Ulcer penetration is a common consequence of gastric ulcer, which is detected in almost 40% of patients with this complicated gastropathology. It is observed much more often in men, and more than 60% of cases are people of working age over 40 years old. According to statistics, in approximately 90% of cases a penetrating ulcer is localized in the piloantrum of the stomach and the initial part of the duodenum.
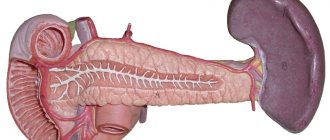
In more than 60% of cases, the ulcer grows into the pancreas. Damage to the liver, lesser omentum and hepatoduodenal ligament occurs in 30% of cases (the distribution between organs is approximately the same). In almost 2% of cases, penetration into the intestines, gallbladder and mesentery is observed. In a quarter of all cases, penetration is accompanied by bleeding, in a third of cases – by perforation and stenosis.
What is it - penetration of an ulcer
Ulcer penetration is a dangerous consequence of underlying gastropathology. In most cases, this complication is caused by the progression of the pathological process in chronic peptic ulcer. The inflammatory process affects the mucous tissues of the stomach and duodenum, and ulcers form.
When the pathology progresses and affects deeper layers, there is a likelihood of the following conditions:
- The ulcerative defect opens into the cavity (perforation).
- The ulcerative defect penetrates into a neighboring organ (penetration).
The development of the pathological process occurs inside the walls of the stomach and duodenum. When an ulcerative defect becomes end-to-end, inflammation spreads to the adjacent organ, to the area where the ulcer has spread beyond the main affected organ. Typically, erosion penetrates into neighboring organs when the area of damage to the stomach or duodenum is small. If the area of erosive lesion is more than 1.5 cm, perforation of the ulcer develops.
When erosive tissue damage spreads to neighboring organs, this means that the human body has a tendency to adhesive processes.
Mechanisms of penetration of gastric ulcers
As a result of the progression of necrosis, all layers of the stomach are destroyed, and the resulting defect opens not into the free abdominal cavity, but into the organ adjacent to the stomach. The wall of the adjacent organ becomes the bottom of the penetrating ulcer. Aggressive gastric juice, containing hydrochloric acid and proteolytic enzymes, begins to gradually dissolve the organ wall.
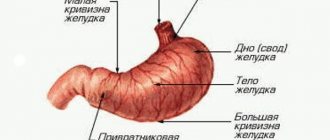
The organs into which the ulcer penetrates are determined by its location in the stomach. Most often, penetration occurs in the pancreas, followed by the frequency of lesions: the liver, lesser omentum, hepatoduodenal ligament, gall bladder, and the walls of the small and large intestines.
Causes
The main cause of ulcer penetration is considered to be the progression of ulcer formation with penetrating inflammation. In other words, if gastritis or gastroduodenitis is not treated in a timely manner, ulcers will form on the walls of the stomach, which will subsequently spread to neighboring organs.
Penetration of an ulcer can be caused by the following phenomena:
- ineffective therapy. Progression can be caused by the disease's resistance to treatment, incorrect medical tactics, irregular use of prescribed medications, or refusal to undergo surgery. With Helicobacter pylori infection, ulcer penetration is caused by immunodeficiency;
- immobility of the adjacent organ. When a parenchymal or hollow organ is tightly adjacent to the wall of the stomach and duodenum, a condition is created for peritoneal fusion. For this reason, penetration of an ulcer localized on the posterior wall of the stomach and duodenum often occurs, which is less displaced by breathing and filling with chyme;
- callous ulcerative formation, characterized by the absence of signs of regeneration and the presence of necrosis on the gastric walls;
- excessive production of hydrochloric acid, which is provoked by poor diet and non-compliance with doctor’s recommendations. The aggressive action of hydrochloric acid helps to increase the area of the inflammatory process. As a result, the walls of the organ are deeply affected, and a penetrating ulcer is formed;
- adhesive process caused by injury, inflammation occurring in the abdominal area or surgery;
- areas of erosive damage larger than 1.5 cm.
Since the penetration of the ulcer is caused by the progression of peptic ulcer, this condition is provoked by the following factors:
- Improper and irregular nutrition.
- Bad habits (smoking and alcohol).
- Stress.
- Taking certain medications.
- Overwork.
- Inadequate sleep.
Stages of development
There are 4 stages of development of ulcer penetration:
- At this stage, the development of superficial erosive lesions of the walls of the gastrointestinal tract begins, which is further complicated by the formation of an inflammatory focus. In addition, there is a partial adhesion of the stomach to the adjacent organ.
- Characterized by the destruction of layers of the gastric walls. The defective process has not yet gone beyond the main lesion, the ulcerative formation has not yet penetrated the neighboring organ.
- There is a spread of the ulcerative defect to a neighboring organ, on the surface of which a wound is formed. Deformation of the affected organ occurs, tissues become sclerotic and thicken. The stomach is also deformed by fibrous cords.
- The last stage is characterized by the formation of cavities in the area of penetration, in which the development of focal inflammation is observed. Over time, a deep ulcerative lesion forms with surrounding tumor.
Stages
At the first stage, superficial erosion of the organ wall begins. A focus of inflammation forms around. From the outside, the adjacent organ is soldered to the stomach.
In the second stage , all layers of the stomach are destroyed, but the pathological process does not yet go beyond the organ. There is no penetration of the ulcer into the neighboring organ.
In the third stage , the ulcer spreads to the adjacent organ, and a surface defect forms on its wall. The structure of the organ changes, the tissues become sclerotic and thicken. Fibrous cords tighten the stomach - it becomes deformed.
In the fourth stage, deep cavities with foci of inflammation in the surrounding tissues are formed in the penetrated organ.
Symptoms
When an ulcer penetrates, the symptoms depend on the degree of pathology and which organ the pathological process has penetrated. This complication of a stomach ulcer can be determined by the changed characteristics of pain:
- intense pain syndrome does not depend on food intake;
- pain radiates to the back, shoulder, pain can be girdling;
- Antacids and painkillers do not relieve pain. Vomiting also does not bring relief.
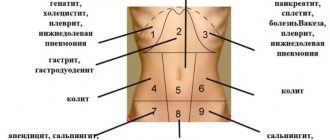
The manifestations of the clinical picture depend on which organs are involved in the pathological process:
| Organ | Symptoms |
| Pancreas |
|
| Small seal |
|
| Liver | The symptoms are identical to penetration into the lesser omentum. In addition, there are:
|
| Colon | An opening appears that connects the intestines to the stomach. This leads to feces entering the stomach and undigested food into the intestines. Symptoms other than pain are:
|
| Small intestine or biliary tract area |
|
| Aperture zone | Severe pain in the sternum, similar to heart pain |
| Retroperitoneal space | A purulent-septic process develops with intoxication and the following symptoms:
|
Dictionary
Penetration of stomach ulcer
- This is the penetration and spread of an ulcer beyond the wall of the stomach or duodenum into nearby organs and tissues.
The ulcer gradually deepens, reaches the outer lining of the stomach and penetrates the tissue that is adjacent to the wall of the stomach or duodenum. Ulcers of the body of the stomach penetrate into the lesser omentum or body of the pancreas. Ulcers of the posterior wall of the duodenal bulb penetrate the head of the pancreas, the liver or bile ducts, and the ligament between the liver and stomach. Sometimes such ulcers penetrate into the colon or mesentery of the colon. Penetration of the ulcer develops gradually and is quite difficult to detect. The patient is experiencing pain in the upper abdomen. The nature of the pain is constant, and no connection with food intake or time of day can be identified. Unlike pain from a simple stomach or duodenal ulcer, taking antacids does not reduce pain. Often the pain begins to radiate to the organ into which the ulcer penetrates. When penetrating into the pancreas, pain occurs in the back or lower back and may have a girdling character. Occasionally, such pain intensifies after eating and at night. If the ulcer penetrates the lesser omentum, pain develops under the right costal arch or radiates to the collarbone, right shoulder, or neck. Sometimes pain radiating to the heart area can be difficult to distinguish from an attack of angina. This occurs especially often when ulcers located in the upper parts of the stomach penetrate. When the ulcer penetrates into the mesentery of the colon, the pain radiates to the navel area. When palpating the abdomen, it is sometimes possible to detect limited pain in the area of penetration and even compaction of the tissue around it (infiltrate). The diagnosis of penetrating ulcers is made using fibrogastroduodenoscopy. The diagnosis is clarified using laparoscopy. Treatment of penetrating ulcers is usually surgical. Postoperative rehabilitation is indicated in sanatoriums with a medical profile: treatment of the digestive system (sanatoriums: "Krainka" (Tula region), "Krasnaya Glinka" (Samara region), "Krasnozersky" (Novosibirsk region), "Krasnoyarsk Zagorye" (Krasnoyarsk region), " Crystal" (Kemerovo region), "Marcial Waters" (Karelia), "Mashuk" (Stavropol Territory), "Lake Medvezhye" (Kurgan Region), "Lake Shira" (Khakassia), "Oktyabrsky" (Krasnodar Territory) and many others health resorts of the Russian Federation. In some resorts of Russia, included in the “List of Unique Resorts of Russia” one of the leading medical profiles: treatment of diseases of the digestive system. These are the resorts of Essentuki, Pyatigorsk, Zheleznovodsk and Kislovodsk (Caucasian Mineral Waters), Sestroretsky resort (St. Petersburg) , Shmakovka (Primorsky Territory), Belokurikha resort (Altai Territory).
Diagnostics
When making a diagnosis, ulcer penetration must be differentiated from ulcer perforation and acute pancreatitis. The most informative are the following laboratory and instrumental studies:
- Coprogram. Using microscopic analysis of stool, differential diagnosis with other gastrointestinal diseases is carried out. The Gregersen reaction is prescribed to determine occult blood in the stool. In addition, an additional study is carried out to determine the level of fecal elastase.
- EGDS. An endoscopic method that allows visualization of the mucous membrane in the initial parts of the gastrointestinal tract. Upon penetration, a deep round niche is revealed, with clear contours, the tissue around without infiltration. Additionally, endoscopic biopsy is performed.
- Laparoscopy. Allows you to determine the location of the pathological defect.
- X-ray examination with contrast. Helps determine the main manifestations of penetration: the contrast agent flows outside the organ, three-layer shadows, changes in the contours of the stomach and duodenum are observed.
- Histological examination. Tissue examination for cytomorphology is carried out in order to exclude malignant neoplasm. In case of ulcerative gastrointestinal tract, inflammatory infiltration is detected in biopsy specimens. In this case, the cells have a normal structure, pathological mitoses are not observed.
- General blood analysis. The number of leukocytes and the ESR value are determined.
- Blood chemistry. Detects hypoproteinemia, hypergammaglobulinemia, increased concentration of acute phase indicators.
- Ultrasound. It excludes or confirms the involvement of neighboring organs in the process.
Treatment
When diagnosing penetration of an ulcer, surgery is recommended in most cases. Before surgery, an intensive course of therapy is prescribed, including:
- elimination of foci of inflammation;
- antiulcer therapy;
- correction of homeostasis disorders.
Surgical intervention for penetration of an ulcer has great risks for the patient’s health, since with such an operation up to 2/3 of the stomach is subject to resection.
At stages I and II of erosive formations, ulcer penetration is treated in a hospital using conservative methods. According to the clinical recommendations of the Russian Gastroenterological Association for the diagnosis and treatment of ulcers, drug treatment consists of:
- Drugs that normalize the motor functions of the gastrointestinal tract.
- Antacids.
- Preparations with a regenerating effect.
- Dietary nutrition, the purpose of which is to eliminate the aggressive effects of irritating factors on the affected area.
A stage III penetrating defect can only be eliminated by surgery. In some cases, surgery is recommended for patients with an initial stage of pathology that is not amenable to drug treatment.
The most effective methods of surgical intervention:
- when a gastric ulcer penetrates, a distal resection is performed, in which 1/2 or 2/3 of the organ is removed. At the initial stages of pathology, for small ulcerative defects, wedge-shaped resection is performed;
- with penetration of a duodenal ulcer:
- with minor damage, duodenoplasty and selective proximal vagotomy are performed;
- for large pyloroduodenal ulcers, anthrumectomy and truncal vagotomy are performed.
In the period after surgery, anti-inflammatory treatment is prescribed, which accelerates the scarring of defects that have arisen in the affected organ. If the penetration of the ulcer is complicated by internal fistulas, in order to eliminate the fistulous tract, the stomach, duodenum, biliary tract, colon and other organs are simultaneously operated on.
Treatment of penetrating ulcers
Penetrating ulcers of stages 1-2 do not respond well to conservative treatment.
In the third and fourth stages of penetration, the ulcers do not heal. The only radical treatment for penetrating ulcers is surgery. Patients with penetrating ulcers of types 1 and 2 according to Johnson are advised to undergo gastric resection. At the first stage of penetration of small ulcers of the pyloric part of the stomach and duodenum, it is possible to perform vagotomies in combination with drainage of the stomach. The same type of operation is acceptable in the presence of huge inflammatory infiltrates in the abdominal cavity, the separation of which is dangerous due to possible damage to the organs and tissues that form it. The article was prepared and edited by: surgeon I.B. Pigovich.
Video:
Healthy:
Related articles:
- Symptoms of cancer from an ulcer Symptoms of cancer from an ulcer are not specific. Malignancy of a gastric ulcer occurs most often...
- Malignization of an ulcer Malignization of an ulcer is the transformation of an ulcer into cancer, which occurs in 5-15% of all ulcers….
- Penetrating ulcer is a surgical complication of peptic ulcer Penetration of ulcers is a surgical complication of peptic ulcer and an intermediate state between a long-term non-healing ulcer and…
- Gastric ulcer - symptoms and diagnosis Gastric ulcer is 5 times less common than duodenal ulcer. Gastric ulcers are mainly...
- Perforation of an ulcer Perforation of an ulcer is a breakthrough of an ulcer into the free abdominal cavity, into the retroperitoneal space or into ...
- Surgical treatment of ulcers Indications for the use of surgery for ulcers are divided into absolute, relative...
Prognosis and prevention
The prognosis of ulcer penetration depends on the degree of germination and timeliness of treatment. The first stage of the pathology has a relatively favorable prognosis; at stages II and III, severe complications can occur. To prevent the progression of the pathological process, timely and comprehensive treatment of ulcers and duodenal ulcers is necessary, as well as regular medical examinations for patients who have undergone ulcer surgery.
To prevent complications, you must adhere to certain rules:
- Follow a strict diet. In case of gastrointestinal ulcers, dietary table No. 1 is prescribed. You should exclude foods that cause increased secretion of gastric juice (smoked, hot, spicy foods, coffee and strong tea, canned food, etc.).
- Follow a healthy regular diet: eat 5-6 times a day in small portions at intervals of 3 hours.
- Completely eliminate smoking and alcohol. Nicotine and alcohol-containing drinks affect the formation of ulcers, rapidly developing complications and malignancy (degeneration of a peptic ulcer into oncology).
- A number of medications have an ulcerogenic effect. The development and progression of ulcers can be caused by aspirin, indomethacin, caffeine, etc. It is not recommended to take medications without a doctor's prescription.
Complications
When an ulcer penetrates, aggressive or infected contents enter the involved organ, which in half of the cases contributes to the development of the pathological process:
- if the gallbladder is affected, an acute form of cholecystitis may occur;
- when the pancreatic parenchyma is damaged, the exocrine functions of the organ and the process of food digestion are disrupted. It causes:
- steatorrhea (excessive fat content in stool);
- lientorrhea (the presence of undigested food in the stool);
- weight loss;
- very rarely perivisceritis develops (adhesions);
- disturbances of immune processes cause generalization of inflammation. Toxins and pathogenic microorganisms enter the bloodstream from the digestive system, which causes the development of sepsis;
- if penetration is combined with perforation, the entry of stomach or intestinal contents into the abdominal cavity can cause the development of diffuse or limited peritonitis;
- When the liver is damaged, fatty degeneration and infiltrative hepatitis develop.
List of references: https://chaika.com/what-do-we-treat/diseases/iazvennaia-bolezn https://www.10gkb.by/informatsiya/stati/oslozhneniya-yazvennoj-bolezni-zheludka-i-dvenadtsatiperstnoj- kishki https://www.irgups.ru/sites/default/files/mkzht/uchebnoe_posobie_yab.pdf https://medportal.ru/enc/gastroenterology/ulcer/4/ dr-kruglov.ru/konsultatsii/penetratsiya/ Author’s notes articles based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/17/2020