chronic fatigue, severe overstrain.
- Loss of strength and spirit, disappointment and moral fatigue.
Therefore, during treatment it is important to have a positive attitude and eliminate all irritating factors.