Pancreatogenic diabetes mellitus appears most often after pancreatitis, but it can also be caused by trauma, surgery, or a tumor of the pancreas. The development mechanism is associated with the destruction of cells that produce insulin and other hormones. The course is often hidden and does not manifest symptoms for a long time. Features: provokes alcoholism, patients are not obese, there is a tendency to drop sugar (hypoglycemic states).
To identify it, a test for glucose tolerance (sugar load) is required; fasting sugar levels and high levels after meals are typical. Treatment includes diet, the use of enzymes (Festal, Mezim), tablets to reduce sugar.
What is pancreatogenic diabetes mellitus
Pancreatogenic diabetes mellitus is an increase in blood sugar due to pancreatitis (inflammation of the pancreas). This type of diabetes is called secondary and differs in its course from types 1 and 2.
It is found in 10-90% of cases of chronic inflammatory process, since the connection between pancreatitis and diabetes mellitus is not always detected in a timely manner. It usually affects men who are prone to drinking alcohol and fatty foods. Specific pancreatogenic diabetes mellitus complicates acute inflammation of the pancreas in 15% of cases.
What is the connection between the pancreas and diabetes?
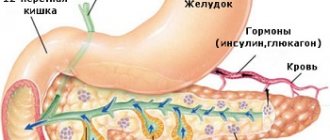
The pancreas is an organ that produces insulin and plays an important role in regulating blood glucose levels.
There is a clear connection between the pancreas and diabetes. Type 1 diabetes occurs when the pancreas does not produce enough insulin. Type 2 diabetes develops when the body cannot use insulin properly.
In this article we will look at the connection between the pancreas and diabetes. We will also describe complications of diabetes related to the pancreas and other organ disorders.
How pancreatitis and diabetes are related
Acute and long-term chronic pancreatitis leads to diabetes mellitus, which is explained by:
- destruction of pancreatic tissue;
- a decrease in the number of cells that produce insulin, glucagon and pancreatic protein (polypeptide);
- impaired digestion of food;
- deterioration of the formation of incretins (hormones that stimulate the release of insulin in response to food intake) in the intestines.
Therefore, diabetes mellitus against the background of pancreatitis occurs against the background of insulin deficiency. Lack of the hormone prevents the absorption of carbohydrates, blood sugar rises after meals and does not decrease enough. Due to digestive disorders and a simultaneous deficiency of many hormones that regulate digestion, diabetes mellitus after pancreatitis occurs in an unusual manner. Patients experience frequent changes in blood glucose.
Classification
Pancreatogenic diabetes mellitus was at one time included in the classification under the designation type 3c diabetes; it occurs according to the development mechanism:
- fibrocalculous - against the background of chronic inflammation, areas of compaction, proliferation of scar tissue and calcifications (deposits of calcium salts) are formed;
- protein deficiency – occurs against the background of protein deficiency.
Depending on the causes of pancreatitis itself, diabetes may be due to alcohol intoxication or diseases of the liver, biliary tract (biliary). In the first case, a more severe disorder of carbohydrate metabolism was noted.
How is the pancreas related to diabetes?
Diabetes is characterized by high blood sugar levels. This is a consequence of insufficient insulin production, which can be one of the consequences of problems with the pancreas. People with diabetes experience high or low blood sugar at different times, depending on what they eat and whether they take insulin or diabetes medications. Type 1 and 2 diabetes are related to the pancreas.
Diabetes mellitus type 1
Type 1 diabetes occurs when the pancreas does not produce enough or any insulin. Without insulin, cells cannot get enough energy from food. This form of diabetes occurs as a result of the immune system attacking the insulin-producing beta cells of the pancreas. Beta cells become damaged, and over time the pancreas no longer produces enough insulin to meet the body's needs. People with type 1 diabetes can balance their blood glucose levels by taking insulin injections. Doctors call this type “juvenile diabetes” because it often develops in childhood or adolescence. There is no clear cause for type 1 diabetes. Some evidence suggests that this form of diabetes is the result of genetic or environmental factors.
Diabetes mellitus type 2
This type occurs when insulin resistance develops. Although the pancreas still produces the hormone, the body's cells cannot use it effectively. As a result, the pancreas begins to produce more insulin for the body's needs. When there is not enough insulin in the body, diabetes develops. Over time, beta cells become damaged and may stop producing insulin altogether. Type 2 diabetes also causes high blood sugar levels, which makes it difficult for cells to get enough energy. Type 2 diabetes can be the result of genetics and family history. Lifestyle factors such as obesity, lack of exercise and poor diet also play a role in this. Treatment often includes physical activity, improved diet, and certain medications. A doctor can detect type 2 diabetes in an early stage called prediabetes. A person with prediabetes can prevent or delay the disease by making changes to their diet and exercise.
How does pancreatitis manifest in type 1 and type 2 diabetes mellitus?
In diabetes mellitus types 1 and 2, acute pancreatitis occurs with severe symptoms:
- pain in the epigastric region, in the left hypochondrium, sometimes girdling, radiating under the left shoulder blade;
- the pain attack does not subside, and its intensity only increases, becoming worse when lying on the back;
- The condition is worsened by spicy and fatty foods, fried foods, and alcohol;
- vomiting is uncontrollable and does not provide relief;
- increased body temperature;
- fever;
- yellowness of the sclera of the eyes, less often of the skin;
- bloating, heartburn.
With chronic pancreatitis, symptoms periodically decrease, characterized by alternating diarrhea and constipation, weight loss, and aversion to food. As pancreatitis progresses, exacerbations become more frequent, and periods of remission (pain subsidence) shorten.
Features of the flow
Diabetes mellitus when developing after pancreatitis has the following characteristics:
- usually appears in adulthood in patients with a thin or normal build (type 1 occurs in children and adolescents, and type 2 in obese people);
- there are always pronounced symptoms of digestive disorders - bloating, flatulence, nausea, heartburn;
- there is pain in the upper abdomen, which gets worse as it gets worse;
- the increase in blood glucose is moderate;
- Sugar often drops, but there are no increases typical for diabetes (hyperglycemic and ketoacidotic states);
- with sugar up to 10 mmol/l there are no symptoms, but only at higher levels thirst, dry mouth and skin, and copious urine output occur.
Diagnosis of the patient
It is quite difficult to identify the disease, since the signs of diabetes are often erased. For diagnosis, all patients with pancreatitis need to consult an endocrinologist; he first identifies additional risk factors:
- previous surgeries, abdominal injuries;
- alcohol consumption;
- use of hormonal drugs.
Laboratory examination includes:
- general blood test;
- glucose tolerance test: usually on an empty stomach, sugar is normal or slightly elevated, and after a sugar load high levels are found;
- blood biochemistry with determination of the activity of pancreatic enzymes (amylase, lipase, trypsin);
- urine test (usually no glucose and ketone bodies).
Instrumental diagnostic methods:
- Ultrasound of the abdominal organs;
- tomography of the pancreas.
These methods of studying the structure help to find places with heterogeneous tissue, compactions, and calcifications. If the endocrinologist has doubts whether diabetes mellitus is a classic type 1 variant, he prescribes a blood test for antibodies to pancreatic cells, C-peptide and insulin. Type 2 is characterized by obesity, tissue resistance to insulin, and attacks of low blood sugar are extremely rare.
Diet for diabetes mellitus and pancreatitis: principles of nutrition
The basic rules for creating a diet for diabetes and pancreatitis are similar in nutritional principles and prohibitions on foods containing sugar, alcohol and fatty foods. Also recommended:
- introduction of vegetables and cereals into the diet;
- use of lean varieties of fish and meat;
- culinary processing in the form of boiling, baking, frying and stewing with oil is not allowed;
- The menu should include non-acidic and low-fat dairy products - yogurt, fermented baked milk, cottage cheese;
- meals are frequent and small;
- during an exacerbation, it is necessary to limit animal fats as much as possible and grind food (mashed soups and cereals, meat is twisted twice through a meat grinder).
Prohibited Products
For diabetes, the list of prohibited foods includes:
- alcoholic and carbonated drinks, kvass;
- lamb, pork, lard, fatty and spicy cheese;
- heavy cream and sour cream, butter;
- fats: meat, fish, mushroom;
- semi-finished products;
- canned food, marinades, pickles, smoked meats;
- sausages;
- chocolate;
- ice cream;
- confectionery;
- baking, puff pastry;
- fast food, chips, crackers with salt and spices;
- condensed milk;
- mayonnaise, ketchup, vinegar, horseradish, mustard, pepper;
- radishes, spinach, onions, garlic;
- millet, pearl barley;
- sour fruits and berries.
Authorized Products
What you can include in your diet:
- vegetarian soups;
- meat: beef, veal, chicken, turkey, rabbit;
- fish: pike, pollock, cod, pike perch, perch;
- cottage cheese 2-5% fat, 1.5-2% yogurt, fermented baked milk, yogurt, 10% sour cream;
- vegetables: zucchini, pumpkin, cauliflower, broccoli, green beans, young green peas;
- egg whites for steam omelet;
- cereals: buckwheat, oatmeal, rice, durum pasta;
- baked apples, plums and apricots for adding to compote, casseroles;
- dried gray bread;
- compote, jelly, weak tea, herbal tea made from mint and chamomile;
- Stevia or fructose is added instead of sugar.
Diabetes and pancreatic cancer
According to the Pancreatic Cancer Society, people who live with diabetes for 5 years or more are 1.5 to 2 times more likely to develop pancreatic cancer.
The onset of type 2 diabetes later in life may be a symptom of this type of cancer.
The direct link between diabetes and pancreatic cancer is still poorly established. Diabetes is known to increase the risk of developing this type of cancer, and pancreatic cancer can sometimes lead to diabetes.
Other risk factors for pancreatic cancer:
- obesity
- aging
- poor nutrition
- smoking
- genetic inheritance
In the early stages, this type of cancer may not cause any symptoms. Doctors most often diagnose it in the later stages, when the patient is usually no longer operable. Therefore, it is necessary to undergo an annual examination of the gastrointestinal tract.
Example menu for pancreatitis and diabetes mellitus
With exacerbation of pancreatitis and diabetes mellitus, the menu may be as follows:
- breakfast: oatmeal, baked apple without peel, weak tea;
- second breakfast: steamed egg white omelette;
- lunch: soup from zucchini, cauliflower, carrots, chicken breast cutlets (steamed), viscous buckwheat porridge;
- snack: cottage cheese soufflé, yogurt;
- dinner: boiled fish with boiled potatoes, compote;
- before bed: fermented baked milk.
Outside of an exacerbation, the diet can be expanded:
- breakfast: rice casserole with pumpkin, endive with milk;
- second breakfast: dried or yesterday’s bread with Adyghe cheese, tea;
- lunch: vegetable soup with fish meatballs, baked turkey with carrots and herbs, compote;
- afternoon snack: cottage cheese with baked apple, jelly;
- dinner: boiled chicken with buckwheat porridge, boiled cabbage with herbs, weak tea;
- before bed: kefir, fructose cookies.
Treatment of diabetes mellitus with pancreatitis
The most important condition in the treatment of diabetes mellitus and pancreatitis is the simultaneous treatment of two diseases. To do this you need:
- strictly adhere to the diet on an ongoing basis, and not just during an exacerbation;
- stop smoking and drinking alcohol;
- take medications with enzymes for replacement therapy (Creon, Festal);
- use glucose-lowering tablets with mandatory daily monitoring of blood sugar levels (Siofor, Glucophage), it should not be lowered below 4.5 mmol/l.
If an operation is performed for pancreatitis (partial or complete removal of the tail), then a patient with diabetes mellitus must be switched to insulin. Injections are given in small doses before meals. After stabilizing the sugar level, it is possible to prescribe tablets on an ongoing basis.
In extremely severe cases of pancreatitis, surgery may be necessary to transplant the patient's own islet cells that produce insulin. After this, the pancreas is removed. This treatment method is available only in large specialized endocrinology centers.
Treatment
The pancreas is restored without difficulty in diabetes mellitus. After determining the disease, the specialist develops a suitable therapeutic method and diet, and recommends visiting a nutritionist. This is the main stage in the process of pancreatic restoration.
Diet is considered a fundamental factor influencing the improvement of organ function and the level of glucose secretion.
In addition to following a diet, you will have to exercise regularly. If physical activity and proper diet do not bring the desired result, the doctor prescribes medicine. Medicines promote the production of necessary hormones or stimulate the use of natural insulin that is produced in the body.
Medicines
Medicines for the pancreas for diabetes mellitus relieve pain and inflammation, are administered through an IV, and prevent the activity of pancreatic enzymes. In difficult situations, antibiotics have to be used.
It is more difficult to restore the pancreas with pancreatitis. The patient has to be admitted to the hospital. First, the inflammation is eliminated. For pancreatitis, all procedures are carried out under the supervision of specialists.
The first few days of therapy require refusing to eat. Fasting will help reduce the intensity of inflammation and normalize the production of pancreatic enzymes. After this, the patient follows a diet and takes medications for 2 weeks, while the missing enzymes are restored. You should not drink alcohol, fatty, smoked, or pickled foods.
The number of beta cells decreases in pancreatitis, and restoration with the help of medications is impossible. Surgical procedures help provide temporary relief to the patient's condition. The best treatment option is insulin therapy.
Folk recipes
In order to improve the functioning of the pancreas in diabetes, traditional medicine is used in combination with medications. At home, you can use decoctions of medicinal plants.
Here are a few recipes:
- Tincture of bay leaves. The ingredients are brewed in boiling water for half an hour. The infusion is taken one tablespoon before meals. This decoction improves metabolism and normalizes the amount of sugar.
- Chamomile, mint, and St. John's wort in combination can achieve a general strengthening effect and reduce pain.
- Monastic tea helps strengthen the pancreas and normalize sugar levels.
Before using decoctions, you should first consult your doctor.
Such drugs do not completely eliminate the disease, but in combination with other medications they help alleviate the patient’s condition.
Diet
The diet is used in combination with other methods. A diabetic should eat only healthy foods. Recovery of the pancreas takes time. Maintain proper nutrition, do not eat too much protein foods, fats, carbohydrates. Nutritionists assign a glycemic index to all types of foods. A table with these values helps determine the appropriate diet for each patient.
Recommendations for adjusting your diet:
- You can consume approximately 350 g of carbohydrates, 100 g of proteins, 60 g of fat per day.
- It is necessary to organize fractional meals in small portions 5-6 times a day.
- You need to cook food in a double boiler, in the oven, or cook. You can’t fry anything, and baked foods are in a state of remission.
- It is undesirable to use hot seasonings, garlic, vinegar, and pepper. The intestinal mucosa will be irritated by such substances.
- Fatty, salty, smoked rich foods should be excluded from the diet.
The functioning of the pancreas in diabetes mellitus requires regular monitoring by a doctor. Traditional medicine recipes in combination with diet and medications help improve the condition of patients.
Possible complications without treatment during exacerbation of pancreatitis in diabetes mellitus
If the patient does not adhere to treatment and neglects the diet, smokes, drinks alcohol, then frequent exacerbations of pancreatitis and worsening of diabetes mellitus are inevitable. Vascular complications develop from:
- kidney – diabetic nephropathy;
- retina – retinopathy;
- bloodstream – angiopathy;
- nervous system: peripheral (limb) in the form of neuropathy, brain – encephalopathy.
Due to impaired digestion of food, vitamins and microelements are insufficiently absorbed, so vascular damage is severe. Patients with type 3c diabetes are characterized by sharp fluctuations in blood sugar. Attacks of hypoglycemia occur with a feeling of hunger, sweating, general agitation, trembling of the hands, the skin turns pale and becomes covered in cold sweat. If you do not take sweet tea or a spoonful of honey at this time, loss of consciousness occurs with convulsions, possibly a coma.
Causes of the disease
The leading causes of the pancreatogenic form of diabetes mellitus include chronic and acute damage to the pancreas. In addition, there are factors that can provoke the formation of an inflammatory reaction in the internal organ. We are talking about the consumption of alcoholic beverages and surgical interventions on the pancreas.
Diabetes mellitus and pancreatitis can develop due to the presence of stones in the gallbladder area. Excess weight, consumption of unhealthy foods, as well as drug-induced organ damage deserve special attention. The provoking factor may be an oncological disease (including metastasizing and regardless of stage). We should not forget about traumatic damage to the pancreas, the development of pancreatic necrosis (against the background of pancreatitis) and genetic predisposition.
Symptoms, classification, treatment of diabetic nephropathy
Prognosis and prevention
If you make a timely diagnosis of diabetes mellitus against the background of pancreatitis and strictly follow the recommendations for therapy, then the prognosis for pancreatogenic increase in blood sugar is good. It is possible to normalize digestion and carbohydrate metabolism. The prognosis is worse for tumors and extensive surgery on the pancreas. Factors that complicate the treatment process include alcoholism, smoking, and ignoring the diet.
To prevent type 3c diabetes, it is important to consult a doctor if you have symptoms of pancreatitis and undergo a full examination by an endocrinologist. At least once a year (even if tests and health are normal), preventive courses of medication are taken to improve the functioning of the pancreas. The diet is prescribed on an ongoing basis.
Pancreatogenic diabetes mellitus occurs due to inflammation of the pancreas, it leads to sharp fluctuations in blood sugar. It is imperative to follow a diet, use enzymes and sugar-lowering tablets, and avoid alcohol.
Other diseases of the pancreas
Cystic fibrosis can also lead to the development of insulin-dependent diabetes (type 1).
In a person with cystic fibrosis, persistent sticky mucus causes scar tissue to form on the pancreas, and scarring can prevent the organ from producing enough insulin. As a result, cystic fibrosis-related diabetes (CFRD) may develop.
The signs and symptoms of CFRD may resemble those of cystic fibrosis. A person may not know that he does not have cystic fibrosis, but diabetes, until he passes the appropriate tests.